- Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
Correspondence Address:
Shu Takeuchi, Spinal Disorders Center, Fujieda Heisei Memorial Hospital, Fujieda, Japan.
DOI:10.25259/SNI_804_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shu Takeuchi, Junya Hanakita, Toshiyuki Takahashi, Ryo Kanematsu, Izumi Suda, Sho Nakamura, Manabu Minami. Thoracic synovial cyst in patient with diffuse idiopathic skeletal hyperostosis. 30-Sep-2022;13:450
How to cite this URL: Shu Takeuchi, Junya Hanakita, Toshiyuki Takahashi, Ryo Kanematsu, Izumi Suda, Sho Nakamura, Manabu Minami. Thoracic synovial cyst in patient with diffuse idiopathic skeletal hyperostosis. 30-Sep-2022;13:450. Available from: https://surgicalneurologyint.com/surgicalint-articles/11900/
Abstract
Background: Spinal synovial cysts, attributed to degenerative changes of the facet joints, commonly occur at the sites of segmental spinal instability. Here, we present a patient with diffuse idiopathic skeletal hyperostosis (DISH) who developed a T10/T11 synovial cyst contributing to myelopathy that resolved following surgical cyst excision.
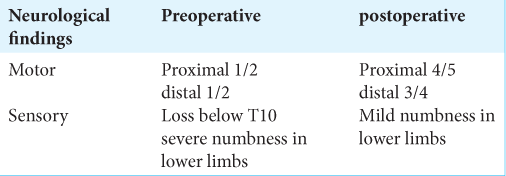
Case Description: A 69-year-old male presented with progressive numbness and paraparesis for 2-month duration. The thoracic MR spine showed synovial cyst at the T10/T11 level, while the computed tomography confirmed DISH fusion between the T4 and T10 levels. Following a laminectomy with cyst excision, the patient’s symptoms resolved and he sustained no recurrent dynamic instability.
Conclusion: A patient with DISH presented with the new onset of myelopathy attributed to a T10/T11 thoracic synovial cyst; following cyst excision, the patient’s myelopahty resolved.
Keywords: Diffuse idiopathic skeletal hyperostosis, Instability, Synovial cyst, Thoracic spine
INTRODUCTION
Synovial cysts of the spine may be simple fluid-filled sacs or thick, fibrinous, touch, and tenacious lesions arising from the facet joints. They rarely occur in thoracic spine (i.e., 1.6% incidence reported).[
CASE DESCRIPTION
History and imaging findings
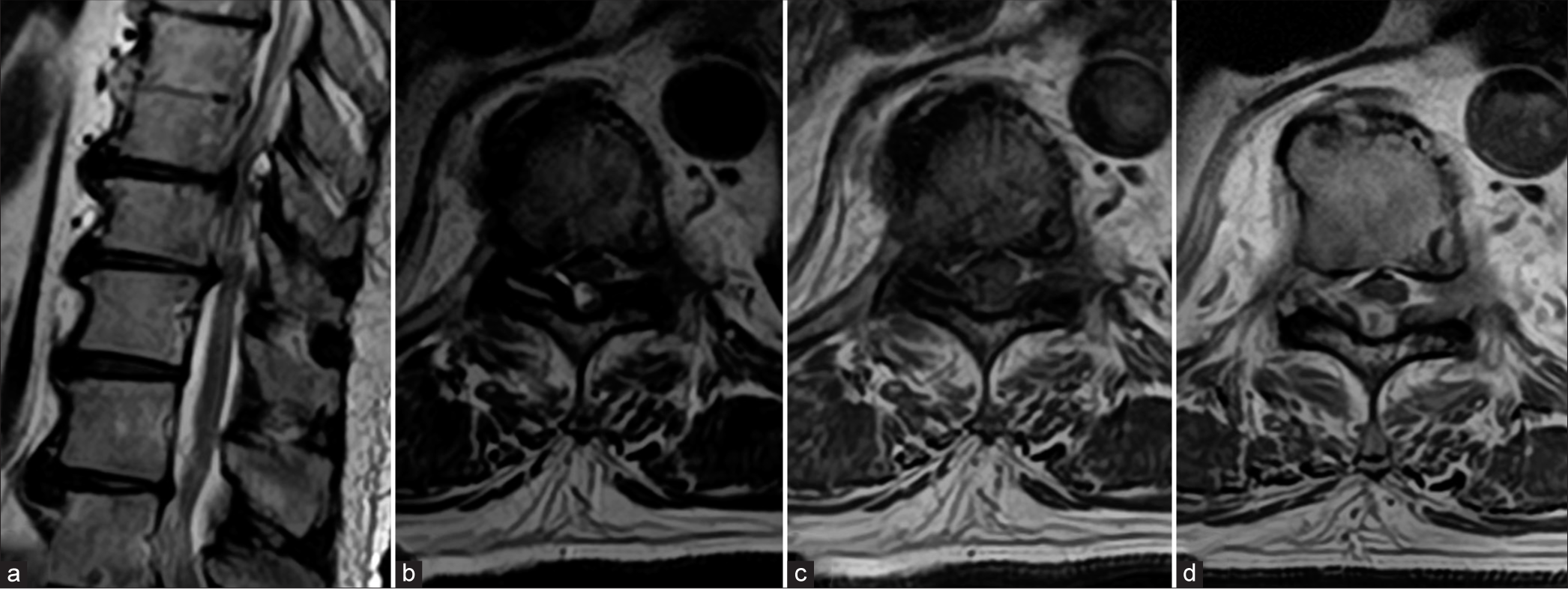
A 69-year-old male patient presented with a progressive paraparesis of 2-month duration. On presentation, he showed predominantly a right paraparesis, brisk patellar tendon reflexes, diminished sensation in the lower limbs to both pinprick and vibration, and a spinal sensory level at T10 but intact sphincter function. The thoracic MR showed central canal stenosis through the T10–12 levels and a dorsal extradural cyst at the T10/11 level that enhanced with contrast and contributed to cord compression [
Figure 1:
Magnetic resonance imaging (MRI) of the thoracic spine. (a) Sagittal T2-weighted image shows central canal stenosis at Th10/11, Th11/12. (b) Axial T2-weighted image reveal dorsal extradural cystic lesion and fluid within the right facet joint at Th10/11. (c) Axial T1-weighted image shows dorsal hypointense lesion. (d) Gadolinium-enhanced T1-weighted MRI showed peripherally enhancing mass in the extradural space.
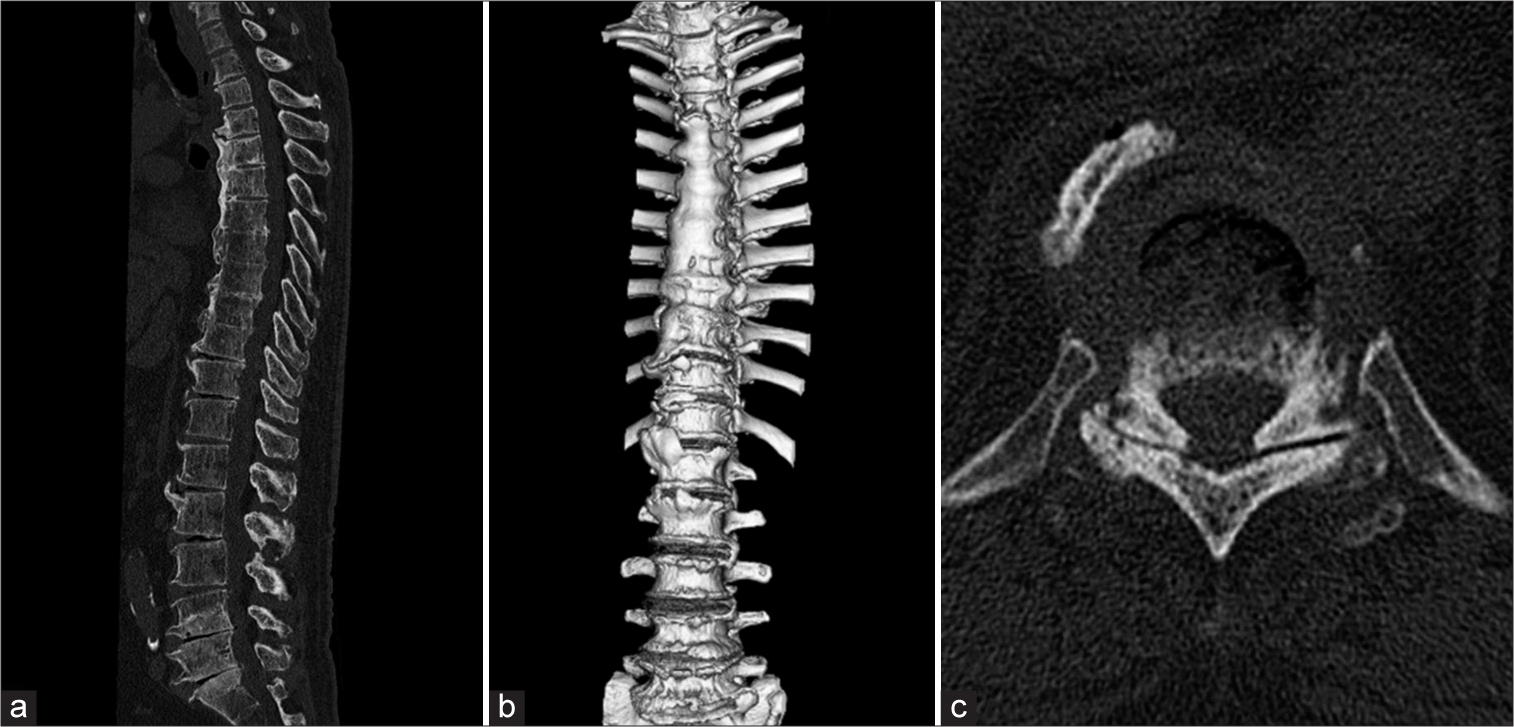
Figure 2:
Computed tomography scan images of the whole spine. (a) Sagittal view shows horizontally oriented ossification of anterior longitudinal ligament in thoracic spine and gas-containing disc at multiple levels. (b) 3D reconstruction image reveals bridging of vertebral bodies from Th4 to Th10. (c) Axial image shows gas within Th10/11 facet joint.
Surgery and histology
He underwent T9·T12 partial and T10–11 total laminectomy with resection of the cystic lesion. The dorsal adherent cystic structure contiguous to the right facet was completely removed. Histopathological examination showed cystic formation with granulation tissue, calcification, inflammatory cells, and chondroid metaplasia, compatible with synovial cyst.
Postoperative course
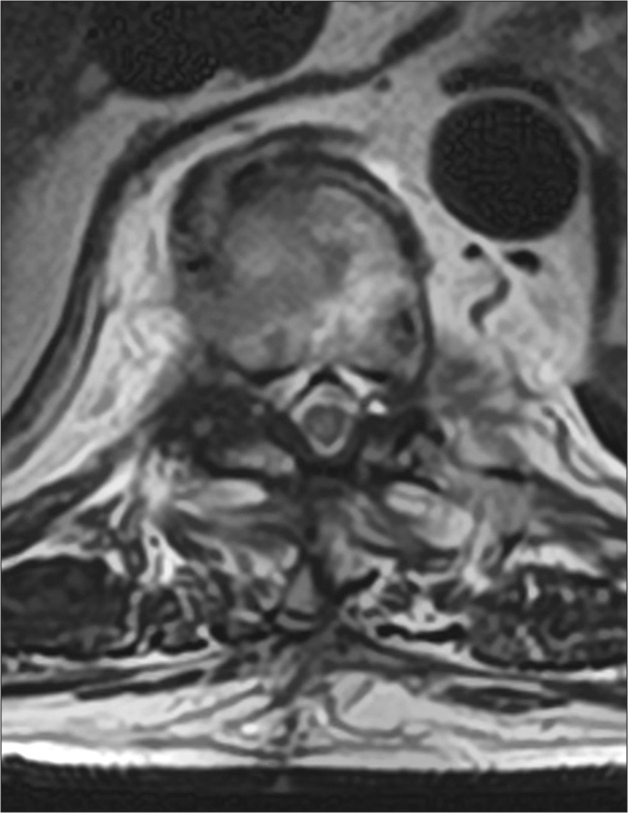
The patient sustained no perioperative/postoperative complications and the postoperative imaging studies showed decompression of spinal cord with no residual cyst [
DISCUSSION
Synovial cysts rarely occur in thoracic spine (i.e., reportedly in 1.6% of cases).[
CONCLUSION
A 69-year-old male with T4–10 DISH developed myelopathy attributed to a right-sided T10/T11 synovial cyst extrusion just below the fused thoracic vertebrae that resolved following cyst excision.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Almefty R, Arnautovic KI, Webber BL. Multilevel bilateral calcified thoracic spinal synovial cysts. J Neurosurg Spine. 2008. 8: 473-7
2. Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M. Spinal synovial cysts: Pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J. 2008. 17: 831-7
3. Bruder M, Cattani A, Gessler F, Droste C, Setzer M, Seifert V. Synovial cysts of the spine: Long-term follow-up after surgical treatment of 141 cases in a single-center series and comprehensive literature review of 2900 degenerative spinal cysts. J Neurosurg Spine. 2017. 27: 256-67
4. Cohen-Gadol AA, White JB, Lynch JJ, Miller GM, Krauss WE. Synovial cysts of the thoracic spine. J Neurosurg Spine. 2004. 1: 52-7
5. Epstein NE, Baisden J. The diagnosis and management of synovial cysts: Efficacy of surgery versus cyst aspiration. Surg Neurol Int. 2012. 3: S157-66
6. Houten JK, Sanderson SP, Cooper PR. Spontaneous regression of symptomatic lumbar synovial cysts. Report of three cases. J Neurosurg. 2003. 99: 235-8
7. Khan AM, Girardi F. Spinal lumbar synovial cysts. Diagnosis and management challenge. Eur Spine J. 2006. 15: 1176-82
8. Kusakabe T, Kasama F, Aizawa T, Sato T, Kokubun S. Face cyst in the lumbar spine: Radiological and histopathological findings and possible pathogenesis. J Neurosurg Spine. 2006. 5: 398-403
9. Maezawa Y, Baba H, Uchida K, Furusawa N, Kubota C, Yoshizawa K. Spontaneous remission of a solitary intraspinal synovial cyst of the lumbar spine. Eur Spine J. 2000. 9: 85-7
10. Nascimento FA, Gatto LA, Lages RO, Neto HM, Demartini Z, Koppe GL. Diffuse idiopathic skeletal hyperostosis: A review. Surg Neurol Int. 2014. 16: 122-5