- Department of Special Surgery, Faculty of Medicine, The Hashemite University, Zarqa, Jordan,
- Department of Neurosciences, Arab Hospitals Group, Ramallah, Palestinian Territory, Occupied, Jordan
- Department of Neurosurgery, Al-Kindi Hospital, Amman, Jordan
Correspondence Address:
Alaa Al-Mousa, Department of Special Surgery, Faculty of Medicine, The Hashemite University, Zarqa, Jordan.
DOI:10.25259/SNI_316_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alaa Al-Mousa1, Amjed A. Tarifi1, Anan Shtaya2, Ishaq M. Ghanem3. Transglabellar resection of frontal sinus cholesterol granuloma extending cranially through cecum foramina: Technical note. 07-Jul-2023;14:238
How to cite this URL: Alaa Al-Mousa1, Amjed A. Tarifi1, Anan Shtaya2, Ishaq M. Ghanem3. Transglabellar resection of frontal sinus cholesterol granuloma extending cranially through cecum foramina: Technical note. 07-Jul-2023;14:238. Available from: https://surgicalneurologyint.com/surgicalint-articles/12392/
Abstract
Background: Cholesterol granuloma (CG) commonly occurs in the petrous apex; their occurrence in the anterior cranial fossa CGs is rare. Subfrontal approaches are the conventional surgical approaches for the resection of midline lesions of the anterior cranial fossa and frontal sinuses. In this article, we describe a successful minimally invasive approach for resection of a small midline anterior cranial fossa CG.
Methods: We report a rare case of frontal air sinus CG extending intradurally through the foramen caecum. The surgical management of this patient involved the use of a minimally invasive transglabellar approach and a butterfly incision and the patient outcomes at 1 year after the surgery.
Results: The lesion was totally resected with no complications and the patient was discharged on the 3rd postoperative day. A 1-year follow-up scan showed neither residual nor recurrence of the lesion.
Conclusion: The transglabellar approach through a butterfly incision offers a safe approach for the resection of a lesion extending from the frontal air sinuses to the anterior cranial fossa with no complications, shorter hospital stay, and good cosmetic results.
Keywords: Anterior skull base, Butterfly incision, Cholesterol granuloma, Foramen cecum, Frontal sinus
INTRODUCTION
Cholesterol granulomas (CGs) are granulomatous reaction to cholesterol crystals. The mastoid air cells are the most common site for their occurrence. On the other hand, sino-orbital CGs are rare, but they are addressed sparsely in the literature.[
For sinus lesions with intracranial extension, subfrontal approaches are the standard of care and are associated with large scars, flaps, and craniotomies which all involve inherent risks of complications and prolonged hospital stays.[
In this article, we describe a rare case of frontal sinus CG extending intradurally through the foramen caecum and the minimally invasive approach used to treat this pathology.
MATERIALS AND METHODS
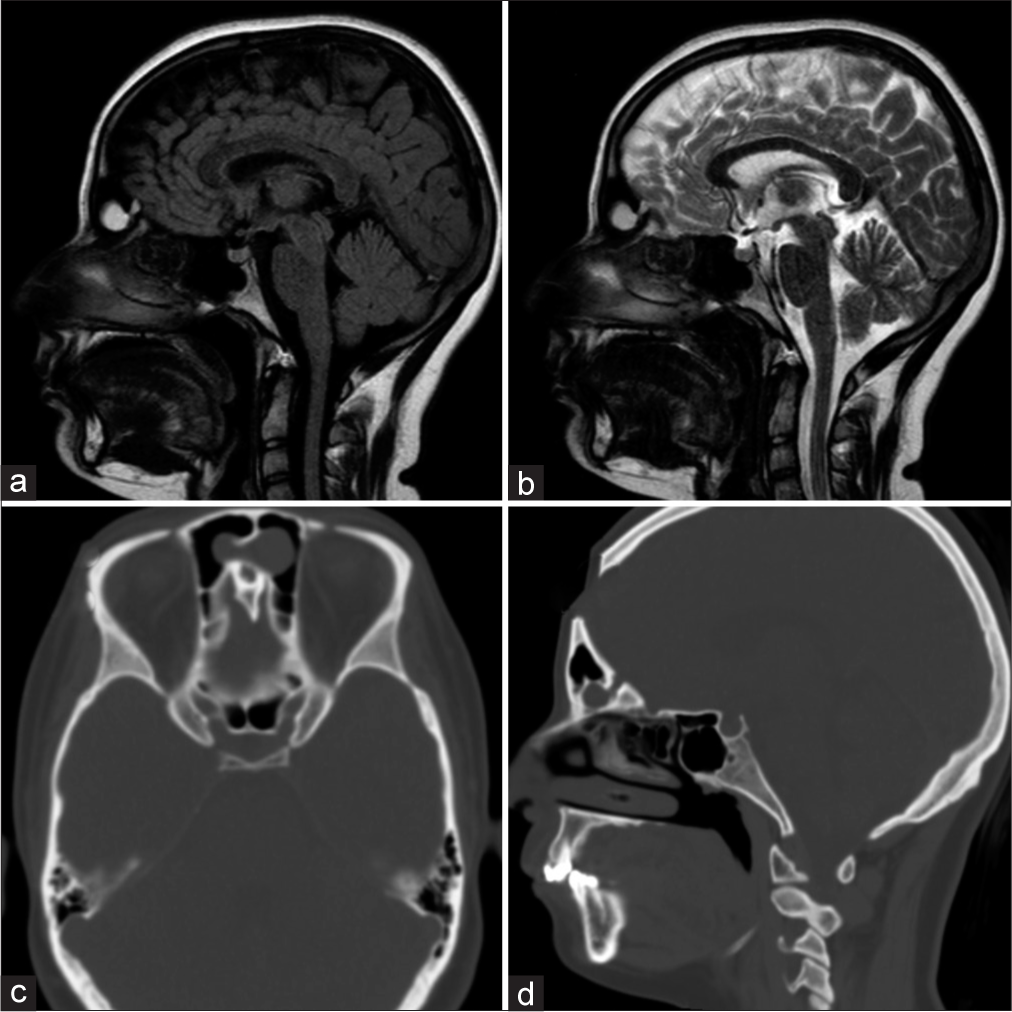
A 17-year-old female patient, previously healthy, with a frontal headache for 6 months in duration before the presentation associated with nasal congestion, underwent computed tomography sinuses which showed an isodense lesion with calcified walls within the frontal air sinuses communicating through the enlarged foramen cecum with the intracranial compartment. Her brain magnetic resonance (MR) imaging scan showed a frontal sinus lesion extending intracranially with hypertense signal on both T1 and T2 sequences [
Figure 1:
(a and b) Fluid-attenuated inversion recovery and T2-weighted sagittal magnetic resonance scan, showing hyperintense lesion within the frontal air sinus extending to the intracranial compartment (c and d) Axial and sagittal cuts computed tomography sinuses showing isodense irregular lesion within the frontal air sinus, showing extension of the lesion through the right foramen cecum.
The patient was operated on under general anesthesia in the supine position. A butterfly incision was utilized and a flap was elevated [
Under the microscope, the lesion was resected from the frontal sinus and its extension into the anterior skull base was identified. The edges of the foramen cecum were opened using a combination of a high-speed drill and a Kerrison punch. The dura was opened circumferentially around the lesion which was piercing the dura with visible arachnoid layers. After total resection, the dural edges were approximated with four stitches and a Tachosil was applied inlay followed by fascia Lata as overlay graft. A draining tube from the frontal air sinus to the nasal cavity was used and sutured [
RESULTS
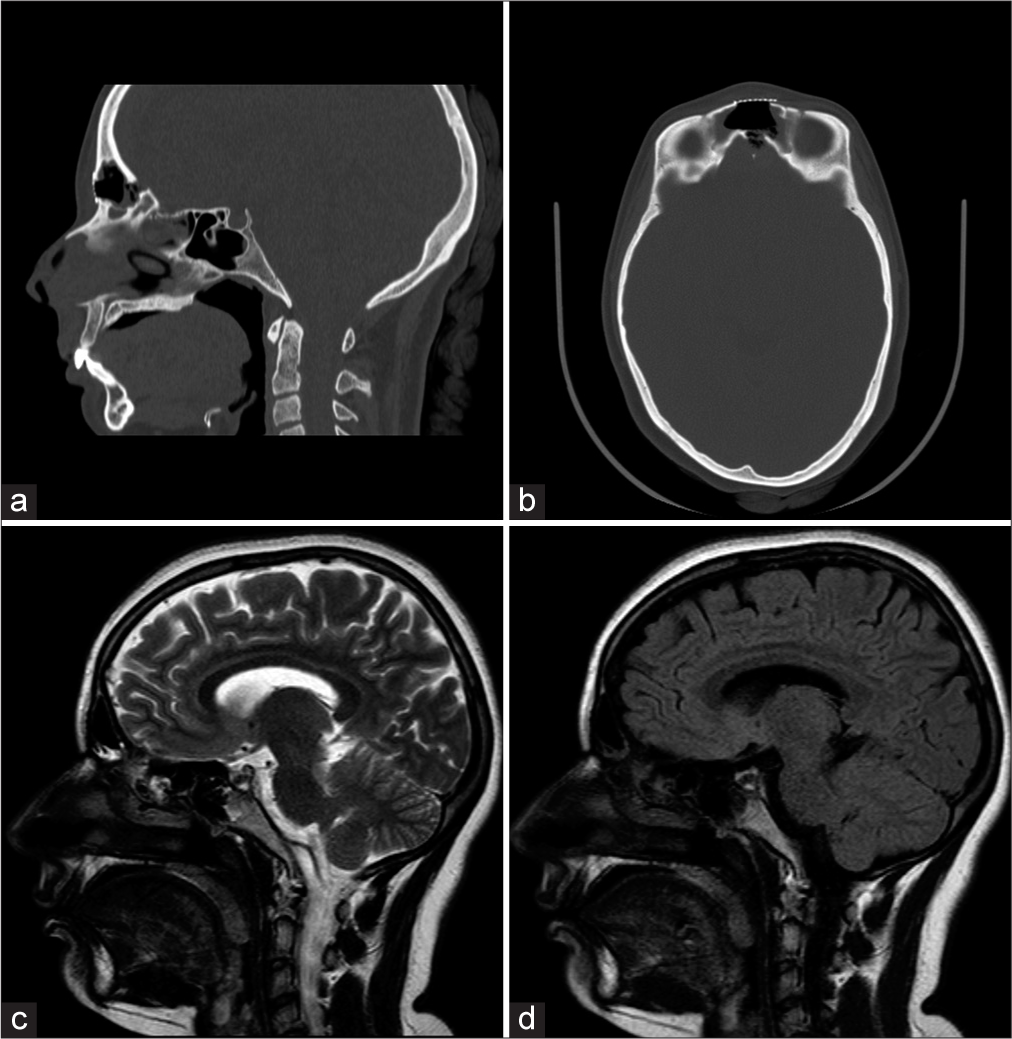
A gross total resection was achieved with no perioperative complications. The patient was discharged on the 3rd postoperative day and the draining tube was removed in outpatient clinic on the 7th postoperative day. A follow-up magnetic resonance scan 1 year later showed no evidence of recurrence [
Figure 3:
(a and b) Axial and sagittal computed tomography sinuses on the 2nd day after surgery showing widening of foramen cecum and the repair of the anterior frontal sinus wall by mesh (c and d) Sagittal T2 and fluid-attenuated inversion recovery at 1 year after surgery confirming total resection and no recurrence.
DISCUSSION
The management of anterior cranial fossa tumors is a complex and challenging task for neurosurgeons.[
Another alternative approach for such a lesion would be the extended transcribriform endoscopic endonasal approach, which allows visualization from the frontal sinus, olfactory groove, and crista galli, along the floor of the anterior fossa to the anterior planum sphenoidale.[
In selected cases, with small midline lesions, the transglabellar approach is feasible and involves making a small incision in the skin between the eyebrows in the natural skin crease.[
Our experience with this approach is limited to this case and a case of anterior cranial fossa encephalocele. In both cases, there were no complications, and the clinical and esthetic outcomes were satisfactory.
CONCLUSION
The transglabellar approach through a butterfly incision is a safe and effective technique for the resection of anterior cranial fossa tumors. It offers a direct and precise route to the tumor with minimal brain manipulation, reducing the risk of postoperative complications. Moreover, it results in good esthetic outcomes and improved patient satisfaction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abu-Ghanem S, Fliss DM. Surgical approaches to resection of anterior skull base and paranasal sinuses tumors. Balkan Med J. 2013. 30: 136-41
2. Durgam A, Batra PS. Paranasal sinus cholesterol granuloma: Systematic review of diagnostic and management aspects. Int Forum Allergy Rhinol. 2013. 3: 242-7
3. Greenfield JP, Anand VK, Kacker A, Seibert MJ, Singh A, Brown SM. Endoscopic endonasal transethmoidal transcribriform transfovea ethmoidalis approach to the anterior cranial fossa and skull base. Neurosurgery. 2010. 66: 883-92 discussion 892
4. Kellman RM, Marentette L. The transglabellar/subcranial approach to the anterior skull base: A review of 72 cases. Arch Otolaryngol Head Neck Surg. 2001. 127: 687-90
5. Kutlay M, Durmaz A, Özer İ, Kural C, Temiz Ç, Kaya S. Extended endoscopic endonasal approach to the ventral skull base lesions. Clin Neurol Neurosurg. 2018. 167: 129-40
6. Lee Y, Choi HG, Shin DH, Uhm KI, Kim SH, Kim CK. Subbrow approach as a minimally invasive reduction technique in the management of frontal sinus fractures. Arch Plast Surg. 2014. 41: 679-85
7. Montovani JC, Nogueira EA, Ferreira FD, Neto AC, Nakajima V. Surgery of frontal sinus fractures: Epidemiologic study and evaluation of techniques. Braz J Otorhinolaryngol. 2006. 72: 204-9
8. Ochiai H, Yamakawa Y, Fukushima T, Nakano S, Wakisaka S. Large cholesterol granuloma arising from the frontal sinus--case report. Neurol Med Chir (Tokyo). 2001. 41: 283-7
9. Xiao F, Shen J, Zhang L, Yang J, Weng Y, Fang Z. Unilateral subfrontal approach for giant tuberculum sellae meningioma: Single center experience and review of the literature. Front Oncol. 2021. 11: 708235