- Department of Neurosurgery, State University of New York Upstate Medical University, Syracuse, United States.
Correspondence Address:
Brandon Michael Wilkinson, Department of Neurosurgery, State University of New York Upstate Medical University, Syracuse, United States.
DOI:10.25259/SNI_786_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brandon Michael Wilkinson, Hanish Polavarapu, Sunnyhith Korsapati, Ali Hazama. Thymoma metastatic to the epidural thoracic spine. 03-Nov-2023;14:388
How to cite this URL: Brandon Michael Wilkinson, Hanish Polavarapu, Sunnyhith Korsapati, Ali Hazama. Thymoma metastatic to the epidural thoracic spine. 03-Nov-2023;14:388. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12623
Abstract
Background: Thymomas rarely metastasize to the spine. Here, we present a 69-year-old female diagnosed with stage IV thymoma, which subsequently developed a symptomatic epidural thoracic spinal lesion causing thoracic myelopathy.
Case Description: The patient initially presented with paraspinal rib pain, lower extremity weakness, and gait imbalance. The magnetic resonance revealed a T10 vertebral body lesion with epidural extension causing severe spinal cord compression. A T9–T10 hemilaminotomy for tumor resection was performed; this was followed by adjuvant chemotherapy and radiation. Gross total resection was achieved, and the final pathology was metastatic thymoma. Postoperatively, the patient significantly improved.
Conclusion: Metastatic thymomas to the thoracic spine are rare. For those presenting with epidural lesions causing myelopathy, surgical resection is beneficial and may be accompanied by adjunctive radiation and chemotherapy.
Keywords: Epidural, Hemilaminotomy, Myelopathy, Thoracic, Thymoma
INTRODUCTION
Thymoma accounts for approximately 0.2–1.5% of all adult malignancies (incidence of 0.13/100,000[
CASE PRESENTATION
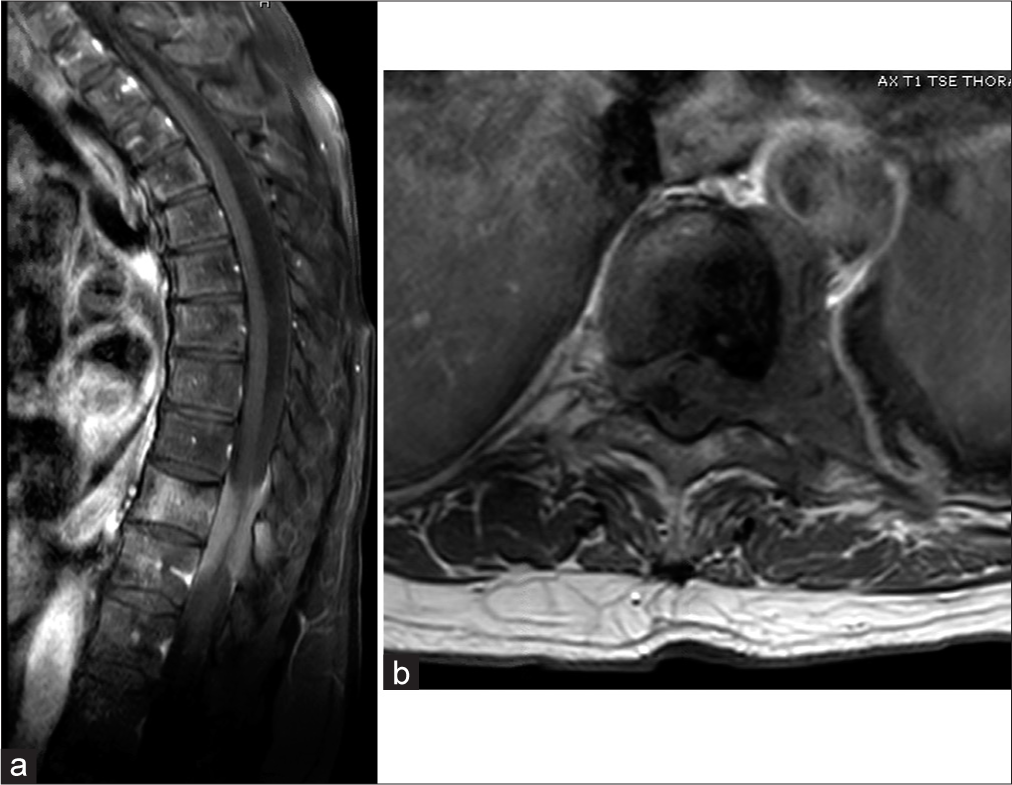
A 69-year-old female patient diagnosed with stage IV thymoma in 2021 previously treated with chemotherapy and radiation presented with progressive worsening mid-back pain, gait imbalance, and lower extremity weakness. The initial magnetic resonance revealed a T10 vertebral body lesion with epidural extension causing spinal cord compression [
Figure 1:
(a) Sagittal T1-weighted magnetic resonance imaging (MRI) with contrast demonstrating a homogeneously enhancing lesion in the T10 vertebral body with ventral and dorsal epidural extension causing severe spinal cord compression. (b) Axial T1-weighted MRI with contrast demonstrating a predominantly left-eccentric epidural lesion causing rightward displacement of the spinal cord. Of note the left T10 nerve root appears completely enveloped in the tumor.
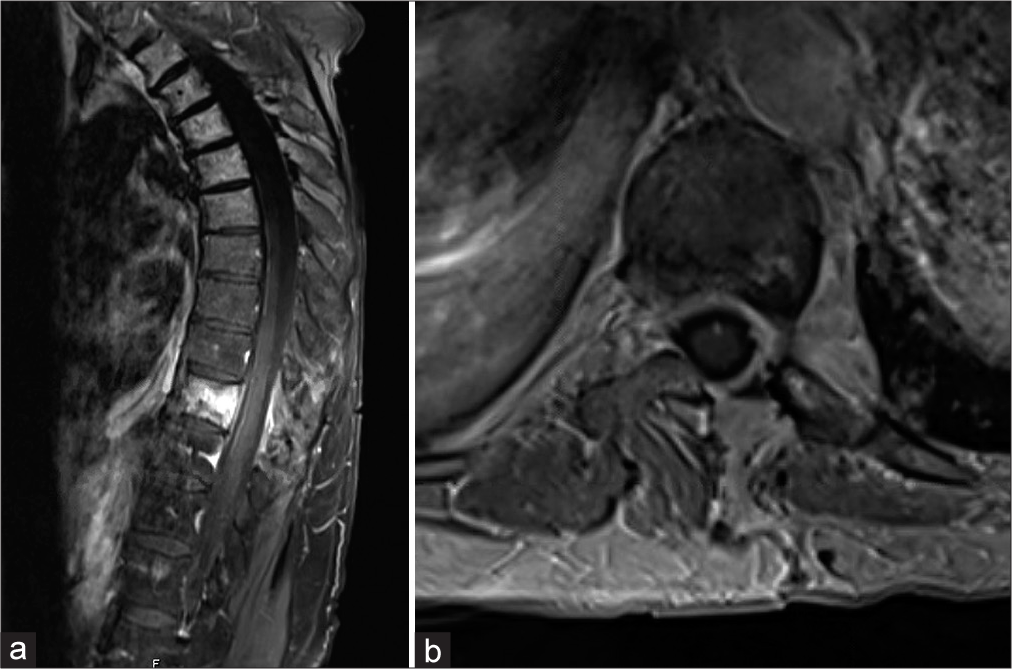
In August 2022, the patient underwent T9 and T10 left hemilaminotomy for gross total tumor resection. At surgery, the firm tumor was densely adherent to the ligamentum flavum and underlying dura; it was dissected free while the left T10 nerve root, encased by the tumor, was sacrificed. A small durotomy was encountered near the axilla of the left T9 nerve root and was repaired primarily. The frozen pathology was consistent with metastatic thymoma. Postoperatively, the patient’s myelopathy resolved within 6 postoperative months. Subsequent imaging revealed adequate decompression/removal of the epidural tumor [
Figure 2:
(a) Four-month postoperative sagittal T1-weighted magnetic resonance imaging (MRI) with contrast demonstrating good spinal cord decompression with removal of epidural tumor components. Residual enhancement is seen throughout the T10 vertebral body which was not pursued during surgery. (b) Postoperative axial T1-weighted MRI with contrast showing the hemilaminectomy defect and a well-decompressed spinal cord with normal positioning in the spinal canal.
DISCUSSION
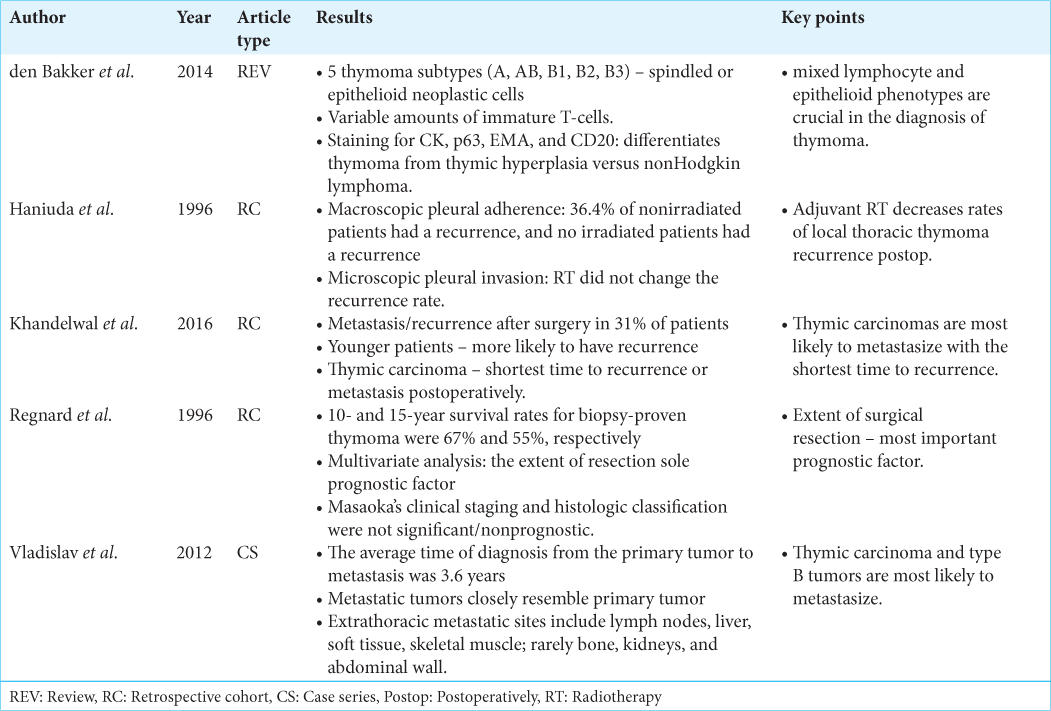
Khandelwal et al. demonstrated that thymic carcinoma had the fastest rate of metastasis with a median of 3.6 months [Reference Summary Table].[
CONCLUSION
The successful surgical management of metastatic thymomas, consisting of gross total excision, carries the best prognosis for achieving optimal outcomes. Additional postoperative adjuvant chemotherapy and radiation treatments may be utilized.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. den Bakker MA, Roden AC, Marx A, Marino M. Histologic classification of thymoma: A practical guide for routine cases. J Thorac Oncol. 2014. 9: S125-30
2. Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol. 2010. 5: S260-5
3. Haniuda M, Miyazawa M, Yoshida K, Oguchi M, Sakai F, Izuno I. Is postoperative radiotherapy for thymoma effective?. Ann Surg. 1996. 224: 219-24
4. Hwang Y, Park IK, Park S, Kim ER, Kang CH, Kim YT. Lymph node dissection in thymic malignancies: Implication of the ITMIG lymph node map, TNM stage classification, and recommendations. J Thorac Oncol. 2016. 11: 108-14
5. Khandelwal A, Sholl LM, Araki T, Ramaiya NH, Hatabu H, Nishino M. Patterns of metastasis and recurrence in thymic epithelial tumours: Longitudinal imaging review in correlation with histological subtypes. Clin Radiol. 2016. 71: 1010-7
6. Regnard JF, Magdeleinat P, Dromer C, Dulmet E, de Montpreville V, Levi JF. Prognostic factors and long-term results after thymoma resection: A series of 307 patients. J Thorac Cardiovasc Surg. 1996. 112: 376-84
7. Sung YM, Lee KS, Kim BT, Choi JY, Shim YM, Yi CA. 18F-FDG PET/CT of thymic epithelial tumors: Usefulness for distinguishing and staging tumor subgroups. J Nucl Med. 2006. 47: 1628-34
8. Vladislav T, Jain RK, Alvarez R, Mehta RJ, Gökmen-Polar Y, Kesler KA. Extrathoracic metastases of thymic origin: A review of 35 cases. Mod Pathol. 2012. 25: 370-7