- Department of Orthopedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan.
Correspondence Address:
Kei Ando, Department of Orthopedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan.
DOI:10.25259/SNI_14_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naoki Segi, Kei Ando, Hiroaki Nakashima, Masaaki Machino, Sadayuki Ito, Hiroyuki Koshimizu, Hiroyuki Tomita, Shiro Imagama. Thoracic myelopathy due to ossification of the posterior longitudinal ligament shown on dynamic MR. 11-Feb-2022;13:51
How to cite this URL: Naoki Segi, Kei Ando, Hiroaki Nakashima, Masaaki Machino, Sadayuki Ito, Hiroyuki Koshimizu, Hiroyuki Tomita, Shiro Imagama. Thoracic myelopathy due to ossification of the posterior longitudinal ligament shown on dynamic MR. 11-Feb-2022;13:51. Available from: https://surgicalneurologyint.com/surgicalint-articles/11380/
Abstract
Background: Magnetic resonance (MR) and computed tomography (CT) studies combined are the optimal studies for diagnosing thoracic ossification of the posterior longitudinal ligament (OPLL) contributing to myelopathy. Here, we report a 71-year-old female, whose additional dynamic thoracic MR demonstrated transient T6–T9 anterior OPLL with cord compression.
Case Description: A 71-year-old female presented with a progressive myelopathy originally attributed to cervical cord compression resulting in a cervical laminoplasty. However, when she failed to improve postoperatively, a dynamic thoracic MR was performed. On the flexion study, it demonstrated significant although transient T6–T9 anterior thoracic cord compression due to both OPLL and kyphosis. The patient’s symptoms resolved following a posterior thoracic fusion alone (i.e., no decompression was warranted).
Conclusion: Dynamic MR studies (i.e., flexion studies) in addition to the routine MR and CT evaluations should be performed for patients with myelopathy attributed to thoracic OPLL/kyphosis.
Keywords: Dynamic magnetic resonance imaging, Ossification of the posterior longitudinal ligament, Posterior fusion with dekyphosis
INTRODUCTION
Dynamic factors can significantly contribute to the onset/severity of a progressive myelopathy attributed to cervical or thoracic ossification of the posterior longitudinal ligament (OPLL) with kyphosis.[
CASE REPORT
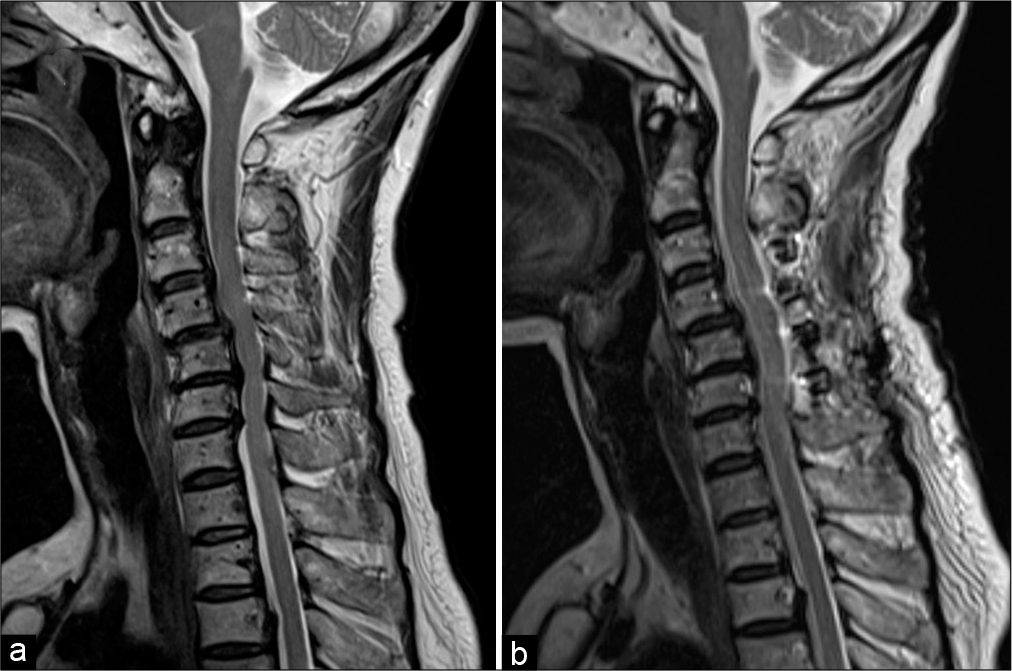
A 71-year-old female presented with a progressive paraparesis of 3 months’ duration. The cervical and thoracic computed tomography (CT)/MR scans revealed OPLL at the C4–6 (i.e., with stenosis) and T2–T8 levels [
Figure 1:
Images before the initial surgery. (a) CT sagittal image showed OPLL at T2–8 levels. (b) Ossification lesion at T7–8 level. (c) MRI sagittal image showed no suggestion of spinal cord compression. (d) MRI trans image showed no spinal cord compression but a mild flattening of the spinal cord and signal changes within the medulla. CT: Computed tomography, MRI: Magnetic resonance imaging, OPLL: Ossification of the posterior longitudinal ligament.
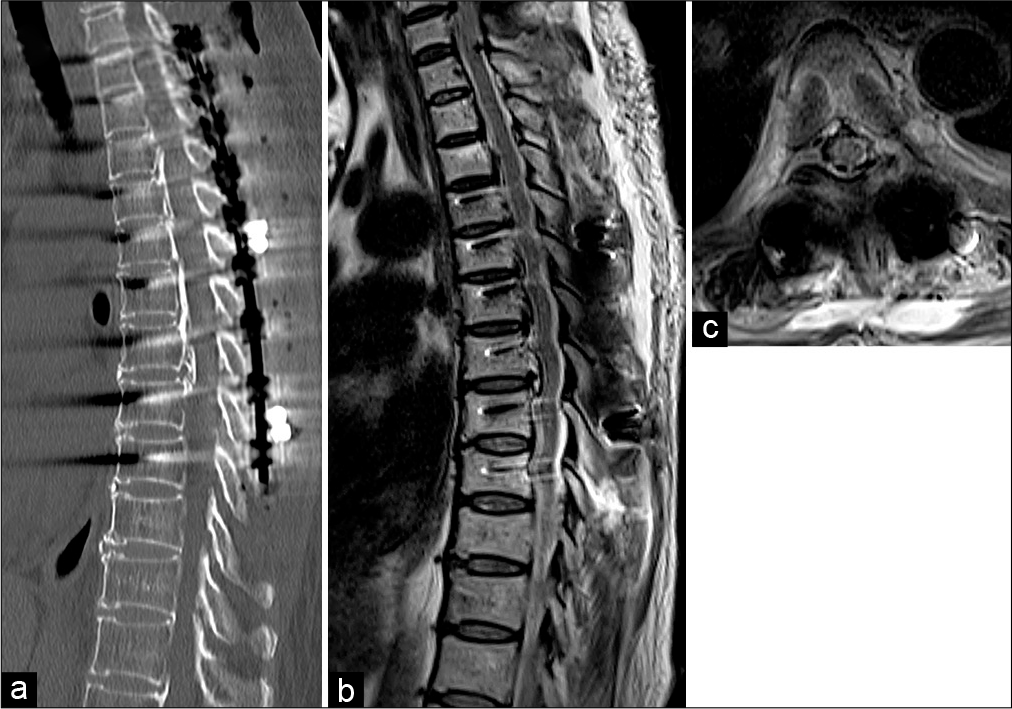
Figure 3:
Dynamic MRI images of the thoracic spine. (a and c) MRI images with backward bending showed the same findings as during routine MRI. (b and d) MRI images with forward bending revealed that the spinal cord was in close contact with the OPLL at T7–8 level and was compressed from the front. MRI: Magnetic resonance imaging, OPLL: Ossification of the posterior longitudinal ligament.
Figure 4:
Images after additional surgery. (a) CT sagittal image showed that the thoracic spine was fixed in the intermediate position. (b and c) MRI images showed that the spinal cord was not in contact with the OPLL. CT: Computed tomography, MRI: Magnetic resonance imaging; OPLL: Ossification of the posterior longitudinal ligament.
DISCUSSION
Dynamic spinal cord compression by OPLL
Thoracic OPLL lesions without a large spinal canal occupancy ratio can contribute to myelopathy best demonstrated on dynamic flexion-MR studies. Good outcomes can be achieved by fusing multiple mobile thoracic levels, even without decompression.[
CONCLUSION
A 71-year-old female first underwent a cervical C3–C6 laminoplasty for the diagnosis of cervical OPLL/stenosis. However, when her myelopathy progressed (i.e., paraparesis), both routine and dynamic thoracic MR studies documented OPLL with instability/kyphosis seen on flexion studies that warranted a posterior T1–T9 fusion without necessitating decompression.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by JSPS KAKENHI Grant Number JP 18K09025 and the General Insurance Association of Japan.
Conflicts of interest
There are no conflicts of interest.
References
1. Ando K, Kobayashi K, Machino M, Ota K, Tanaka S, Morozumi M. Connection of discontinuous segments in early functional recovery from thoracic ossification of the posterior longitudinal ligament treated with posterior instrumented surgery. J Neurosurg Spine. 2019. 32: 200-6
2. Imagama S. The essence of clinical practice guidelines for ossification of spinal ligaments, 2019: 5 Treatment of Thoracic OPLL. Spine Surg Relat Res. 2021. 5: 330-3
3. Imagama S, Ando K, Kobayashi K, Hida T, Ito K, Tsushima M. Factors for a good surgical outcome in posterior decompression and dekyphotic corrective fusion with instrumentation for thoracic ossification of the posterior longitudinal ligament: Prospective single-center study. Oper Neurosurg. 2017. 13: 661-9
4. Koda M, Furuya T, Okawa A, Aramomi M, Inada T, Kamiya K. Bone union and remodelling of the non-ossified segment in thoracic ossification of the posterior longitudinal ligament after posterior decompression and fusion surgery. Eur Spine J. 2015. 24: 2555-9
5. Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S. Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: A multicenter cohort study. Spine. 2008. 33: 2648-50