Transmastoid pediatric penetrating brain injury, interdisciplinary, and tailored patient’s treatment
- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Universitas Brawijaya/Dr. Saiful Anwar General Hospital, Malang, Indonesia
- Department Neurosurgery, Airlangga Univesity/Dr. Soetomo General Hospital, Surabaya, East Java, Indonesia.
Correspondence Address:
Tommy Alfandy Nazwar, Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Universitas Brawijaya/Dr. Saiful Anwar General Hospital, Malang, East Java, Indonesia.
DOI:10.25259/SNI_18_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tommy Alfandy Nazwar1, Farhad Bal’afif1, Donny Wisnu Wardhana1, Akmal Niam Firdaus Masyhudi2, Christin Panjaitan1. Transmastoid pediatric penetrating brain injury, interdisciplinary, and tailored patient’s treatment. 15-Mar-2024;15:85
How to cite this URL: Tommy Alfandy Nazwar1, Farhad Bal’afif1, Donny Wisnu Wardhana1, Akmal Niam Firdaus Masyhudi2, Christin Panjaitan1. Transmastoid pediatric penetrating brain injury, interdisciplinary, and tailored patient’s treatment. 15-Mar-2024;15:85. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12803
Abstract
Background: Pediatric penetrating brain injuries (PBIs) are rare but critical traumatic events, often involving foreign objects. This report will emphasize the clinical presentation, diagnosis, and treatment strategies for pediatric PBI cases.
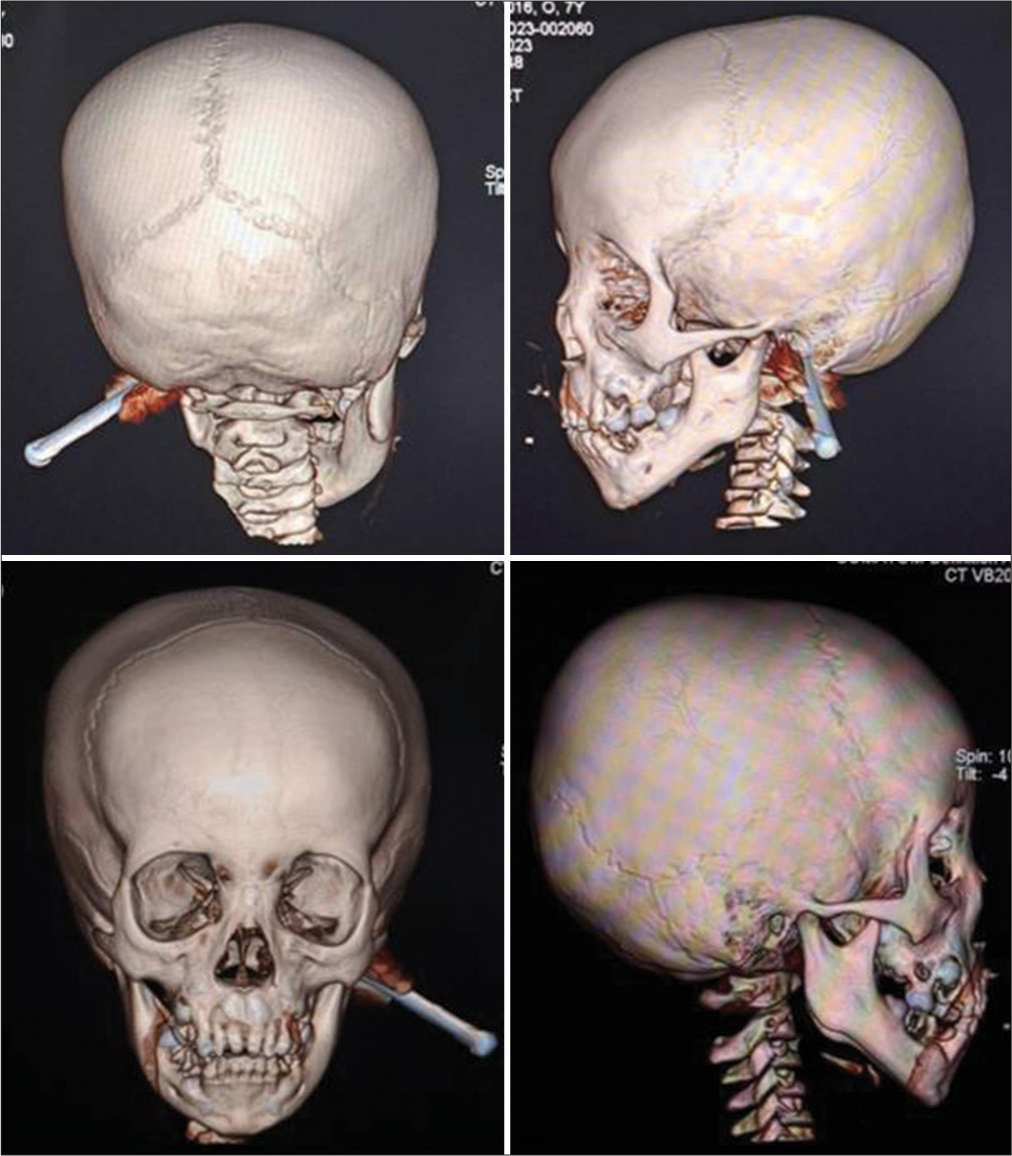
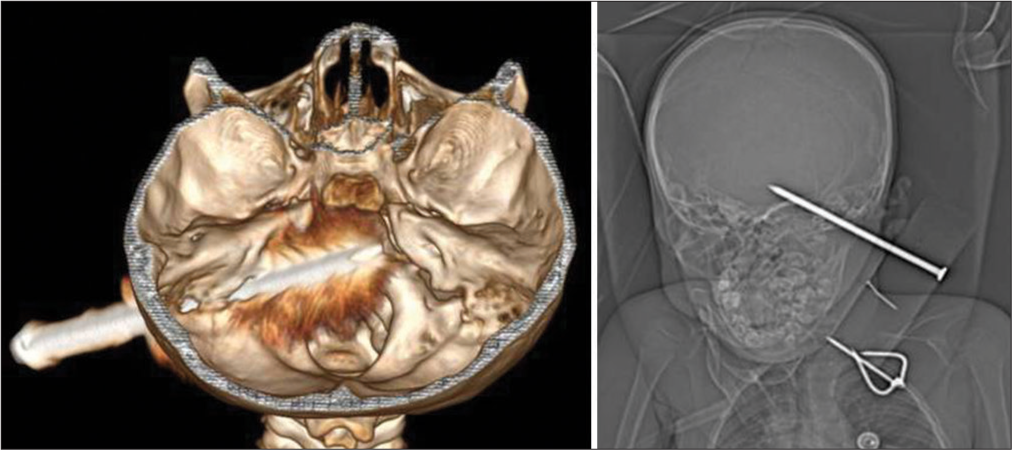
Case Description: This report presents a case of a 7-year-old male patient with a PBI resulting from a nail that penetrated the left mastoid region following a fall from a tree. On admission, the patient maintained consciousness, displayed stable vital signs, and showed no neurological deficits. Crucial radiological examinations, including skull X-rays and head computed tomography (CT) scans, revealed a 6.5 mm caliber nail penetrating 5.5 cm into the brain, with intraventricular hemorrhage filling the bilateral posterior horns of the lateral ventricles. In addition, the CT angiography (CTA) of the head provided a visual of the internal carotid arteries and the vertebrobasilar artery system, obscured by metal artifacts but showing no evidence of thrombus, aneurysm, or vascular malformation. The patient underwent an urgent mastoidectomy and retro sigmoid craniotomy to remove a foreign object, involving a multidisciplinary team. Subsequent to the intervention, the patient sustained full consciousness without neurological impairments and received intensive care.
Conclusion: Radiological tools, notably skull X-rays and head CT scans, are pivotal for the precise diagnosis of pediatric PBI. The combined mastoidectomy and retro sigmoid craniotomy approach offers a safe and efficient means of foreign body removal. Tailoring treatments to individual patient needs enhances outcomes.
Keywords: Case report, Computed tomography angiography, Foreign object, Pediatric, Penetrating brain injury
INTRODUCTION
Penetrating brain injury (PBI) in the pediatric population is a rare subset of traumatic brain injury (TBI). PBI accounts for around 0.4% of total brain injuries; despite this low incidence, it is associated with a significantly higher level of morbidity and mortality.[
CASE DESCRIPTION
A 7-year-old boy was admitted to the emergency department with a punctured nail in the left mastoid area after he fell off from a tree [
A head CT scan reveals a PBI by a foreign nail object in the left mastoid region [
During the surgical procedure, the patient was positioned in the park bench position to enhance access to the surgical site. The incision employed was a Lazy S-shaped postauricular incision, precisely aligned with the entry point of the foreign object. Initial management of the sizable wooden block necessitated meticulous handling, with its gradual removal in segments adhering to stringent sterilization protocols. Preceding patient positioning, electrical sawing was conducted to ensure sterility maintenance. Subsequent to the incision, a layered approach was adopted for mastoidectomy, systematically removing bone until visualization of the foreign object was achieved. Following nail localization, dural closure was effectuated utilizing primary closure techniques.
The absence of damage to adjacent intracranial tissues underscores the success of this surgical approach. The patient received broad-spectrum anti-tetanus and antibiotic treatment for three months. Following the operation, the patient’s recovery progressed positively, with full restoration of consciousness and no apparent neurological issues.
DISCUSSION
PBI in children poses significant clinical challenges. This condition occurs when an object penetrates through the skin and skull, causing damage to the brain tissue and intracranial blood vessels.[
Neuroimaging plays an important role in managing penetrating head injuries, helping to define an appropriate surgical strategy. Cranial computed tomography (CT) scans are the primary choice for neuroradiological evaluations in patients with penetrating head injuries.[
The management of PBI necessitates a comprehensive assessment, encompassing critical factors such as the precise site of injury, the intricate vascular architecture, the adjacent tissue relationship with the foreign body, and the inherent risks of infection and intracranial bleeding.[
In cases where foreign objects penetrate a child’s brain, potential complications can include damage to blood vessels from the object or its removal, unintentional harm to brain tissue, and the risk of c CSF.[
Although PBI has a high mortality rate, this patient had a good recovery and outcome. The collaborative, interdisciplinary approach employed throughout this case proved instrumental in optimizing the patient’s overall care journey. Drawing on various medical specialists’ expertise, this approach ensured that the patient received a comprehensive continuum of care, ultimately enhancing the prospects for a successful recovery and sustained clinical improvement.
CONCLUSION
Radiological tools, notably skull X-rays and head CT scans, are pivotal for the precise diagnosis of pediatric PBI. The combined mastoidectomy and retro sigmoid craniotomy approach offers a safe and efficient means of foreign body removal. Tailoring treatments to individual patient needs enhances outcomes.
Ethical Approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cage TA, Sanai N, Lawton MT, Auguste KI. Penetrating knife injury to the skull: A case report in pediatric neurosurgical care. Trauma (United Kingdom). 2016. 19: 302-7
2. Ferraz VR, Aguiar GB, Vitorino-Araujo JL, Badke GL, Veiga JC. Management of a low-energy penetrating brain injury caused by a nail. Case Rep Neurol. 2016. 2016: 4371367
3. Ganga A, Leary OP, Sastry RA, Asaad WF, Svokos KA, Oyelese AA. Antibiotic prophylaxis in penetrating traumatic brain injury: Analysis of a single-center series and systematic review of the literature. Acta Neurochir (Wien). 2023. 165: 303-13
4. Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011. 4: 395-402
5. Kumar R, Kumar R, Mallory GW, Jacob JT, Daniels DJ, Wetjen NM. Penetrating head injuries in children due to BB and pellet guns: A poorly recognized public health risk. J Neurosurg Pediatr. 2016. 17: 15-221
6. Marut D, Shammassian B, McKenzie C, Adamski J, Traeger J. Evaluation of prophylactic antibiotics in penetrating brain injuries at an academic level 1 trauma center. Clin Neurol Neurosurg. 2020. 193: 105777
7. Mikhael M, Frost E, Cristancho M. Perioperative care for pediatric patients with penetrating brain injury: A review. J Neurosurg Anesthesiol. 2018. 30: 290-8
8. Muballe KD, Hardcastle T, Kiratu E. Neurological findings in pediatric penetrating head injury at a university teaching hospital in Durban, South Africa: A 23-year retrospective study. J Neurosurg Pediatr. 2016. 18: 550-7
9. Samuthrat T, Ye K, Tong Y. Transoral intracranial injury via middle skull base by a blunt chopstick in a child. World Neurosurg. 2017. 103: 952.e11-7
10. Tabibkhooei A, Taheri M, Rohani S, Chanideh I, Rahatlou H. Penetrating brain injury with a metal bar and a knife: Report of two interesting cases. Neuroradiol J. 2018. 31: 203-6
11. Takahashi CE, Virmani D, Chung DY, Ong C, Cervantes-Arslanian AM. Blunt and penetrating severe traumatic brain injury. Neurol Clin. 2021. 39: 443-69
12. Vakil MT, Singh AK. A review of penetrating brain trauma: Epidemiology, pathophysiology, imaging assessment, complications, and treatment. Emerg Radiol. 2017. 24: 301-9
13. Woo X, Yap NK, Toh TH, Yiek SH. Accidental low-velocity penetrating brain injury by glass marble. Asian J Neurosurg. 2022. 17: 116-9
14. Wu R, Ye Y, Liu C, Yang C, Qin H. Management of penetrating brain injury caused by a nail gun: Three case reports and literature review. World Neurosurg. 2018. 112: 143-7
15. Wu Y, Chen TG, Chen SM, Zhou L, Yuan M, Wang L. Trans-base and trans-vault low-velocity penetrating brain injury: A retrospective comparative study of characteristics, treatment, and outcomes. Chin J Traumatol. 2021. 24: 273-9