- Department of Neurosurgery, Showa University Fujigaoka Hospital, Yokohama, Japan.
Correspondence Address:
Ryo Aiura, Department of Neurosurgery, Showa University Fujigaoka Hospital, Yokohama, Japan.
DOI:10.25259/SNI_19_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryo Aiura, Eisuke Hirose, Marina Hirato, Arisa Umesaki, Sadayoshi Nakayama, Tomoyuki Tsumoto. Traumatic arteriovenous fistula of the middle meningeal artery treated with selective coil embolization: A case report. 16-Feb-2024;15:51
How to cite this URL: Ryo Aiura, Eisuke Hirose, Marina Hirato, Arisa Umesaki, Sadayoshi Nakayama, Tomoyuki Tsumoto. Traumatic arteriovenous fistula of the middle meningeal artery treated with selective coil embolization: A case report. 16-Feb-2024;15:51. Available from: https://surgicalneurologyint.com/surgicalint-articles/12751/
Abstract
Background: Dural arteriovenous fistulas (AVFs) are reportedly induced by trauma. We report a rare case of traumatic AVF with a direct shunt from the middle meningeal artery (MMA) to the middle meningeal vein (MMV) and multiple drainage routes after head trauma. The patient was effectively treated with selective coil embolization alone without liquid embolic material.
Case Description: A 56-year-old woman was admitted to the emergency department with mild disturbance of consciousness caused by a head contusion after alcohol consumption. She exhibited impaired consciousness with a Glasgow coma scale score of 14 (E4V4M6), complained of headache, and presented with a hemorrhage in the left ear. Computed tomography suggested a skull fracture and cerebral hemorrhage. Magnetic resonance imaging conducted on the 4th day after the injury indicated shunt disease with a feeder in the right MMA. Cerebral angiography on the 7th day suggested a direct shunt from the right MMA to the MMV aligned with the temporal bone fracture line, with multiple drainage route perfusion. Coil embolization was performed on the 14th day to occlude the shunt point selectively. In the final image, the MMA was absent, and the MMV, superior sagittal sinus, or pterygoid plexus was not visible through the shunt. Her symptoms improved, and she was discharged on the 20th day and did not exhibit recurrence at the 1-year follow-up.
Conclusion: AVF with a direct shunt from the MMA to MMV after head trauma can be effectively and safely treated with coil embolization alone, despite the need for long-term postoperative follow-up.
Keywords: Middle meningeal artery, Middle meningeal vein, Selective coil embolization, Temporal bone fracture, Traumatic arteriovenous fistula
INTRODUCTION
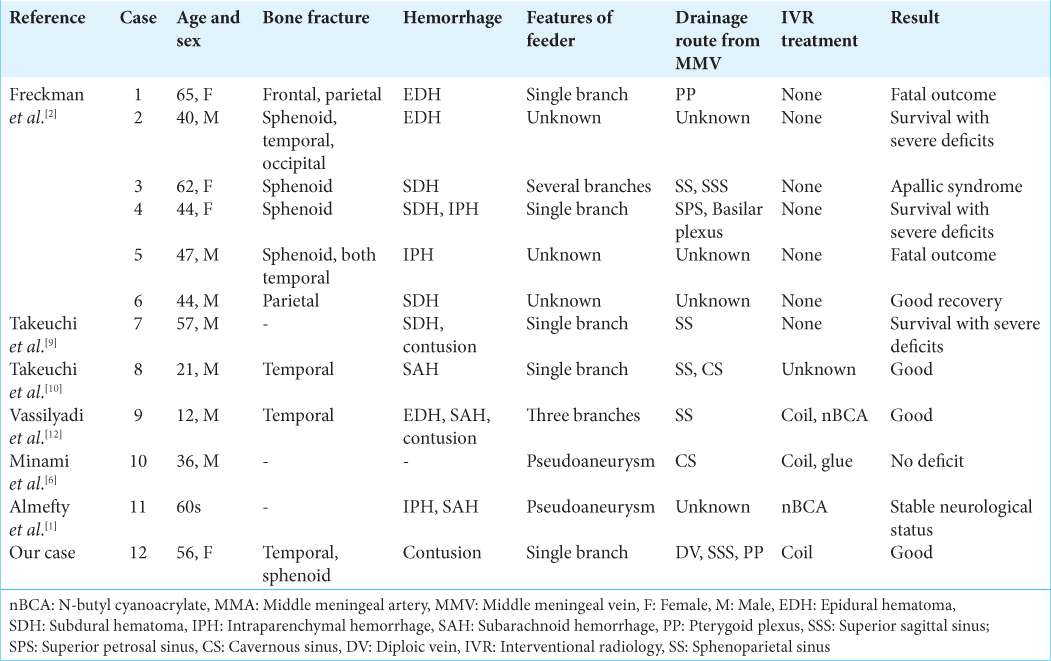
Dural arteriovenous fistulas (dAVFs) are reported to be induced by trauma, frequently having severe neurologic consequences, including hemorrhage, intracranial hypertension, focal deficits, and seizures. Posttraumatic dAVFs of the middle meningeal artery (MMA) are rare.[
CASE PRESENTATION
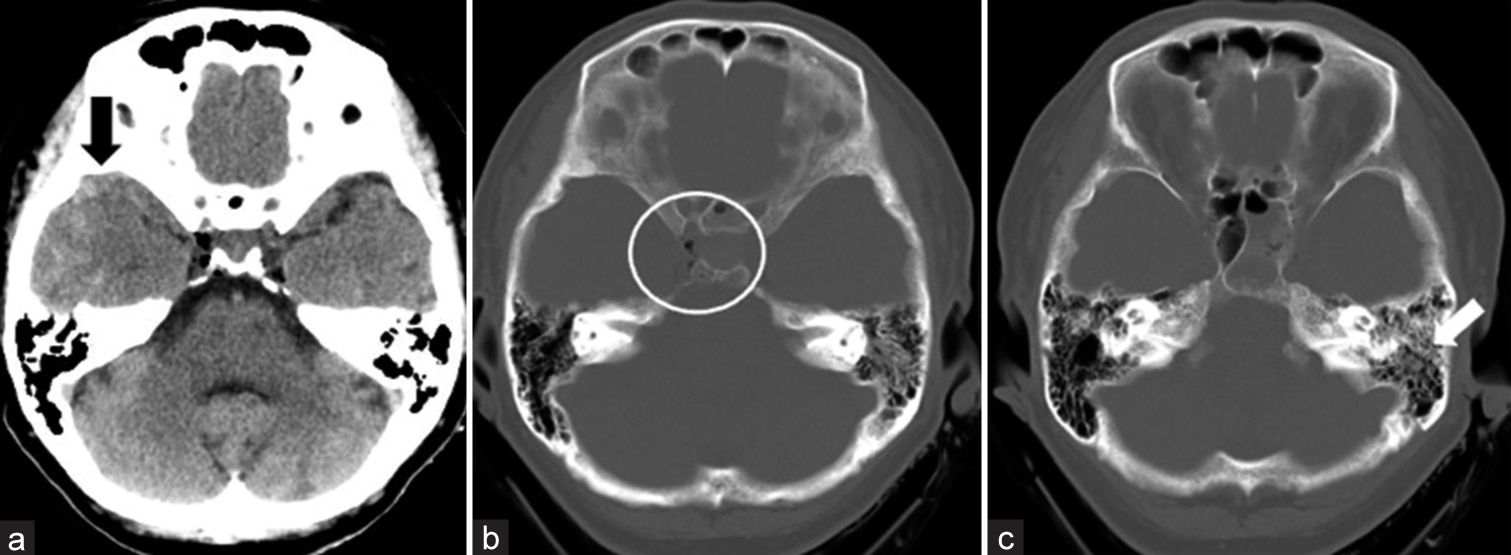
A 56-year-old woman fell and hit her head after consuming alcohol. She was brought to the emergency room due to a mild disturbance of consciousness. On arrival, she exhibited impaired consciousness with a Glasgow coma scale score of 14 (E4V4M6), complained of headache, and presented with hemorrhage in the left ear. Computed tomography (CT) of the head suggested right traumatic subarachnoid hemorrhage, cerebral contusion of the right temporal lobe, right pneumoencephalopathy, and longitudinal fracture of the left petrous bone [
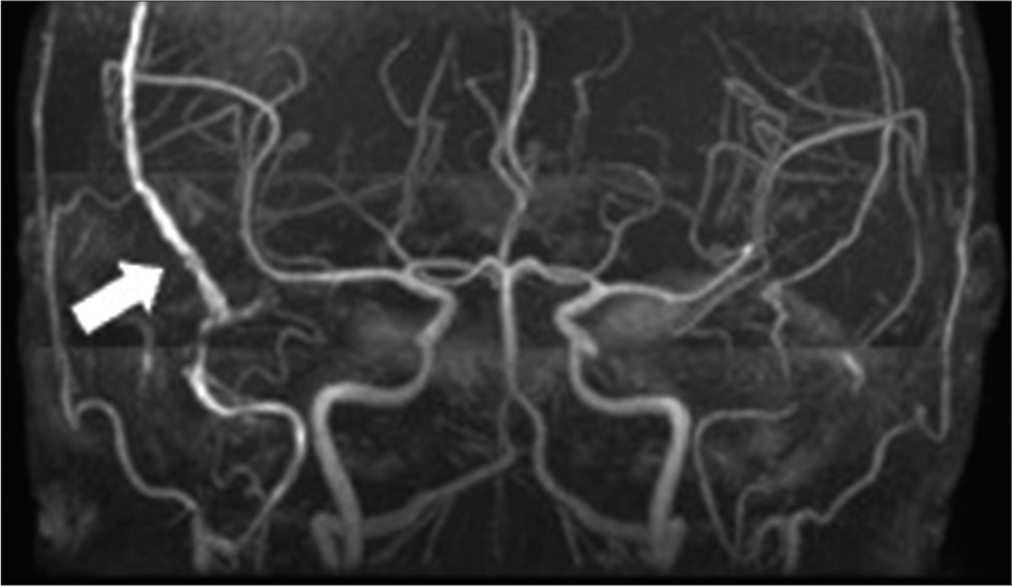
To assess the cerebral contusion in the right temporal lobe, magnetic resonance imaging of the head was conducted on the 4th day after the injury. It suggested the involvement of the right MMA and a vein, indicating the occurrence of shunt disease [
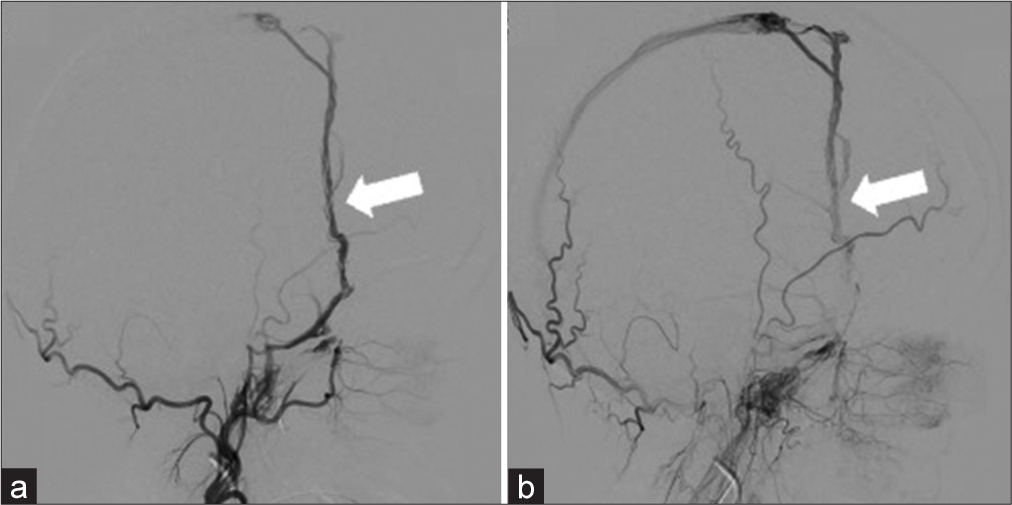
A 5Fr FUBUKI guiding catheter (Asahi Intecc Co., Ltd., Aichi, Japan), along with an intermediate catheter Guidepost (Tokai Medical Products, Aichi, Japan), was used to approach the right MMA. Subsequently, CHIKAI (Asahi Intecc Co., Ltd.) was used to guide the GREACH (Tokai Medical Products) to the shunt point. Coil embolization commenced from the MMA distal to the shunt point and continued until immediately before the point. At the shunt point, the MMV was embolized with the coil, concluding with proximal MMA embolization. Seven coils were used for the embolization. In the final image, the MMA was no longer visible, and the MMV, DV, SSS, and PP were absent [
DISCUSSION
Here, we present a case of dAVF with a single shunt from the MMA to the MMV and multiple drainage routes early in the injury after a temporal bone fracture. The patient was treated successfully with coil embolization alone.
The incidence of traumatic AVF involving MMA is 8 (1.8%) in 446 head trauma cases, signifying its relative rarity.[
The MMA courses within the dura mater on the inner surface of the skull and in cases of head trauma with compromised dura mater; moreover, the MMA is susceptible to injury.[
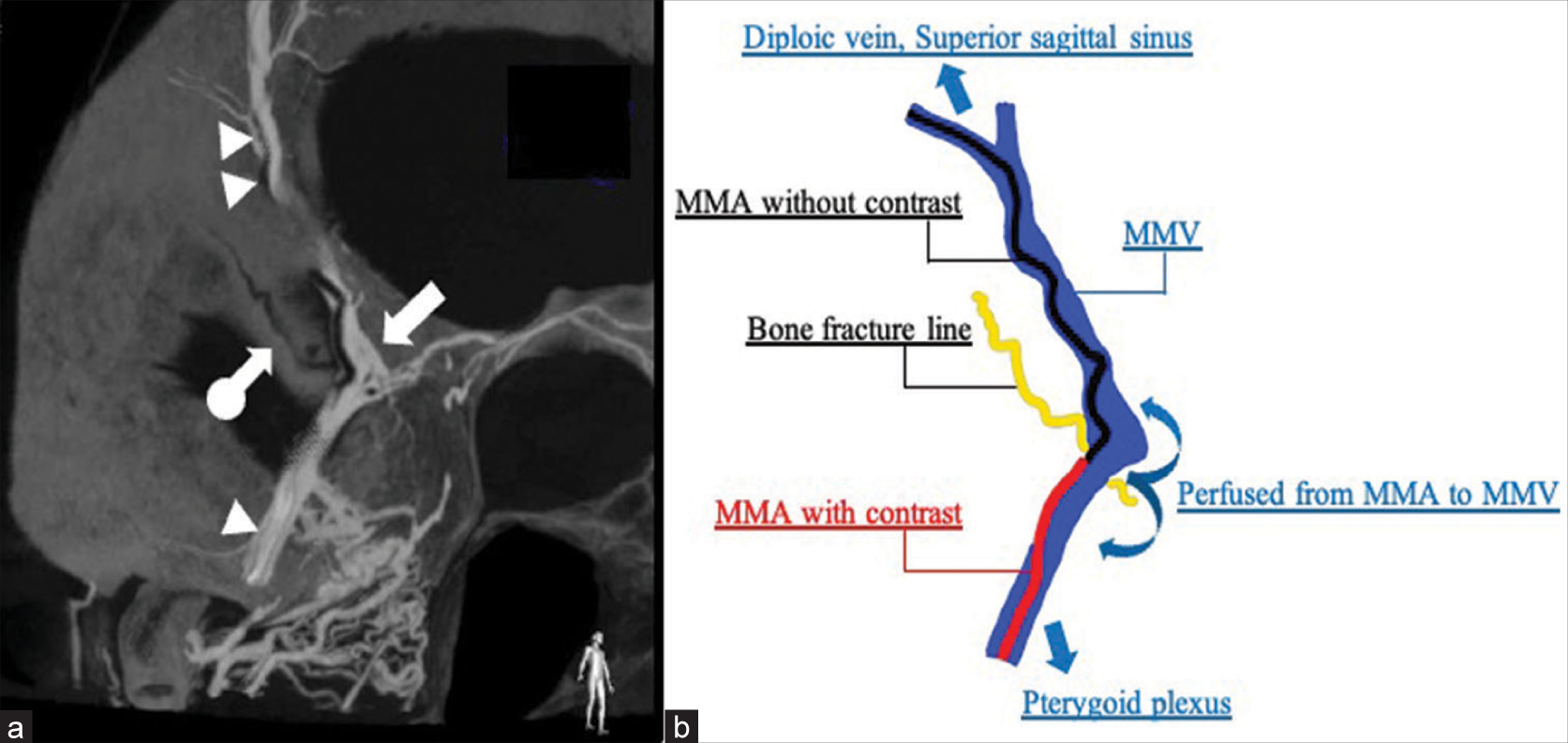
Anatomically, venous tracts in the periosteal dura are parallel to the MMA and its major branches, typically accompanied by two veins, creating a tram-track appearance. In addition, MMVs communicate with each other and with the venous sinus through DVs. Typically, they enter the PP through the foramen ovale but often open into the temporal venous plexus through the guiding venous tract before reaching the skull base.[
Unlike non-traumatic dAVF, traumatic AVF often involves only a single shunt in a single artery.[
In this case, a temporal bone fracture resulting from head trauma damaged the MMA specifically. This damage may have caused a direct shunt from the MMA to the MMV at a specific site, leading to perfusion to the DV, SSS, and PP through the MMV. Using CBCT, we accurately located the shunt point for perfusion from the MMA to MMV. This allowed us to secure the MMA and MMV beyond the shunt point using a microcatheter, and we occluded the shunt using selective coil embolization without the need for liquid embolic material.
CONCLUSION
We encountered a case of traumatic AVF with a direct shunt from the MMA to MMV and multiple drainage routes after head trauma. In contrast to non-traumatic dAVF, traumatic AVF commonly exhibits a direct shunt. In cases of traumatic AVF with such a direct shunt, preoperative identification of the shunt point is important, and CBCT proves to be highly useful for this. When the shunt site is identified accurately, selective coil embolization alone can be used to treat the shunt safely.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Almefty RO, Kalani MY, Ducruet AF, Crowley RW, McDougall CG, Albuquerque FC. Middle meningeal arteriovenous fistulas: A rare and potentially high-risk Dural arteriovenous fistula. Surg Neurol Int. 2016. 7: S219-22
2. Freckmann N, Sartor K, Herrmann HD. Traumatic arteriovenous fistulae of the middle meningeal artery and neighbouring veins or Dural sinuses. Acta Neurochir (Wien). 1981. 55: 273-81
3. Hassler O. Medial defects in the meningeal arteries. J Neurosurg. 1962. 19: 337-40
4. Kawaguchi T, Kawano T, Kaneko Y, Ooasa T, Ooigawa H, Ogasawara S. Traumatic lesions of the bilateral middle meningeal arteries--case report. Neurol Med Chir (Tokyo). 2002. 42: 221-3
5. Luo CB, Teng MM, Chang FC, Chang CY. Traumatic indirect carotid cavernous fistulas: Angioarchitectures and results of transarterial embolization by liquid adhesives in 11 patients. Surg Neurol. 2009. 71: 216-22
6. Minami H, Miki T, Kakita H, Matsumoto H, Tominaga S, Yamaura I. Traumatic aneurysm of the middle meningeal artery presenting with traumatic middle meningeal arteriovenous fistula: A case report. J Neuroendovasc Ther. 2015. 9: 84-9
7. Nakamura K, Tsugane R, Ito H, Obata H, Narita H. Traumatic arterio-venous fistula of the middle meningeal vessels. J Neurosurg. 1966. 25: 424-9
8. Shapiro M, Raz E, Nossek E, Srivatanakul K, Walker M, Mir O. Dural venous system: Angiographic technique and correlation with ex vivo investigations. J Neurointerv Surg. 2022. 14: 196-201
9. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y. Case of traumatic Dural arteriovenous fistula presenting as an acute subdural hematoma and an intracerebral hematoma. A case report. No Shinkei Geka [Neurol Surg]. 2008. 36: 907-10
10. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y. A case of traumatic middle meningeal arteriovenous fistula on the side of the head opposite to the injured side. No Shinkei Geka [Neurol Surg]. 2009. 37: 983-6
11. Tao Y, Niu Y, Zhu G, Chen Z. Endovascular treatment of a traumatic Dural arteriovenous fistula of the superior sagittal sinus using dual lumen balloon microcatheter. Neurosciences (Riyadh). 2016. 21: 158-6
12. Vassilyadi M, Mehrotra N, Shamji MF, Michaud J. Pediatric traumatic Dural arteriovenous fistula. Can J Neurol Sci. 2009. 36: 751-6