Neurovascular
Original Article
- Department of Neurosurgery, Konyang College of Medicine, Konyang University Hospital, Daejeon, Republic of Korea
- Department of Neurosurgery, Hankook Hospital, Cheongju, Republic of Korea
- Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea
- Department of Neurosurgery, The Ajou University School of Medicine, Ajou University Hospital, Suwon, Republic of Korea
- Department of Neurosurgery, College of Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
Correspondence Address:
Yong Sam Shin
Department of Neurosurgery, College of Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Republic of Korea
DOI:10.4103/sni.sni_132_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jihye Song, Jung Eon Park, Joonho Chung, Yong Chul Lim, Yong Sam Shin. Treatment strategies of ruptured posterior inferior cerebellar artery aneurysm according to its segment. 25-Jul-2017;8:155
How to cite this URL: Jihye Song, Jung Eon Park, Joonho Chung, Yong Chul Lim, Yong Sam Shin. Treatment strategies of ruptured posterior inferior cerebellar artery aneurysm according to its segment. 25-Jul-2017;8:155. Available from: https://surgicalneurologyint.com/surgicalint-articles/treatment-strategies-of-ruptured-posterior-inferior-cerebellar-artery-aneurysm-according-to-its-segment/
Abstract
Background:The aim of this study was to evaluate the clinical outcomes between endovascular treatment (EVT) and surgery of the ruptured posterior inferior cerebellar artery (PICA) aneurysms and suggest proper management strategies according to the PICA segment.
Methods:We retrospectively analyzed clinical and radiological data of patients with ruptured PICA aneurysms who underwent surgery or EVT from three different institutes. Clinical outcomes were evaluated by mRS.
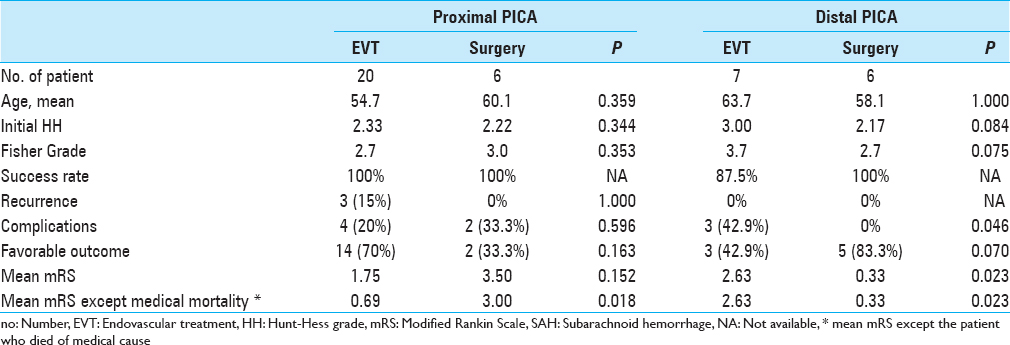
Results:We collected 39 consecutive patients with 39 ruptured PICA aneurysms; 26 patients were with proximal segment aneurysm and 13 patients were with distal. Of the 26 proximal PICA aneurysms, 20 aneurysms were treated with EVT and 6 aneurysms were treated with surgery. EVT seemed to have more favorable clinical outcome (mRS 0–2; mean mRS, 1.75 for EVT vs 3.50 for surgery, P = 0.152). Of the 13 distal PICA aneurysms, 7 aneurysms were treated with EVT and 6 were treated with surgery. Surgery showed more favorable clinical outcome (mean mRS, 2.63 for EVT vs 0.33 for surgery, P = 0.023) and lower procedure-related complication rate (42.9% for EVT vs 0% for surgery, P = 0.046) than EVT.
Conclusions:For the treatment of ruptured PICA aneurysms, EVT seemed to have more favorable outcomes for proximal segment, while surgery showed more favorable outcomes for distal segment. Additional experience and follow-up are needed in a larger series to state the efficacy of this strategy.
Keywords: Endovascular treatment, intracranial aneurysm, posterior inferior cerebellar aneurysm, surgery
INTRODUCTION
The posterior inferior cerebellar artery (PICA) is very tortuous, has a small diameter, and projects along the brainstem and cerebellum.[
MATERIALS AND METHODS
This study was approved by our institutional review board. The requirement to obtain written informed consent to participate in this study was waived. We retrospectively collected data of patients who were treated for ruptured PICA aneurysms in three referral hospitals (Seoul St. Mary’s Hospital, Ajou University Hospital and Severance Hospital). Those three institutions have a tertiary neurointerventional center, and their neurointerventionists completed a fellowship program with Dr. YS Shin, therefore, the neurointerventionists were expected to follow similar management strategies for aneurysm treatment. From October 2002 to April 2013, 39 patients with 39 cases of PICA aneurysm were included (mean age 58.9 years; range). One of them had a failed endovascular treatment, after which microsurgical treatment was performed).
There were 7 men and 32 women (mean age 58.9 years, range: 21-75 years). The mean follow-up duration was 19 months (range: 1 month − 6 years). The PICA infarct area was confirmed by a post-procedure CT after surgery or by diffusion MRI after EVT and neurologic changes before and after treatment. All except 10 patients (three patients lost follow-up, and seven patients died) were evaluated by MR angiography, CT angiography, or transfemoral cerebral angiography (TFCA) after treatment.
The PICA was divided into 5 segments according to the classification by Lister et al.[
All patients with ruptured aneurysms were treated within 24 hours. Endovascular treatment was performed under general anesthesia. If a stent needed to be implanted, 200 mg of aspirin and 300 mg of clopidogrel were loaded through the Levin-tube in patients. These patients then maintained on daily doses of 100 mg of aspirin and 75 mg of clopidogrel for 3 to 6 months, followed by aspirin 100 mg daily for 12 months.
The choice of the treatment strategy was made through multidisciplinary team. Selective endosaccular coiling was performed in the case of reasonable neck morphology, and if vessels were tortuous or had a narrow lumen (not wide enough to insert the microcatheter) and suspected of a distal PICA dissection with well-developed collateral circulations, parent artery occlusion, or ligation was considered. For microsurgical treatments, lateral suboccipital craniotomy was considered in patients with proximal PICA aneurysms, and midline suboccipital craniotomy in patients with distal PICA aneurysms.
SPSS version 18 was used for statistical analyses (SPSS Inc., Chicago, Illinois, USA). Statistical analyses were performed by use of t-tests and one-way analyses of variance (ANOVAs) for continuous variables, and χ2 or Fisher’s exact test for categorical variables. Differences were considered statistically significant if P values were less than 0.05.
RESULTS
Arteries of the 39 patients were ruptured on admission. Twenty-six patients had proximal PICA aneurysms. Vertebral artery (VA) - PICA junction in 25 cases, anterior medullary segment in one case, while 13 aneurysms were located at distal segments.
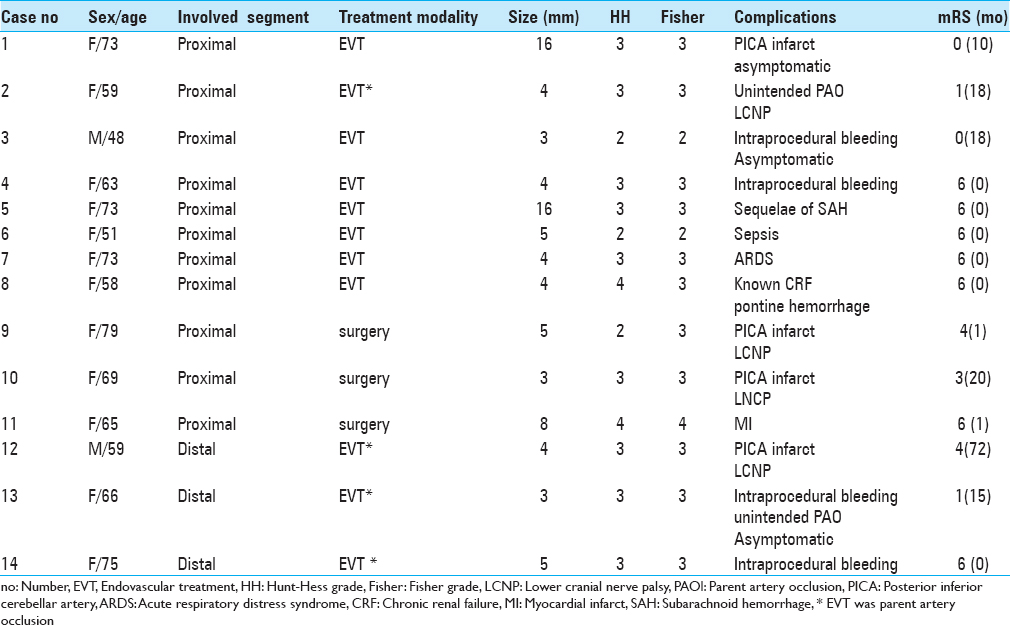
Clinical and radiological results and patient data for included PICA aneurysms are described according to the treatment modalities [
Of the 13 patients with distal PICA aneurysm, 7 patients were treated by EVT (four of them performed parent artery occlusion using detachable coils or N-Butyl Cyanoacrylate glue), and 6 patients were treated by surgery (two of them were performed via trapping without anastomosis). There was no mortality by medical cause. In the EVT group, all aneurysms were completely occluded and had no recurrence. Four patients (57.1%, 4/7) showed a favorable outcome and the mean mRS was 2.63. In the surgical group, there were no treatment failures and recurrence. The treatment-related complication rate and the mean mRS of surgery was significantly lower than those of EVT (0% vs 42.9%, P = 0.046; 2.63 vs 0.33, P = 0.023).
DISCUSSION
PICA aneurysm is very rare, making up approximately 0.49-3.0% of all intracranial aneurysms.[
The PICA showed an anomalous pattern in 4-16% of cases and was classified into anterior medullary, lateral medullary, tonsillomedullar, telovelotonsillar, and cortical segments according to the nearby structure along the course of the aneurysm.[
Surgery of posterior inferior cerebellar artery aneurysms
The type of surgical approach, such as lateral suboccipital, midline subocciptial, and far lateral suboccipital, depends on the location of aneurysm.[
The optimal strategy is to clip the aneurysm with the patent parent artery. The clip-wrap technique can be used to save the parent artery if the distinction of the neck and the parent artery is unclear. Surgical short-segment trapping of the parent artery, which can save more perforators through retrograde flow compared with parent artery occlusion (PAO) using glue injection, can be adjusted without any neurologic sequelae. We did not note any definite neurologic changes after microsurgical parent artery trapping in two of our patients. For ruptured distal PICA aneurysms, the mean initial HH for the microsurgical-treated groups and EVT was 2.17 and 3.00, respectively, and the rate of favorable outcome at surgery groups and EVT were 83.3% and 42.9% each. Also, in terms of mean mRS, microsurgical treatment showed favorable results (0.33 vs. 2.63, P = 0.023).
But jugular tubercle, occipital condyle, and lower cranial nerves provide a narrow corridor; forced brain retraction to expose the neck of aneurysm in a narrow corridor can cause retraction injury and aggravate brain swelling during the acute phase. And the incidence of LCNP while manipulating the PICA is high in patients with a proximal PICA aneurysm through lateral and far-lateral suboccipital approaches.[
Endovascular treatment of posterior inferior cerebellar artery aneurysms
Recently, EVT has become the primary option in the treatment of aneurysms. EVT decreases the risk of direct brainstem injury and reduces the burden of anesthesia in patients with a very poor clinical status or with a poor past medical history. Ryttlefors et al. reported that the survival rate without disability in the EVT group is significantly higher in subarachnoid hemorrhage (SAH) cases compared with surgical treatment.[
Nevertheless, there are also many reports regarding the limitations of EVT, especially with respect to a distal PICA.[
Asymptomatic or symptomatic embolic infarct and unexpected parent artery occlusion, procedure-related thrombus formation can occur during EVT. Occasional LCNP due to brainstem infarct has been reported.[
Other treatment methods
Another treatment method is endovascular or microsurgical VA occlusion. This reduces blood flow at both the PICA and the aneurysm without blocking blood flow to critical perforators and cortical branches, and it allows for collateral vessels to develop; complication rates after sacrificing the PICA are thus decreased.[
Study limitations
This study suffers from the usual limitations that arise from retrospective data reviews. The small number of patients in the subgroups and inherent biases involved in patient selection for treatment preclude making any definitive recommendations. Nevertheless, the results provide some guidance to the clinician when considering EVT or surgery for the treatment of patients with ruptured PICA aneurysms.
CONCLUSIONS
Both surgery and EVT are feasible treatment modalities for preventing rebleeding in the treatment of proximal or distal PICA aneurysms. EVT appears to result in a more favorable clinical outcome in patients with proximal PICA aneurysms, while surgery results in a more favorable outcome in patients with distal PICA aneurysms. Additional experience and follow-up are needed in a larger series to state the efficacy of this strategy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-khayat H, Al-Khayat H, Beshay J, Manner D, White J. Vertebral artery-posteroinferior cerebellar artery aneurysms: Clinical and lower cranial nerve outcomes in 52 patients. Neurosurgery. 2005. 56: 2-10
2. Bacigaluppi S, Bergui M, Crobeddu E, Garbossa D, Ducati A, Fontanella M. Aneurysms of the medullary segments of the posterior-inferior cerebellar artery: Considerations on treatment strategy and clinical outcome. Neurol Sci. 2013. 34: 529-36
3. Chalouhi N, Jabbour P, Starke RM, Tjoumakaris SI, Gonzalez LF, Witte S. Endovascular treatment of proximal and distal posterior inferior cerebellar artery aneurysms. J Neurosurg. 2013. 118: 991-9
4. Hudgins RJ, Day AL, Quisling RG, Rhoton AL, Sypert GW. Garcia-Bengochea F. Aneurysms of the posterior inferior cerebellar artery. A clinical and anatomical analysis. J Neurosurg. 1983. 58: 381-7
5. Isokangas JM, Siniluoto T, Tikkakoski T, Kumpulainen T. Endovascular treatment of peripheral aneurysms of the posterior inferior cerebellar artery. AJNR Am J Neuroradiol. 2008. 29: 1783-8
6. Korja M, Sen C, Langer D. Operative nuances of side-to-side in situ posterior inferior cerebellar artery-posterior inferior cerebellar artery bypass procedure. Neurosurgery. 2010. 67: 471-7
7. Lewis SB, Chang DJ, Peace DA, Lafrentz PJ, Day AL. Distal posterior inferior cerebellar artery aneurysms: Clinical features and management. J Neurosurg. 2002. 97: 756-66
8. Lister JR, Rhoton AL, Matsushima T, Peace DA. Microsurgical anatomy of the posterior inferior cerebellar artery. Neurosurgery. 1982. 10: 170-99
9. Mericle RA, Reig AS, Burry MV, Eskioglu E, Firment CS, Santra S. Endovascular surgery for proximal posterior inferior cerebellar artery aneurysms: An analysis of Glasgow Outcome Score by Hunt-Hess grades. Neurosurgery. 2006. 58: 619-25
10. Orakcioglu B, Schuknecht B, Otani N, Khan N, Imhof HG, Yonekawa Y. Distal posterior inferior cerebellar artery aneurysms: Clinical characteristics and surgical management. Acta Neurochir. 2005. 147: 1131-9
11. Peluso JP, van Rooij WJ, Sluzewski M, Beute GN, Majoie CB. Posterior inferior cerebellar artery aneurysms: Incidence, clinical presentation, and outcome of endovascular treatment. AJNR Am J Neuroradiol. 2008. 29: 86-90
12. Singh RK, Behari S, Kumar V, Jaiswal AK, Jain VK. Posterior inferior cerebellar artery aneurysms: Anatomical variations and surgical strategies. Asian J Neurosurg. 2012. 7: 2-11
13. Song HH, Won YD, Kim YJ, Kim BS. The endovascular management of saccular posterior inferior cerebellar artery aneurysms. Korean J Radiol. 2008. 9: 396-400