- Midwest Radiology, Saint Paul, Minnesota, United States,
- Gillette Children’s Specialty Healthcare, St. Paul, Minnesota, United States,
- Superior Medical Experts, St. Paul, Minnesota, United States,
- Department of Neurosurgery, National Brain Aneurysm and Tumor Center, Minneapolis, Minnesota, United States.
Correspondence Address:
Michael T. Madison, Midwest Radiology, Saint Paul, Minnesota, United States.
DOI:10.25259/SNI_939_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Michael T. Madison1, Patrick C. Graupman2, Jason M. Carroll1, Collin M. Torok1, Jillienne C. Touchette3, Eric S. Nussbaum4. Traumatic epidural hematoma treated with endovascular coil embolization. 06-Jul-2021;12:322
How to cite this URL: Michael T. Madison1, Patrick C. Graupman2, Jason M. Carroll1, Collin M. Torok1, Jillienne C. Touchette3, Eric S. Nussbaum4. Traumatic epidural hematoma treated with endovascular coil embolization. 06-Jul-2021;12:322. Available from: https://surgicalneurologyint.com/surgicalint-articles/10956/
Abstract
Background: Traumatic cerebrovascular injury may result in epidural hematoma (EDH) from laceration of the middle meningeal artery (MMA), which is a potentially life-threatening emergency. Treatment ranges from surgical evacuation to conservative management based on a variety of clinical and imaging factors.
Case Description: A 14-year-old male presented to our institution after falling from his bicycle with traumatic subarachnoid hemorrhage and a right frontotemporal EDH. The patient did not meet criteria for surgical evacuation and endovascular embolization of the right MMA was performed. Rapid resolution of the EDH was observed.
Conclusion: This case corroborates the sparse existing literature for the potential role of endovascular embolization to treat acute EDH in carefully selected patients who do not meet or have borderline indications for surgical management.
Keywords: Endovascular procedures, Epidural hematoma, Meningeal arteries, Traumatic cerebral hematoma, Traumatic subarachnoid hemorrhage
INTRODUCTION
Traumatic epidural hematoma (EDH) is typically associated with a skull fracture and laceration of the meningeal artery.[
The increasing use of endovascular therapies has reduced mortality rates associated with cerebrovascular injuries and disease.[
CASE REPORT
Patient history
A 14-year-old male presented to our facility after falling from his bicycle. He had lacerations on the right parietal area of his scalp and mild confusion that resolved quickly. He had lost consciousness for 1–2 min but remembered the events up to and through the traumatic incident. At the time of the original trauma, he had no associated vomiting, weakness, numbness, blurry vision, double vision, or neck pain and was not on blood thinning medication.
Clinical findings
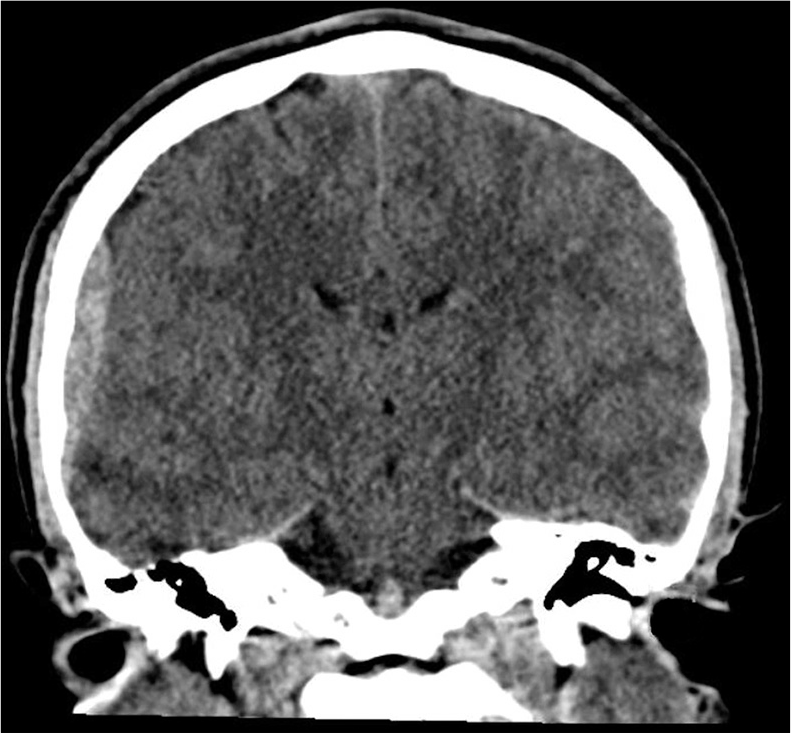
At presentation, neurological examination was benign with no focal neurologic deficits. The patient then began to have large volume emesis and increasing lethargy in the emergency department (ED), although he remained clinically stable. A head CT was performed which showed an EDH in the right frontotemporal region, measuring up to 7 mm in transverse dimension, with additional thin subdural hemorrhage extending along the lateral margin of the right temporal lobe [
Therapeutic intervention
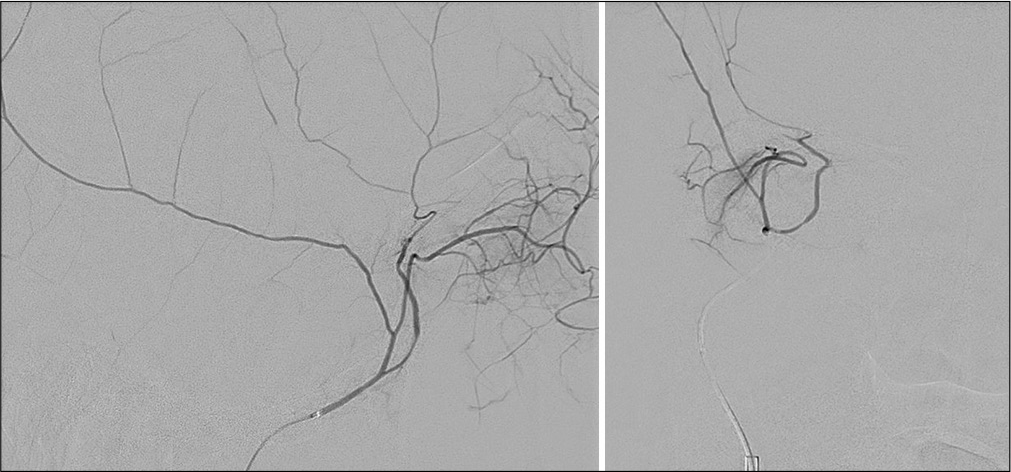
Following diagnostic angiography [
Follow-up and outcomes
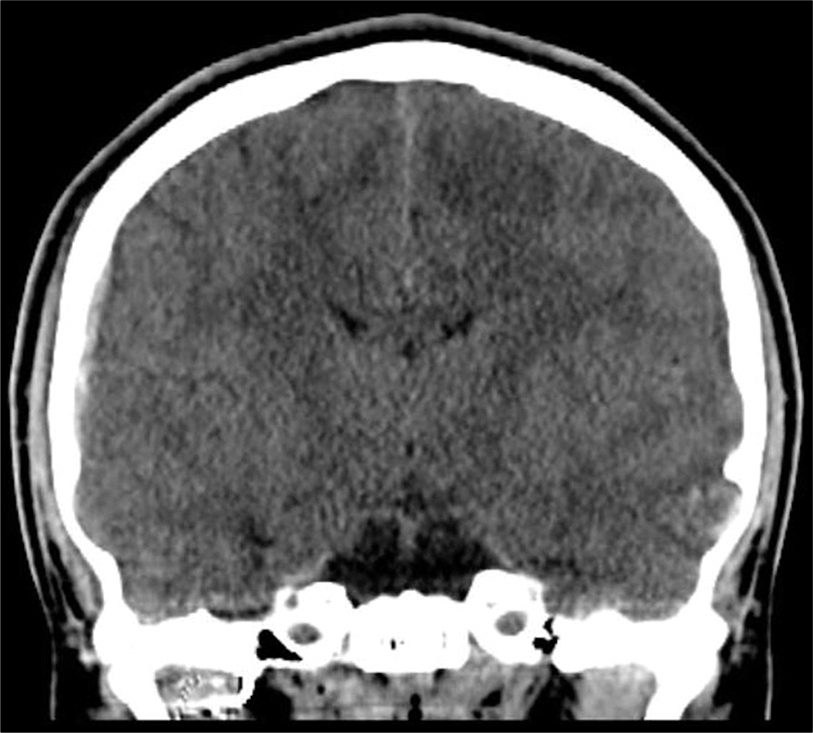
There were no apparent complications, and the patient awoke from general anesthesia at his preprocedure neurologic baseline [
DISCUSSION
In this case, a traumatic cerebrovascular injury with EDH was quickly resolved following endovascular coil embolization in a pediatric patient. This case demonstrates the potential role of endovascular coil embolization to treat acute EDH in carefully selected patients.
Cerebrovascular injuries occur in approximately 1% of all blunt traumatic brain injuries[
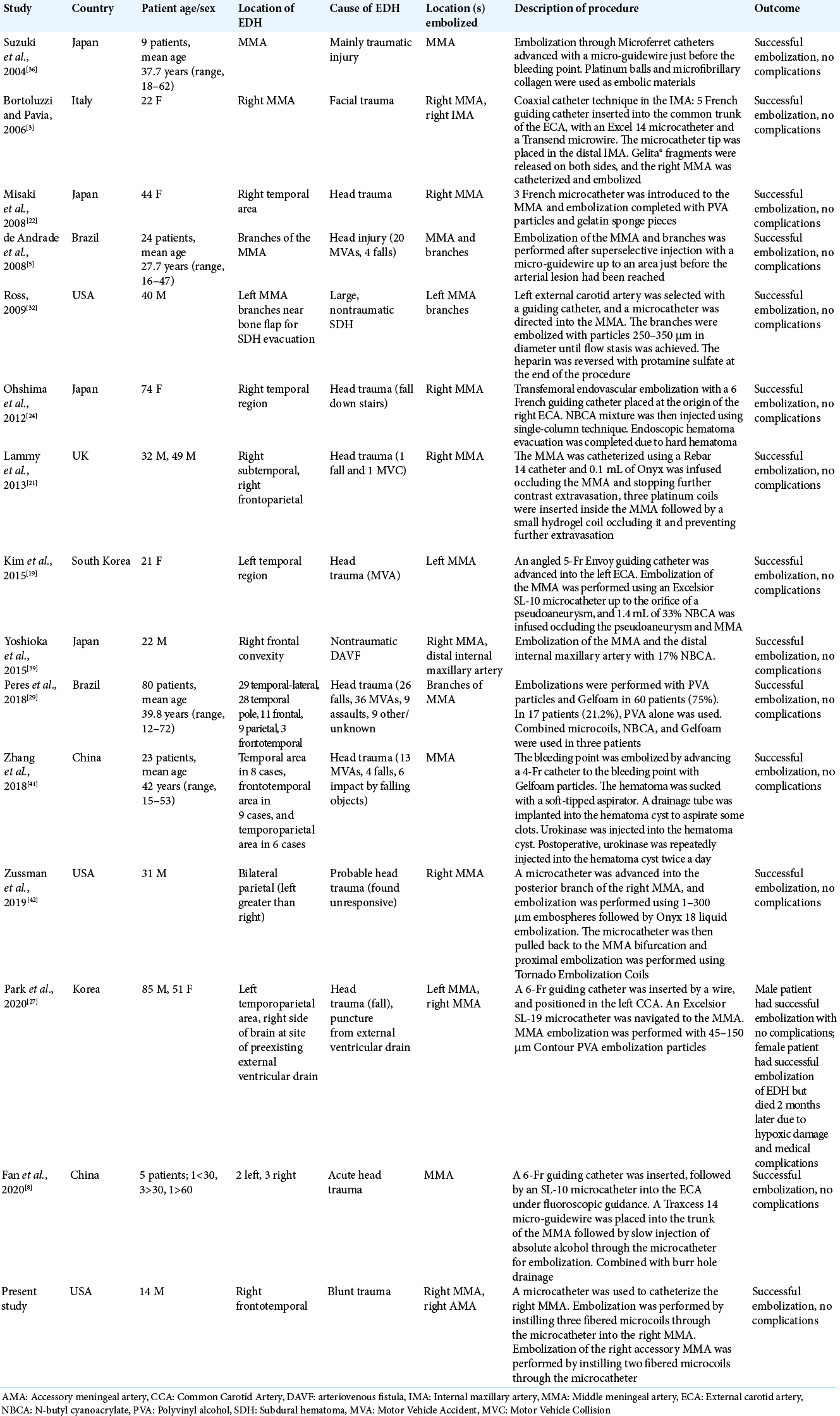
A recent study by Peres et al. reported results of 80 patients with acute, mainly temporal, EDH treated endovascularly.[
EDH occurs in approximately 6% of traumatic brain injuries in pediatric patients.[
Embolization procedures involving the MMA should only be performed by experienced neurointerventionalists familiar with head-and-neck vascular neuroanatomy, given the known potential anastomoses and variant collaterals between the MMA and the ophthalmic artery or facial arcade.[
CONCLUSION
This case demonstrates that a positive outcome and quick resolution can be achieved following embolization for acute traumatic EDH in appropriately selected patients. This technique may be considered for patients who do not meet or have borderline indications for surgical evacuation where the alternative of conservative serial imaging is expected to be prolonged.
Declaration of patient consent
Patient’s consent not required as patients identify is not disclosed or compromised.
Financial support and sponsorship
This work was supported by a grant from the United Hospital Foundation.
Conflicts of interest
Jillienne C Touchette is CEO and has ownership interest in Superior Medical Experts.
Acknowledgments
The authors acknowledge Superior Medical Experts for research and drafting assistance.
References
1. Arthurs ZM, Starnes BW. Blunt carotid and vertebral artery injuries. Injury. 2008. 39: 1232-41
2. Biffl WL, Moore EE, Ryu RK, Offner PJ, Novak Z, Coldwell DM. The unrecognized epidemic of blunt carotid arterial injuries: Early diagnosis improves neurologic outcome. Ann Surg. 1998. 228: 462-70
3. Bortoluzzi M, Pavia M. Endovascular treatment of incoercible epistaxis and epidural cerebral hematoma. A case report. Interv Neuroradiol. 2006. 12: 233-6
4. Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW. Surgical management of acute epidural hematomas. Neurosurgery. 2006. 58: S7-15
5. de Andrade AF, Figueiredo EG, Caldas JG, Paiva WS, De Amorim RL, Puglia P. Intracranial vascular lesions associated with small epidural hematomas. Neurosurgery. 2008. 62: 416-20
6. Duthie G, Reaper J, Tyagi A, Crimmins D, Chumas P. Extradural haematomas in children: A 10-year review. Br J Neurosurg. 2009. 23: 596-600
7. Edwards NM, Fabian TC, Claridge JA, Timmons SD, Fischer PE, Croce MA. Antithrombotic therapy and endovascular stents are effective treatment for blunt carotid injuries: Results from longterm followup. J Am Coll Surg. 2007. 204: 1007-13
8. Fan G, Wang H, Ding J, Xu C, Liu Y, Wang C. Application of absolute alcohol in the treatment of traumatic intracranial hemorrhage via interventional embolization of middle meningeal artery. Front Neurol. 2020. 11: 824
9. Flaherty BF, Loya J, Alexander MD, Pandit R, Ha BY, Torres RA. Utility of clinical and radiographic findings in the management of traumatic epidural hematoma. Pediatr Neurosurg. 2013. 49: 208-14
10. Flaherty BF, Moore HE, Riva-Cambrin J, Bratton SL. Pediatric patients with traumatic epidural hematoma at low risk for deterioration and need for surgical treatment. J Pediatr Surg. 2017. 52: 334-9
11. Flaherty BF, Moore HE, Riva-Cambrin J, Bratton SL. Repeat head CT for expectant management of traumatic epidural hematoma. Pediatrics. 2018. 142: e20180385
12. Fusco MR, Harrigan MR. Cerebrovascular dissections: A review. Part II: Blunt cerebrovascular injury. Neurosurgery. 2011. 68: 517-30
13. Geibprasert S, Pongpech S, Armstrong D, Krings T. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: Vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol. 2009. 30: 1459-68
14. Grigorian A, Kabutey NK, Schubl S, de Virgilio C, Joe V, Dolich M. Blunt cerebrovascular injury incidence, strokerate, and mortality with the expanded Denver criteria. Surgery. 2018. 164: 494-9
15. Hayashi N, Kubo M, Tsuboi Y, Nishimura S, Nishijima M, Abdel-Aal MA. Impact of anomalous origin of the ophthalmic artery from the middle meningeal artery on selection of surgical approach to skull base meningioma. Surg Neurol. 2007. 68: 568-71
16. Holsti M, Kadish HA, Sill BL, Firth SD, Nelson DS. Pediatric closed head injuries treated in an observation unit. Pediatr Emerg Care. 2005. 21: 639-44
17. Irie F, Le Brocque R, Kenardy J, Bellamy N, Tetsworth K, Pollard C. Epidemiology of traumatic epidural hematoma in young age. J Trauma. 2011. 71: 847-53
18. Kay PR, Freemont AJ, Davies DR. The aetiology of multiple loose bodies. Snow storm knee. J Bone Joint Surg Br. 1989. 71: 501-4
19. Kim DH, Lee JY, Jeon HJ, Cho BM, Park SH, Oh SM. Intraoperative endovascular embolization of middle meningeal artery and a pseudoaneurysm by using N-butyl 2-cyanoacrylate for hemostasis during operation of acute epidural hemorrhage. Korean J Neurotrauma. 2015. 11: 167-9
20. Knuckey NW, Gelbard S, Epstein MH. The management of “asymptomatic” epidural hematomas. A prospective study. J Neurosurg. 1989. 70: 392-6
21. Lammy S, McConnell R, Kamel M, Rennie I, Al-Haddad S. Extradural haemorrhage: Is there a role for endovascular treatment?. Br J Neurosurg. 2013. 27: 383-5
22. Misaki K, Muramatsu N, Nitta H. Endovascular treatment for traumatic ear bleeding associated with acute epidural hematoma. Neurol Med Chir (Tokyo). 2008. 48: 208-10
23. Nyberg EM, Chaudry MI, Turk AS, Turner RD. Transient cranial neuropathies as sequelae of Onyx embolization of arteriovenous shunt lesions near the skull base: Possible axonotmetic traction injuries. J Neurointerv Surg. 2013. 5: e21
24. Ohshima T, Tajima H, Fujii K, Nagakura M, Nishizawa T, Kato K. Combined endovascular and endoscopic surgery for acute epidural hematoma in a patient with poor health. Neurol Med Chir (Tokyo). 2012. 52: 829-31
25. Paiva WS, Andrade AF, Mathias L, Guirado VM, Amorim RL, Magrini NN. Management of supratentorial epidural hematoma in children: Report on 49 patients. Arq Neuropsiquiatr. 2010. 68: 888-92
26. Pang D, Horton JA, Herron JM, Wilberger JE, Vries JK. Nonsurgical management of extradural hematomas in children. J Neurosurg. 1983. 59: 958-71
27. Park TJ, Lee SP, Baek J, Ryou K, Kim SH. Middle meningeal artery embolization to treat progressive epidural hematoma: A case report. J Cerebrovasc Endovasc Neurosurg. 2020. 22: 20-5
28. Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet. 2012. 380: 499-505
29. Peres CM, Caldas J, Puglia P, de Andrade AF, da Silva IA, Teixeira MJ. Endovascular management of acute epidural hematomas: Clinical experience with 80 cases. J Neurosurg. 2018. 128: 1044-50
30. Perrini P, Cardia A, Fraser K, Lanzino G. A microsurgical study of the anatomy and course of the ophthalmic artery and its possibly dangerous anastomoses. J Neurosurg. 2007. 106: 142-50
31. Qureshi AI. Endovascular treatment of cerebrovascular diseases and intracranial neoplasms. Lancet. 2004. 363: 804-13
32. Ross IB. Embolization of the middle meningeal artery for the treatment of epidural hematoma. J Neurosurg. 2009. 110: 1247-9
33. Samples DC, Bounajem MT, Wallace DJ, Liao L, Tarasiewicz I. Role of follow-up CT scans in the management of traumatic pediatric epidural hematomas. Childs Nerv Syst. 2019. 35: 2195-203
34. Sharp NE, Svetanoff WJ, Desai A, Alemayehu H, Raghavan MU, Sharp SW. Radiation exposure from head computed tomography scans in pediatric trauma. J Surg Res. 2014. 192: 276-9
35. Sheppard JP, Nguyen T, Alkhalid Y, Beckett JS, Salamon N, Yang I. Risk of brain tumor induction from pediatric head CT procedures: A systematic literature review. Brain Tumor Res Treat. 2018. 6: 1-7
36. Suzuki S, Endo M, Kurata A, Ohmomo T, Oka H, Kitahara T. Efficacy of endovascular surgery for the treatment of acute epidural hematomas. AJNR Am J Neuroradiol. 2004. 25: 1177-80
37. Tubbs RS, Walker AM, Demerdash A, Matusz P, Loukas M, Cohen-Gadol AA. Skull base connections between the middle meningeal and internal carotid arteries. Childs Nerv Syst. 2015. 31: 1515-20
38. Wang AG, Liu JH, Hsu WM, Luo CB, Yen MY. Choroidal infarction after embolization of arteriovenous fistula of middle meningeal artery. Retina. 2000. 20: 573-5
39. Yoshioka S, Kuwayama K, Satomi J, Nagahiro S. Transarterial N-butyl-2-cyanoacrylate embolization of an intraosseous dural arteriovenous fistula associated with acute epidural hematoma: Technical case report. Neurosurgery. 2015. 11: E468-71
40. Yu J, Guo Y, Xu B, Xu K. Clinical importance of the middle meningeal artery: A review of the literature. Int J Med Sci. 2016. 13: 790-9
41. Zhang Y, Li Q, Zhao R, Yang Z, Li Y, Min W. Novel minimally invasive treatment strategy for acute traumatic epidural hematoma: Endovascular embolization combined with drainage surgery and use of urokinase. World Neurosurg. 2018. 110: 206-9
42. Zussman BM, Goldschmidt E, Faraji AH, Salvetti DJ, Jankowitz BT. Middle meningeal artery embolization for the treatment of an expanding epidural hematoma. World Neurosurg. 2019. 128: 284-6