- Department of Neurosurgery, Puerta de Hierro University Hospital, Madrid, Spain
- Department of Pathology, Puerta de Hierro University Hospital, Madrid, Spain
- Department of Neurophysiology, Puerta de Hierro University Hospital, Madrid, Spain
Correspondence Address:
Ruth Prieto
Department of Neurophysiology, Puerta de Hierro University Hospital, Madrid, Spain
DOI:10.4103/sni.sni_340_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Ruth Prieto, Eva Tejerina, Xavier Santander, Esperanza Marín. Thymoma dissemination through the thoracic intervertebral foramen: Pleural recurrence resulting in spinal cord compression. 13-Dec-2018;9:253
How to cite this URL: Ruth Prieto, Eva Tejerina, Xavier Santander, Esperanza Marín. Thymoma dissemination through the thoracic intervertebral foramen: Pleural recurrence resulting in spinal cord compression. 13-Dec-2018;9:253. Available from: http://surgicalneurologyint.com/surgicalint-articles/9138/
Abstract
Background:Spinal dissemination of thymic tumors is rare but should be considered in the differential diagnosis of thoracic dumbbell-shaped lesions and/or vertebral tumors, irrespective of the time since the initial diagnosis.
Case Description:A 63-year-old man, with a history of invasive type AB thymoma treated 21 years ago, newly presented to the hospital with a dumbbell-shaped T8-T9 lesion compressing the spinal cord. A review of the literature showed only 16 previous cases of thymic tumors with thoracic spine involvement. Here, we report the lengthiest interval between the initial tumor diagnosis and the detection of spinal involvement, that was secondary to a pleural recurrence from his thymoma. The patient did well following successful excision of the intraspinal mass which had encased the T8 nerve root.
Conclusion:Spinal dissemination of thymic tumors can occur due to vertebral metastasis or to extension of a pleural recurrence through the intervertebral foramen. Definitive treatment for spinal lesions should be considered to provide adequate cord decompression.
Keywords: Thymoma, thymic tumor, spinal cord compression, pleural recurrence, spinal metastases
INTRODUCTION
Thymomas are infrequently encountered. They are slow-growing and typically benign mediastinal tumors originating from epithelial cells of the thymus. The most aggressive tumor variant are thymic carcinomas, which are found on rare occasions.[
CASE DESCRIPTION
A 63-year-old male presented with dorsal pain of a 3 month duration. He had undergone gross-total resection of an invasive mixed AB thymoma (Masaoka-Koga II–III) 21 years ago, followed by local radiotherapy (52 Gy). After staying disease free for 12 years, he developed three pleural nodules; subsequent biopsy demonstrated pleural recurrent thymoma that was then treated with gamma knife radiosurgery (13 × 300 cGy in each lesion). The pleural lesions remained stable for the next 10 years. The patient was referred to our institution at the time radiographic spinal cord compression at T8-T9 level was discovered in addition to pleural thickening involving both hemithoraces [
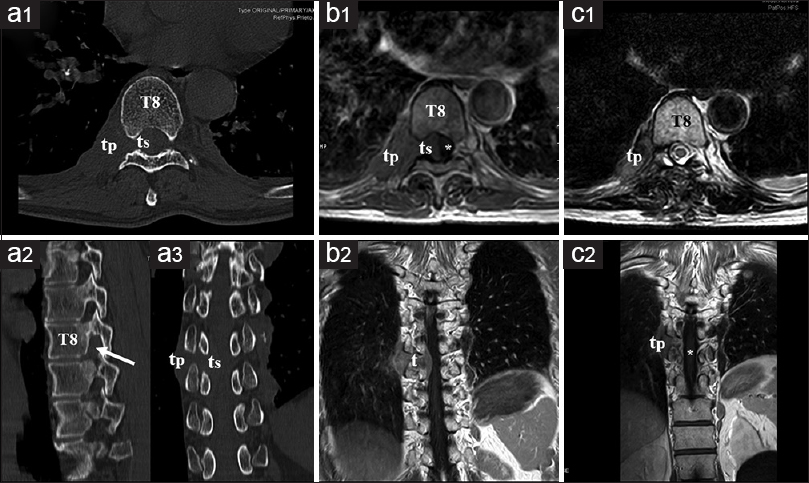
Figure 1
Preoperative and postoperative neuroradiological studies. (a) Preoperative computed tomography: axial (a1), sagittal (a2), and coronal (a3) scans showing an irregular tumor with pleural (tp) and spinal (ts) components. Note that the vertebral foramen is slightly enlarged (arrow) and the adjacent bone structures are not infiltrated. T8: Eighth thoracic vertebrae. (b) Preoperative MRI: axial (b1) and coronal (b2) MRI scans demonstrating a dumbbell-shaped mass along the course of the right eighth nerve root. The spinal cord (asterisk) is displaced to the left. (c) Postoperative MRI shows an adequate decompression of the spinal cord (asterisk) and persistence of the pleural tumor component (tp)
MR findings
The magnetic resonance imaging showed an irregular, dumbbell-shaped lesion at the T8–T9 level with an intraspinal component occupying 60% of the canal, displacing the cord toward the left [
Surgery
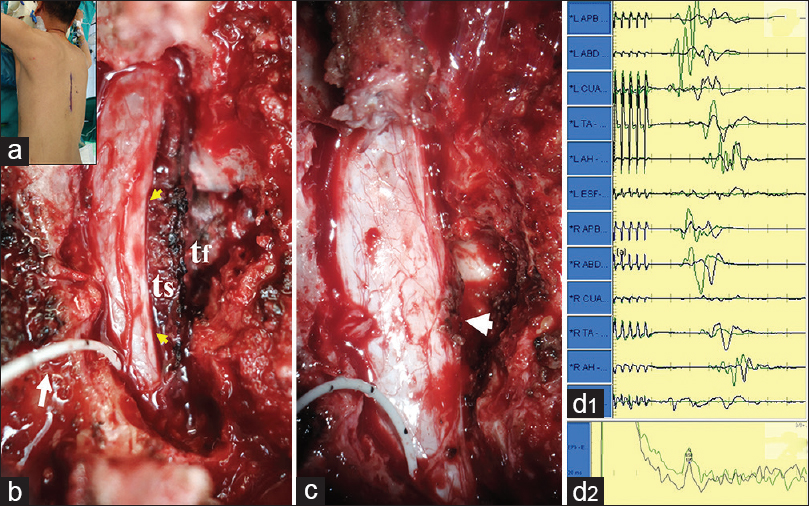
The spinal and foraminal components of the tumor were removed through a one-level laminectomy with right-sided foraminotomy and medial T8–T9 facetectomy [
Figure 2
Intraoperative photographs and neurophysiologic monitoring. (a) The patient is placed in a prone position. A vertical midline incision was made centered at the T8 level. (b) Following a one-level laminectomy and extensive foraminotomy, the intraspinal (ts) and foraminal (tf) components of the tumor were exposed. Observe the notable spinal cord compression (yellow arrows). White arrow points to the D-wave cable placed in the epidural space below the tumor. (c) The spinal cord has been decompressed. Two nonabsorbable stitches (arrowhead) were placed at the anatomical area of the T8's right exiting nerve root, where a small dural hole was found after tumor removal. Motor evoked potentials to transcranial electrical stimulation (d1) and D-wave (d2) monitoring. No changes were observed between basal recordings (green waves) and those measured at the end of tumor removal (black waves)
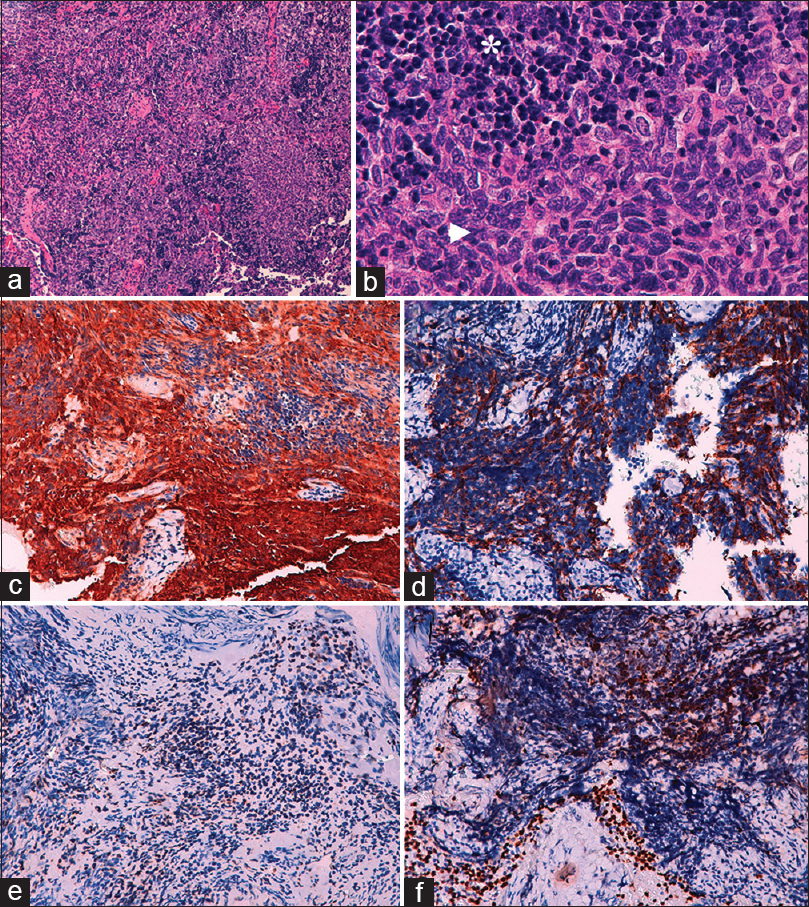
Histologic Diagnosis
The histological analysis revealed an admixture of neoplastic epithelial cells and nonneoplastic small lymphocytes. The morphological and immunostaining features of the tumor corresponded to metastatic thymoma [
Figure 3
Photomicrographs of the surgical specimen. Hematoxylin–eosinstain ((a) 10×, (b) 40×). The neoplasm consisted of a mixture of poligonal (oval) and spindle-shaped epithelial cells (arrowhead), small-to-medium sized, arranged in nests, and surrounded or intermingled with nonneoplastic small mature-appearing lymphocytes (asterisk). The epithelial cells show vesicular oval nuclei with nucleoli and pale cytoplasms. Immunohistochemistry stains (c–f): The epithelial nature of the polygonal and spindle-shaped cells was supported by their immunostaining for low- and high-molecular weight cytokeratin markers CKAE1-AE3 (c) and CK5-6 (d). The nonneoplastic, immature lymphoid population intermingled with the epithelial cells showed positivity for CD3 (e) and TdT (f)
DISCUSSION
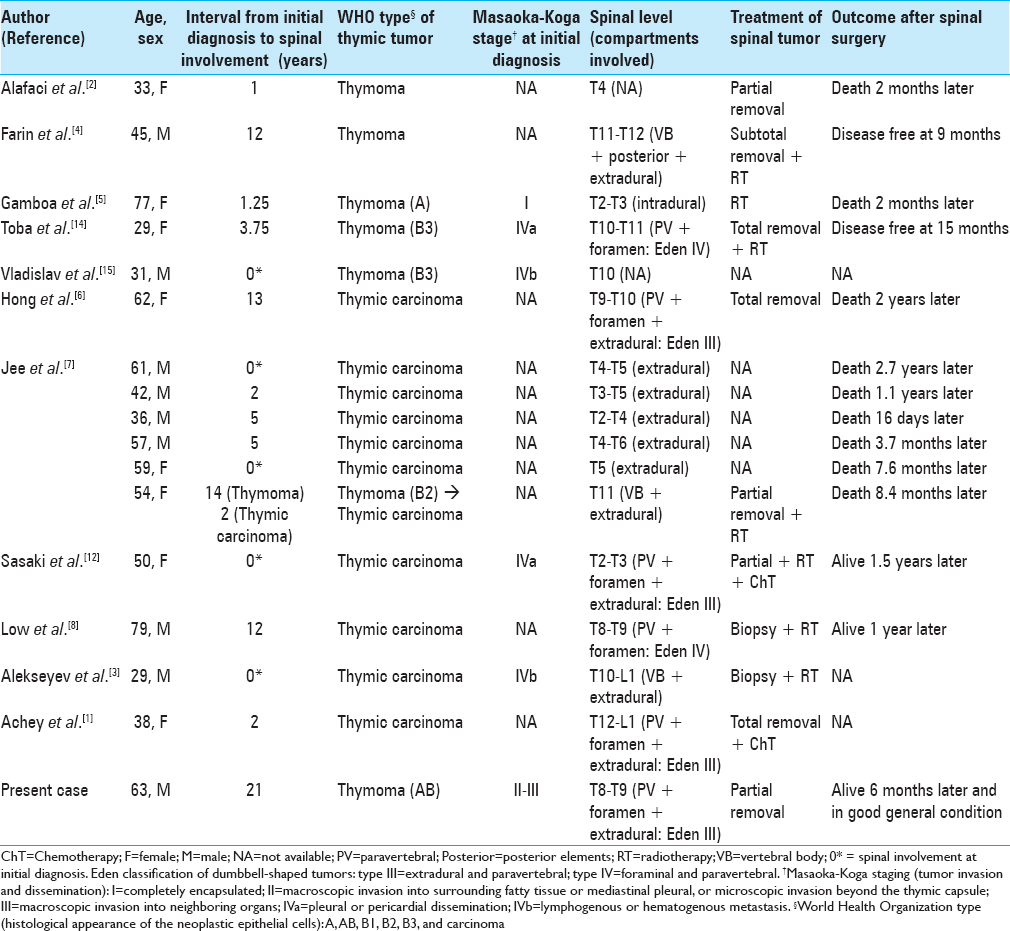
In the literature, we could only find 16 previous cases of thymic tumors involving the thoracic spine [
There is a lack of consensus regarding the optimal management of thymic tumors in advanced stages and specifically how to treat the rare cases that exhibit spinal disseminations.[
CONCLUSION
Spinal dissemination from thymic tumors is rare and should be included in the differential diagnosis of thoracic dumbbell-shaped lesions and vertebral tumors. Definitive treatment and surgery should be based on the status of the disease and the patient's clinical condition. As these are slow-growing mediastinal lesions, early decompression of the spinal cord may avoid the subsequent onset of progressive neurological dysfunction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We are grateful to George Hamilton for his critical review of the language and style of the manuscript.
References
1. Achey RL, Lee BS, Sundar S, Benzel EC, Krishnaney AA. Rare thymoma metastases to the spine: Case reports and review of the literature. World Neurosurg. 2018. 110: 423-31
2. Alafaci C, Salpietro FM, Grasso G, Passalacqua M, Lucerna S, Romano A, Tomasello F. Spinal cord compression by a metastasizing thymoma. Acta Neurochir (Wien). 1999. 141: 215-6
3. Alekseyev K, Iannicello A, Amore G, Rosenkranz T, Ross MK. Thymic carcinoma with metastasis in a young 29-year-old male causing radiculopathy. Oxf Med Case Rep. 2016. 8: 183-5
4. Farin A, Ayran HE, Abshire BB. Thymoma metastatic to the extradural spine. J Clin Neurosci. 2005. 12: 824-7
5. Gamboa EO, Sawhney V, Lanoy RS, Haller NA, Powell AT, Hazra SV. Widespread metastases after resection of noninvasive thymoma. J Clin Oncol. 2008. 26: 1752-5
6. Hong B, Nakamura M, Hartmann C, Brandis A, Ganser A, Krauss JK. Delayed distal spinal metastases in thymomas. Spine (Phila Pa 1976). 2013. 38: E1709-13
7. Jee TK, Lee SH, Kim HJ, Kim ES, Eoh W. Spinal metastasis of thymic carcinoma as a rare manifestation: A summary of 7 consecutive cases. Korean J Spine. 2014. 11: 157-61
8. Low HM, Wong CF, H'ng MW. Thymic carcinoma presenting with an unusual and delayed metastasis to the neural foramen, mimicking thoracic spinal radiculopathy. Med J Malaysia. 2016. 71: 378-69
9. Moser B, Fadel E, Fabre D, Keshavjee S, de Perrot M, Thomas P. Surgical therapy of thymictumours with pleural involvement: An ESTS thymic working group project. Eur J Cardiothoracic Surg. 2017. 52: 346-55
10. Moser B, Scharitzer M, Hacker S, Ankersmit J, Matilla JR, Lang G. Thymomas and thymic carcinomas: Prognostic factors and multimodal management. Thorac Cardiovasc Surg. 2014. 62: 153-60
11. Okada K, Yano M, Yoshino I, Okumura M, Higashiyama M, Suzuki K. Thymoma patients with pleural dissemination: Nationwide retrospective study of 136 cases in Japan. Ann Thorac Surg. 2014. 97: 1743-9
12. Sasaki S, Fukushima T, Maruyama Y, Gomi D, Kobayashi T, Sekiguchi N. Two cases of thymic carcinoma initially presenting as bone metastasis: A clinical report and the usefulness of CD5 immunohistochemistry for assessing bone lesions. Intern Med. 2015. 54: 1781-5
13. Scorsetti M, Leo F, Trama A, D'Angelillo R, Serpico D, Macerelli M. Thymoma and thymic carcinomas. Crit Rev Oncol Hematol. 2016. 99: 332-50
14. Toba H, Kondo K, Takizawa H, Tangoku A. Recurrent thymoma with a pleural dissemination invading the intervertebral foramen. Eur J Cardiothoracic Surg. 2009. 35: 917-9
15. Vladislav T, Jain RK, Alvarez R, Mehta RJ, Gökmen-Polar Y, Kesler KA. Extrathoracic metastases of thymic origin: A review of 35 cases. Mol Pathol. 2012. 25: 370-7