- Department of Neurological Surgery, Baylor Scott and White, Temple, Texas, United States.
- Department of Orthopedic Surgery, Baylor Scott and White, Temple, Texas, United States.
Correspondence Address:
Lokeshwar Sai Santosh Bhenderu, Department of Neurological Surgery, Baylor Scott and White, Temple, Texas, United States.
DOI:10.25259/SNI_234_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lokeshwar Sai Santosh Bhenderu1, Kristopher A. Lyon1, William Trent Richardson1, Ronak Desai2, Hilda H. Kriel2, Mark D. Rahm2. Treatment of unilateral L5–S1 locked facet in a pediatric patient. 07-Apr-2023;14:133
How to cite this URL: Lokeshwar Sai Santosh Bhenderu1, Kristopher A. Lyon1, William Trent Richardson1, Ronak Desai2, Hilda H. Kriel2, Mark D. Rahm2. Treatment of unilateral L5–S1 locked facet in a pediatric patient. 07-Apr-2023;14:133. Available from: https://surgicalneurologyint.com/surgicalint-articles/12236/
Abstract
Background: Traumatic unilateral lumbosacral facet dislocations are rare injuries. The majority of cases are treated with open reduction and instrumented spinal fusions. Only less commonly can they be managed conservatively.
Case Description: A 7-year-old unrestrained passenger was involved in a high-speed motor vehicle accident. X-ray/magnetic resonance/computed tomography imaging documented a unilateral L5–S1 facet dislocation and multiple lumbar/sacral fractures. The patient underwent open reduction and temporary L5-pelvic instrumentation without fusion; the instrumentation was removed 10 weeks later at which point follow-up imaging showed preserved lumbosacral stability.
Conclusion: Open reduction with temporary instrumentation without fusion was successfully utilized to treat a unilateral L5–S1 facet dislocation in a 7-year-old child.
Keywords: Facet dislocation, Locked facet, Pediatric spine injury, Spinal instrumentation
INTRODUCTION
Traumatic facet dislocations at the L5–S1 level rarely occur following high-impact trauma.[
CASE SUMMARY
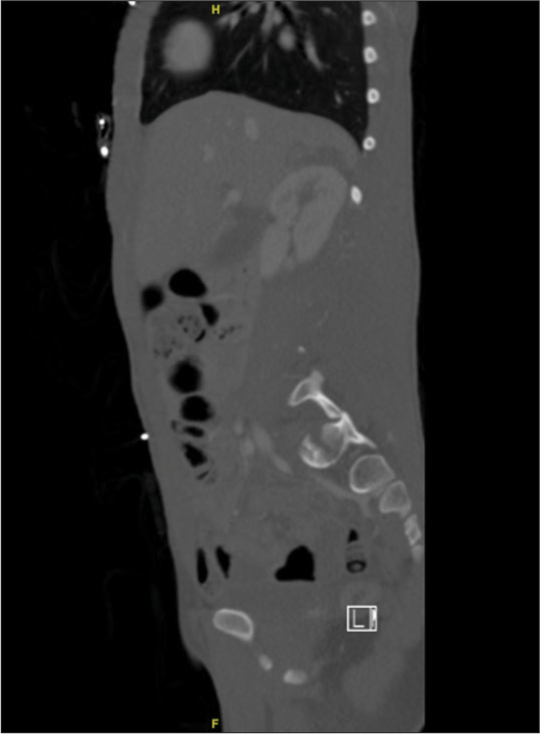
A 7-year-old male presented after a high-speed motor vehicle collision with severe back pain and lumbar radiculopathy, but without a focal neurological deficit or sphincter dysfunction. The lumbar computed tomography showed; spinous process fractures of L1–L3, right transverse process fractures of L3–L5, left L4 lamina and inferior articular facet fractures, bilateral transverse and lateral mass fractures of S1 with a diastases of the left SI joint, and a left L5–S1 facet dislocation [
Surgery
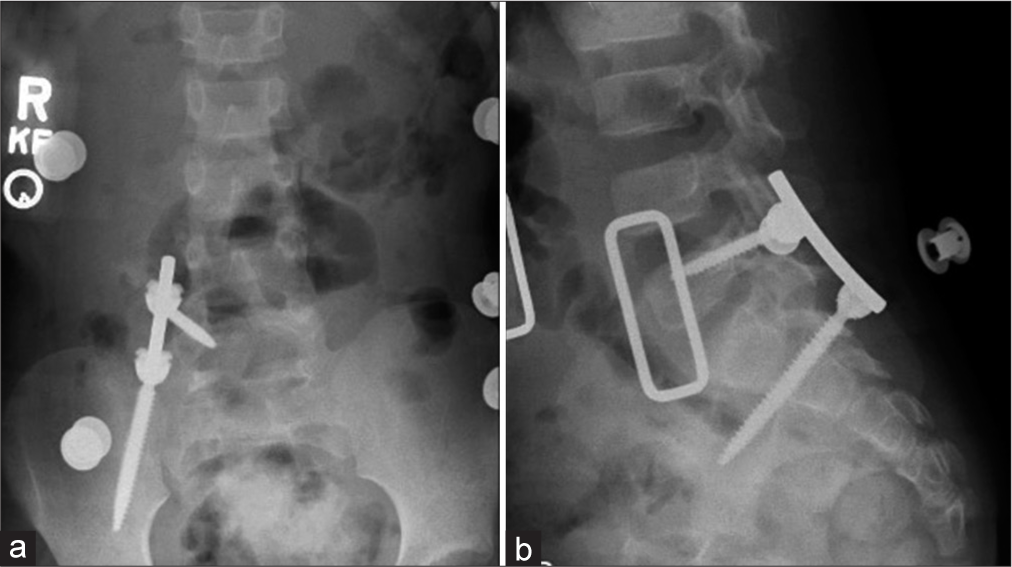
With neuromonitoring and under fluoroscopic guidance, a unilateral L4-S1 exposure was performed on the right side. At surgery, marked posterior tissue disruption was noted involving avulsion of the spinous processes from L3 to 5. There was also significant periosteal stripping of the L3–5 lamina, and the right facet capsule and joint of L5–S1 were disrupted/dislocated. A clamp placed on the lamina of L5 allowed for manual reduction of the dislocation, and placement of a right-sided L5 pedicle screw. Another incision was performed medial/superior to the posterior superior iliac spine of the right ilium, and a right iliac screw was applied (i.e., requiring resection of a small portion of posterior iliac apophysis) [
Removal of instrumentation 10 weeks later with X-rays showed adequate alignment
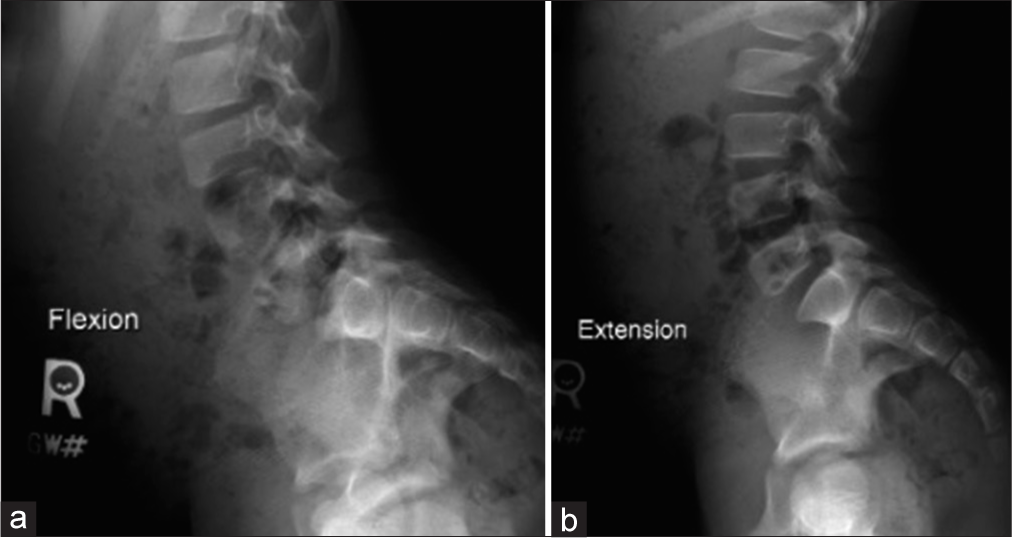
Ten weeks later, the patient underwent removal of all instrumentation on the right side. When followed for an additional 16 months postoperatively, he had no pain, a normal gait, and flexion/extension X-rays which showed no pathological L5–S1 motion [
DISCUSSION
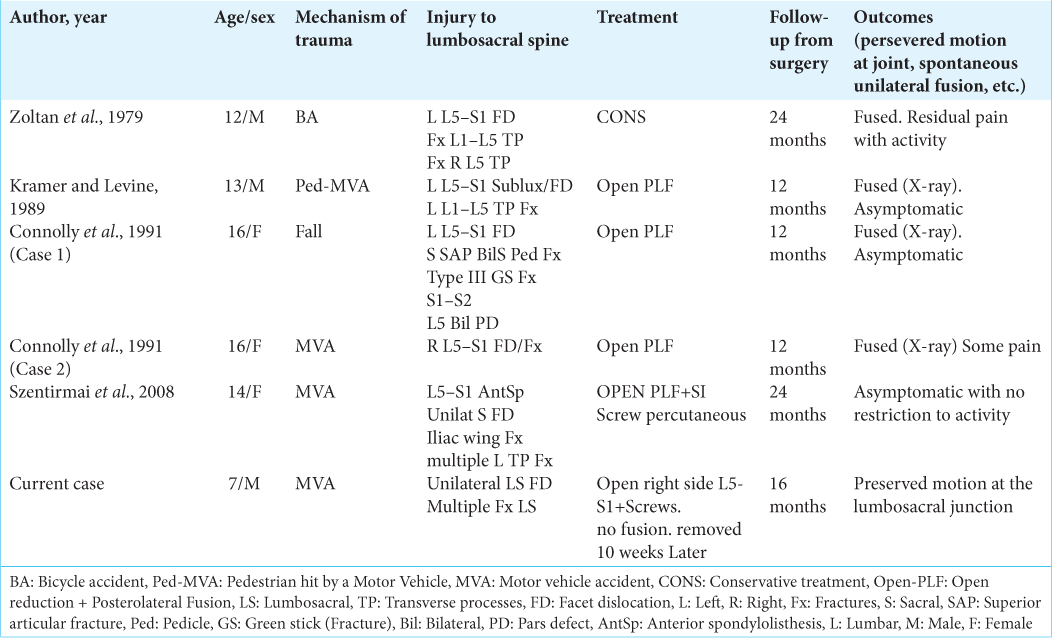
We performed a literature review of unilateral L5–S1 locked facets in pediatric patients. This identified five cases from four reports obtained from PubMed [
CONCLUSION
A 7-year-old male with a unilateral L5–S1 lumbosacral facet dislocation was effectively treated with open reduction and temporary instrumentation without fusion (i.e., unilateral L5 pedicle and iliac screw placement without bony decortication or graft placement). Ten weeks later, once the instrumentation was removed, the patient remained asymptomatic, and demonstrated adequate X-ray documented stability.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cho N, Alkins R, Khan OH, Ginsberg H, Cusimano MD. Unilateral lumbar facet dislocation: Case report and review of the literature. World Neurosurg. 2019. 123: 310-6
2. Connolly PJ, Esses SI, Heggeness MH, Cook SS. Unilateral facet dislocation of the lumbosacral junction. Spine (Phila Pa 1976). 1992. 17: 1244-8
3. Fok KC, Cheung JP. Traumatic bilateral L4-5 facet fracture dislocation: A case presentation with mechanism of injury. BMC Musculoskelet Disord. 2019. 20: 558
4. Grivas TB, Papadakis SA, Katsiva V, Koufopoulos G, Mouzakis V. Unilateral lumbosacral dislocation: Case report and a comprehensive review. Open Orthop J. 2012. 6: 473-7
5. Kramer KM, Levine AM. Unilateral facet dislocation of the lumbosacral junction. A case report and review of the literature. J Bone Joint Surg Am. 1989. 71: 1258-61
6. Mori K, Hukuda S, Katsuura A, Saruhashi Y, Asajima S. Traumatic bilateral locked facet at L4-5: Report of a case associated with incorrect use of a three-point seatbelt. Eur Spine J. 2002. 11: 602-5
7. Rhea E, Rahmathulla G. Traumatic unilateral L3-4 jumped facet treated with open reduction and short segment fusion. World Neurosurg. 2018. 119: 103-7
8. Szentirmai O, Seinfeld J, Beauchamp K, Patel V. Traumatic unilateral lumbosacral jumped facet without fracture in a child-presentation of a safe treatment strategy for a rare injury. Patient Saf Surg. 2008. 2: 29
9. Younus A, Kelly A. Lumbar unifacet dislocation without an associated fracture-a case report and literature review. Interdiscipl Neurosurg. 2021. 23: 100973
10. Zoltan JD, Gilula LA, Murphy WA. Unilateral facet dislocation between the fifth lumbar and first sacral vertebrae. Case report. J Bone Joint Surg Am. 1979. 61: 767-9