- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, WI, USA
Correspondence Address:
Ha Son Nguyen
Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, WI, USA
DOI:10.4103/2152-7806.182548
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nguyen HS, Doan N, Lozen A, Gelsomino M, Shabani S, Kurpad S. Traumatic spondyloptosis at the cervico-thoracic junction without neurological deficits. Surg Neurol Int 17-May-2016;7:
How to cite this URL: Nguyen HS, Doan N, Lozen A, Gelsomino M, Shabani S, Kurpad S. Traumatic spondyloptosis at the cervico-thoracic junction without neurological deficits. Surg Neurol Int 17-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/traumatic-spondyloptosis-at-the-cervico%e2%80%91thoracic-junction-without-neurological-deficits/
Abstract
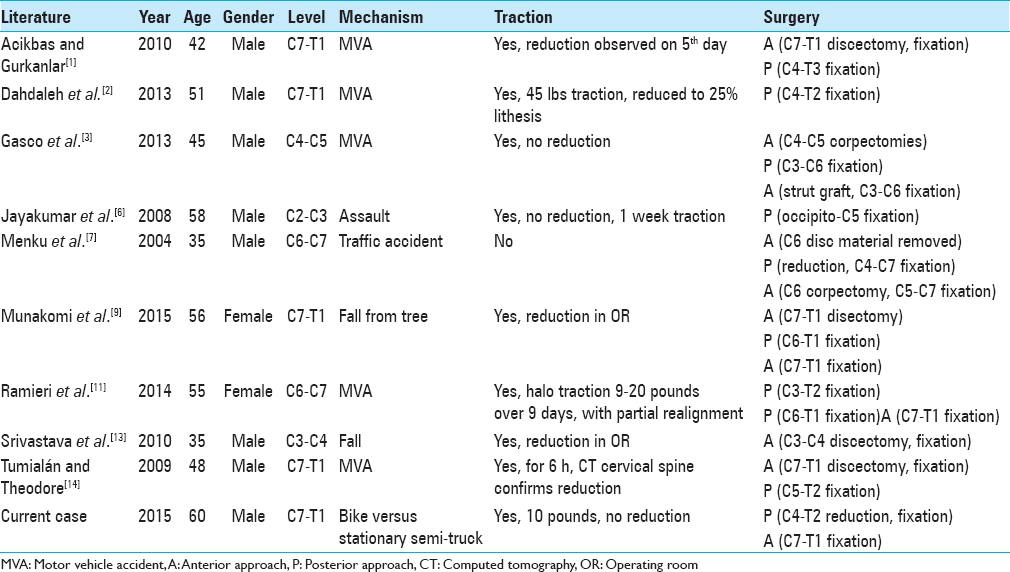
Background:There have been rare cases of traumatic cervical spondyloptosis without neurological compromise. We report another case and provide a review of the literature, with a focus on appropriate management.
Case Description:A 60-year-old male rode his bicycle into a stationary semi-truck. He reported initial bilateral upper extremity paresthesias that resolved. Imaging demonstrated C7 on T1 spondyloptosis. Traction did not achieve reduction and a halo was applied. Subsequently, he underwent posterior decompression C6-T1, reduction via bilateral complete facetectomies at C7, and fixation from C4 to T2 fixation. Afterward, an anterior C7-T1 fixation occurred, where exposure was performed through a midline sternotomy. Postoperatively, he woke up with baseline motor and sensory examination in his extremities. He did exhibit voice hoarseness due to paralysis of the left vocal cords. He was discharged home 3 days after surgery. At 6 months follow-up, there was a progressive improvement of the left vocal cords to slight paresis; dynamic X-rays demonstrated no instability with good fusion progression.
Conclusion:Traumatic cervical spondyloptosis without neurological compromise is a rare and challenging scenario. There is a concern for neurologic compromise with preoperative traction, but if specific posterior elements are fractured, the spinal canal may be wide enough where the concern for disc migration is minimal. For patients who have not been reduced preoperatively, a posterior approach with initial decompression to widen the canal, before reduction, appears safe. This scheme may avoid an initial anterior approach for decompression, necessitating a 3-stage procedure if circumferential stabilization is pursued.
Keywords: Fracture dislocation, neurologically intact, spondyloptosis
INTRODUCTION
Spondyloptosis leads to severe spinal cord compression and neurological deficits. Here, we report another case of cervical spondyloptosis where the patient remained neurologically intact and provided a review of the literature, focusing on appropriate management.
CASE PRESENTATION
Clinical presentation and neurodiagnostic studies
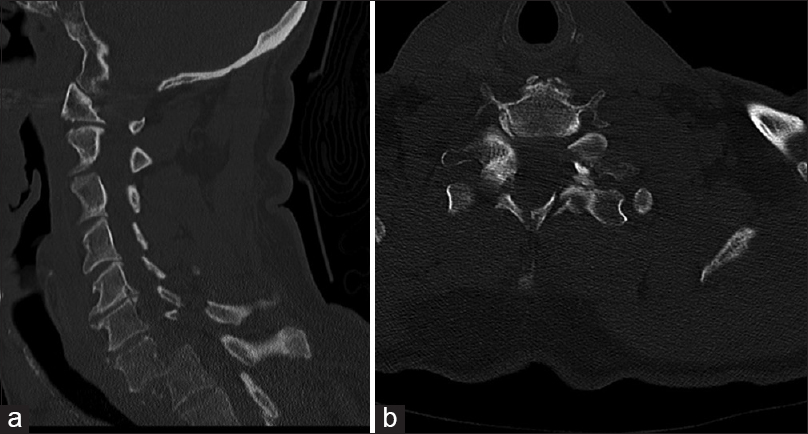
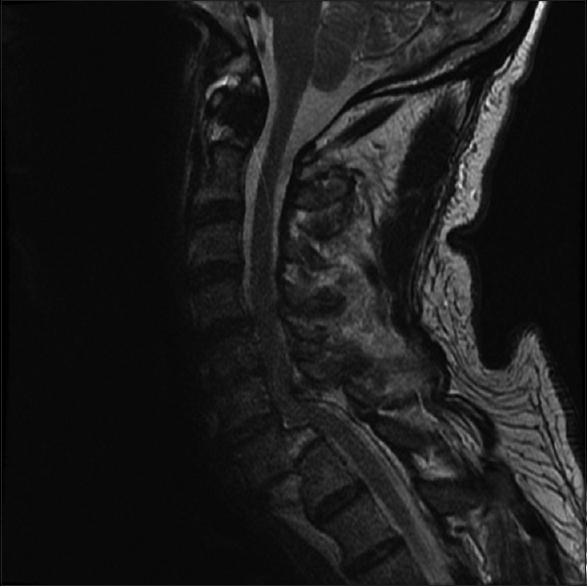
A 60-year-old male presented to the hospital after riding his bicycle into a stationary semi-truck. He reported initial bilateral upper extremity paresthesias that resolved before presentation. A computed tomography (CT) scan of the cervical spine demonstrated C7 on T1 spondyloptosis, with fractures of both C7 pedicles, C7/T1 facets, and C7 lamina [
Treatment strategies
Cervical traction of 10 pounds was applied with tongs but failed to reduce the subluxation. A halo was placed; the next day the patient underwent a posterior decompression (inferior C6 laminectomy, bilateral C7 laminectomy, superior T1 laminectomy), with reduction of the fracture/dislocation utilizing bilateral complete facetectomies at C7, and fusion from C4 to T2. Intraoperatively, the O-arm documented adequate reduction. Subsequently, on the same day, an anterior C7-T1 fusion was performed through a midline sternotomy.
Intraoperative monitoring
Intraoperative monitoring (somatosensory evoked potentials [SSEPs], motor evoked potentials [MEPs], electromyography) was employed for both procedures; after reduction of the fracture via the posterior approach, SSEPs improved. At the end of the anterior procedure, SSEP and MEP remained normal. Postoperatively, he was neurologically intact.
Left-sided recurrent laryngeal nerve injury
Postoperatively, the patient was hoarse. This was attributed to the anterior C7/T1 exposure, which involved moderate retraction of the recurrent laryngeal nerve. He had paralysis of the left vocal cords. Six months later, this was just a mild paresis.
Six-month outcome and dynamic X-rays
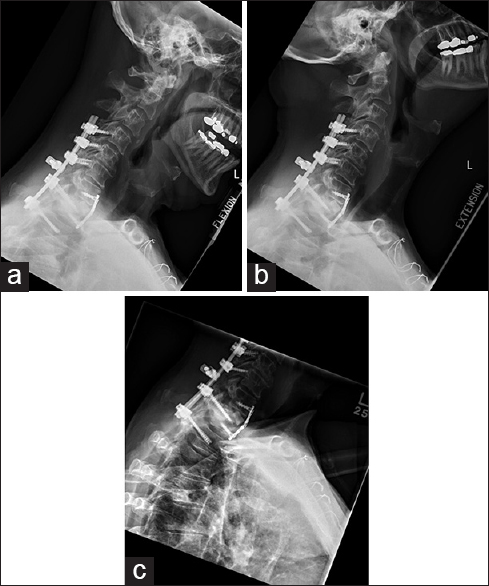
Six months postoperatively, the patient was intact, and dynamic X-rays demonstrated no instability (e.g., adequate fusion) [
DISCUSSION
Spondyloptosis is more common within the lumbar spine than the cervical spine.[
Management of cervical spondyloptosis
The management of cervical spondyloptosis for patients with severe deficits involves reduction, and fusion, which can occur anteriorly and/or posteriorly.[
Spontaneous decompression of the fracture level with bilateral pedicle, facet and laminar fractures and timing of reduction
The fractures of bilateral pedicles and posterior elements reduce the threat of cord compromise in these patients with C7/T1 spondyloptosis. However, prolonged dislocation may result in stasis of blood flow within the vertebral arteries, leading to thrombus formation; subsequent reduction may restore blood flow and dislodge the thrombus, leading to ischemic events.[
Surgical goals
Surgical goals include vertebral realignment and stabilization. Overall, preoperative reduction is only rarely, safely, and feasible. Most surgeons, therefore, advocate circumferential stabilization.[
Maneuvers in this case to treat C7/T1 spondyloptosis
In the case presented, as traction failed to achieve the reduction, the patient required the placement of a halo device and subsequently underwent posterior decompression/fusion followed by anterior cervical surgery (decompression/fusion). Three of the prior reported cases[
Financial support and sponsorship
Dr. Kurpad is funded by the Byron Riesch Paralysis Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Acikbas C, Gurkanlar D. Post-traumatic C7-T1 spondyloptosis in a patient without neurological deficit: A case report. Turk Neurosurg. 2010. 20: 257-60
2. Dahdaleh NS, Dlouhy BJ, Greenlee JD, Smoker WR, Hitchon PW. An algorithm for the management of posttraumatic cervical spondyloptosis. J Clin Neurosci. 2013. 20: 951-7
3. Gasco J, Dilorenzo DJ, Patterson JT. C4-C5 post-traumatic spondyloptosis with in situ fusion: Systematic literature review and case report. Spine (Phila Pa 1976). 2013. 38: E621-5
4. Goel A, Muzumdar D, Dange N. One stage reduction and fixation for atlantoaxial spondyloptosis: Report of four cases. Br J Neurosurg. 2006. 20: 209-13
5. Goffin J, Grob D. Spondyloptosis of the cervical spine in neurofibromatosis. A case report. Spine (Phila Pa 1976). 1999. 24: 587-90
6. Jayakumar P, Choi D, Casey A. Late presentation of a type III axis fracture with spondyloptosis. Ann R Coll Surg Engl. 2008. 90: W1-3
7. Menku A, Kurtsoy A, Tucer B, Oktem IS, Akdemir H. The surgical management of traumatic C6 – C7 spondyloptosis in a patient without neurological deficits. Minim Invasive Neurosurg. 2004. 47: 242-4
8. Merianos P, Manousidis D, Samsonas P, Baltopoulos P, Pateras N, Mavroudis G. Injuries of the lower cervical spine associated with widening of the spinal canal. Injury. 1994. 25: 645-8
9. Munakomi S, Bhattarai B, Cherian I. Traumatic cervical spondyloptosis in a neurologically stable patient: A therapeutic challenge. Case Rep Crit Care 2015. 2015. p.
10. Muzumdar DP, Goel A. C2 over C3 spondyloptosis in a case with absent posterior elements.Report of an unusual case and analysis of treatment options. J Clin Neurosci. 2004. 11: 675-7
11. Ramieri A, Domenicucci M, Cellocco P, Lenzi J, Dugoni DE, Costanzo G. Traumatic spondylolisthesis and spondyloptosis of the subaxial cervical spine without neurological deficits: Closed re-alignment, surgical options and literature review. Eur Spine J. 2014. 23: 658-63
12. Sribnick EA, Hoh DJ, Dhall SS. Traumatic high-grade cervical dislocation: Treatment strategies and outcomes. World Neurosurg. 2014. 82: 1374-9
13. Srivastava SK, Agrawal KM, Sharma AK, Agrawal MD, Bhosale SK, Renganathan SR. C3-C4 spondyloptosis without neurological deficit-a case report. The spine journal: Official journal of the North American Spine Society. 2010. 10: e16-20
14. Tumialán LM, Dadashev V, Laborde DV, Gupta SK. Management of traumatic cervical spondyloptosis in a neurologically intact patient: Case report. Spine (Phila Pa 1976). 2009. 34: E703-8
15. Tumialán LM, Theodore N. Basilar artery thrombosis after reduction of cervical spondyloptosis: A cautionary report. J Neurosurg Spine. 2012. 16: 492-6