- Department of Orthopaedic Surgery, University of Rochester, Rochester, New York, United States
- Department of Orthopaedics, University of Rochester, Rochester, New York, United States
- Department of Orthopaedic Surgery, West Virginia University, Morgantown, West Virginia, United States
- Department of Orthopaedic Surgery, Medstar Orthopaedic Institute, Washington, DC, United States.
Correspondence Address:
Addisu Mesfin, Department of Orthopaedic Surgery, Medstar Orthopaedic Institute, Washington, DC, United States.
DOI:10.25259/SNI_502_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sean Childs1, Wajeeh Bakhsh1, Caroline Thirukumaran2, Sanford Emery3, Paul Rubery2, Addisu Mesfin4. Trends in lumbar interbody fusion: A study of American Board of Orthopedic Surgery (ABOS) candidate data. 15-Dec-2023;14:426
How to cite this URL: Sean Childs1, Wajeeh Bakhsh1, Caroline Thirukumaran2, Sanford Emery3, Paul Rubery2, Addisu Mesfin4. Trends in lumbar interbody fusion: A study of American Board of Orthopedic Surgery (ABOS) candidate data. 15-Dec-2023;14:426. Available from: https://surgicalneurologyint.com/surgicalint-articles/12674/
Abstract
Background: There has been an increase in posterior-based interbody fusions over the past two decades. Our objective was to evaluate trends in interbody fusion use among the American Board of Orthopedic Surgery (ABOS) Part II candidates.
Methods: The ABOS database from 2003 to 2012 was queried for common procedural terminology (CPT) codes indicating lumbar interbody fusion (22,558 anterior lumbar interbody fusion [ALIF] and 22,630 and 22,633 posterior lumbar interbody fusion [PLIF] or transforaminal lumbar interbody fusion [TLIF]). Trends in the use of interbody fusion technique, associated complications, and geographical variation were evaluated. We also queried utilization of the anterior and posterior interbody fusions by the International Classification of Diseases-9 code.
Results: 6841 interbody fusion cases were identified (2329 ALIF and 4512 PLIF/TLIF). There was a significantly higher use of PLIF/TLIF than ALIF over the study period (P P P = 0.01). The overall complication rate was 22.2% (n = 1,519). Vascular-related complications were significantly higher among patients undergoing ALIF (31 vs. 1, P P = 0.03, OR 0.87, CI 95%).
Conclusion: Over the 10-year study period, there has been a significantly increased rate of posterior interbody fusion among candidates taking part II ABOS examination.
Keywords: American Board of Orthopedic Surgery (ABOS), Anterior lumbar interbody fusion (ALIF), Complications, Lumbar interbody fusion, Transforaminal lumbar interbody fusion (TLIF), Trends
INTRODUCTION
Degenerative conditions of the lumbar spine are common. Spinal stenosis is a significant cause of disability, particularly in the elderly population.[
Interbody fusion with instrumentation is often used to address lumbar stenosis. The interbody device allows for load bearing and maintains the foraminal height. [
The objective of this study was to evaluate the trends in the use of lumbar interbody devices for the treatment of lumbar spinal pathology as well as their associated complications among candidates for part II of the American Board of Orthopedic Surgery (ABOS) examination over ten years.
MATERIALS AND METHODS
Data source
In the United States, the ABOS confers board certification on orthopedic surgeons. Surgical cases performed during a predetermined 6-month period are submitted for review. The data submitted for each case includes International Classification of Diseases (ICD) codes, CPT codes, patient age and gender, geographical region of the surgeon’s practice, surgical complications, fellowship training of the surgeon, and a brief verbal description of the procedure and indications. These cases are entered into a secure database maintained on behalf of the ABOS by Data Harbor Solutions (Hinsdale, Illinois). This de-identified data is the subject of our study and has been used in other previous work.
Study cohort
The ABOS database was queried for cases of lumbar interbody fusion using the CPT codes 22,558 ALIF, 22,630 PLIF, and 22,633 TLIF between 2003 and 2012. As the CPT code for transforaminal interbody fusion was combined with that for PLIF (CPT 22630) after 2012, these two procedures were grouped for the analysis portion of this study. Surgeon’s geographical location, associated ICD-9 codes, and perioperative complications were gathered.
Key variables
The outcomes of interest were the rates of each surgery type (computed as the number of surgeries per 100 surgeons), the type of surgery (specified as a categorical variable with ALIF and PLIF/TLIF categories), and whether or not a complication was reported (specified as a yes/no variable). The independent variables of interest were the geographic location (categorized as regions of the United States), principal diagnosis (categorized based on the listed ICD code), and the year of surgery. Our analytic models also controlled for covariates such as age and gender that were likely to confound the association of interest.
Statistical analysis
The proportions of lumbar spinal pathology treated with ALIF (CPT 22558) and posterior/transforaminal interbody fusion (CPT 22,530 and CPT 22,633) were determined. We used Chi-square tests and student t-tests to test differences in the distribution of key variables across the surgical groups. We constructed multivariable logistic regression models to examine whether the geographic location and principal diagnosis were significant predictors of the type of surgery and the risk of complications. The statistical significance was set at P <0.05.
RESULTS
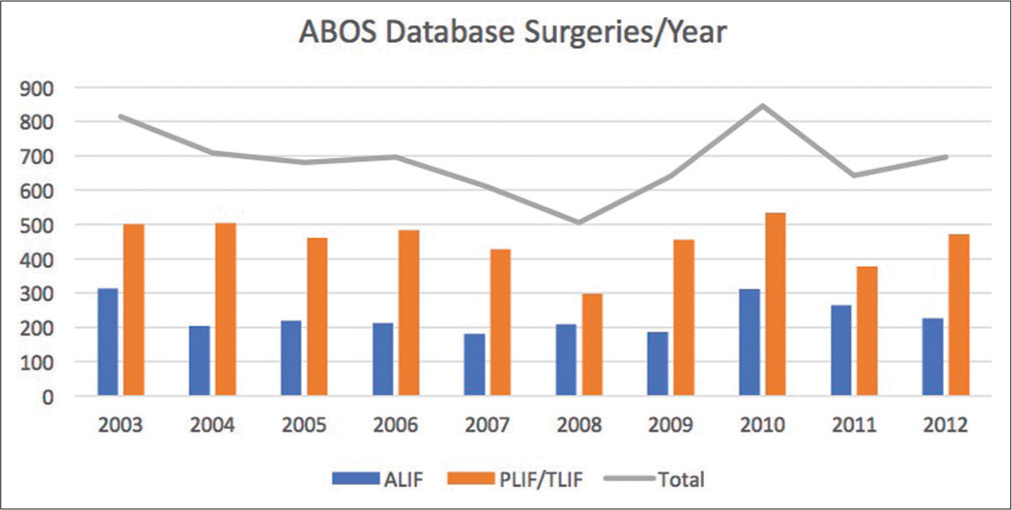
From 2003 to 2012, orthopedic surgeons taking the ABOS part II examination submitted 6841 cases of lumbar interbody fusion. Of the cases submitted, a total of 2329 (34%) cases were ALIFs, and 4512 (66%) were performed from a posterior approach. There was a significantly higher rate of PLIF/TLIF compared to ALIF during the study (P <0.01) [
Regional variations
Anterior-based lumbar interbody fusion was found to be reported most frequently by surgeons practicing in the Southwest (n = 675), followed by surgeons in the Midwest region (n = 472) of the United States. Anterior-based interbody fusion was reported least frequently by surgeons in the Northwest (n = 77) and Southeast (n = 270) regions. PLIF was reported most frequently by surgeons practicing in the Southern (n = 861) and Northeast regions (n = 808). As compared to patients in the Midwest, those in the Northwest had significantly higher odds of undergoing PLIF/TLIF (odds ratio [OR]: 4.79, 95% confidence interval [CI]: 3.61–6.35, P <0.001) and those in the Southwest had significantly lower odds of PLIF/TLIF (OR: 0.81, 95% CI: 0.69–0.95, P = 0.01).
Common diagnoses
The five most commonly listed ICD-9 codes were as follows: spinal stenosis of the lumbar region without neurogenic claudication (724.02), degeneration of lumbar/lumbosacral intervertebral disc (722.52), acquired spondylolisthesis (738.4), thoracic or lumbosacral neuritis/radiculitis (724.4), and displacement of thoracic/lumbar intervertebral disc without myelopathy (722.1). As compared to patients with degenerative disc disease (722.52), patients with ICD-9 diagnoses of lumbar stenosis (724.02) underwent significantly higher numbers of PLIF/TLIF when compared to ALIF (2135 vs. 601; P <0.01) and were at greater odd of undergoing this procedure (P <0.001, OR 2.33, CI 95%: 2.02–2.68).
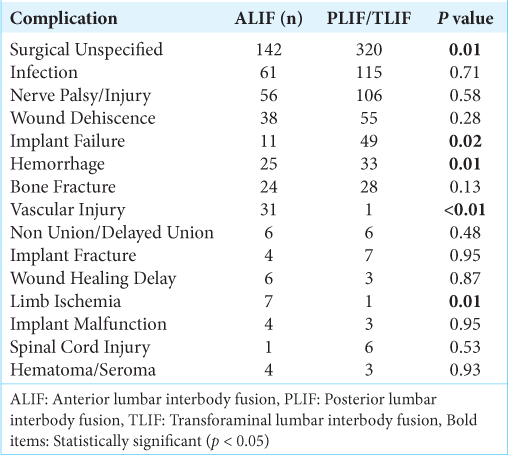
Complications [ Table 1 ]
The overall complication rate for the study cohort was 22% (n = 1,519). The five most common reported complications were as follows: unspecified surgical complications (n = 462), infection (n = 176), nerve palsy/injury (n = 162), wound dehiscence (n = 93), and implant failure (n = 60). There were no significant differences in the rates of these complications between patients undergoing PSIF/TLIF or ALIF (P> 0.05, [
DISCUSSION
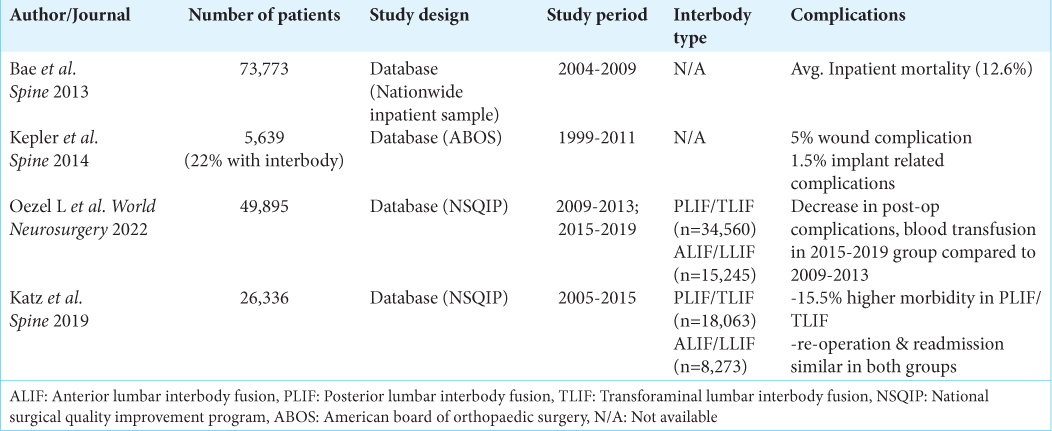
Degenerative lumbar conditions are a common source of disability and societal economic burden. Lumbar spinal decompression and interbody fusion have become an increasingly common procedure in these patients and has been shown to yield good results. Few studies have examined the trends in surgical approaches used during interbody fusion among recent orthopedic graduates as well as their associated complications and economic burden [
Our study reveals that during our 10-year study period, there was a significantly higher use of PLIF/TLIF when compared with ALIF among candidates taking part II ABOS examination. There were significant geographic differences in the use of surgical approaches for lumbar interbody fusion as well, with the Northwest and Southeast having the highest levels of PLIF/TLIF use while the southwest had the lowest. Lumbar stenosis and degenerative spondylolisthesis diagnoses were associated with the highest rates of PLIF/TLIF among part II ABOS candidates during the study period. In addition, there was a 22% rate of complications reported by candidates during this study period. Vascular-related complications were significantly higher among patients with ALIF. In addition, patients undergoing PLIF/TLIF were also found to have significantly lower odds of experiencing a complication within the perioperative or postoperative time course.
CONCLUSION
We found that posterior interbody fusion is more commonly performed than anterior interbody fusion among orthopedic spinal surgeons taking part II of the ABOS certification exam during our 10-year study period. Complications were found to be lower among patients undergoing PLIF/TLIF, and vascular-related complications were found to be significantly higher among patients undergoing anterior interbody fusion.
Ethical approval
Due to the deidentified nature of the database with no patient or surgeon identifiers present, an IRB approval was not obtained.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
Addisu Mesfin: Travel/lodging: Medtronic, NuVasive.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine lumbar spine study. Spine (Phila Pa 1976). 2005. 30: 936-43
2. Bae HW, Rajaee SS, Kanim LE. Nationwide trends in the surgical management of lumbar spinal stenosis. Spine (Phila Pa 1976). 2013. 38: 916-26
3. Deyo RA. Treatment of lumbar spinal stenosis: A balancing act. Spine J. 2010. 10: 625-7
4. Garrett WE, Swiontkowski MF, Weinstein JN, Callaghan J, Rosier RN, Berry DJ. American board of orthopaedic surgery practice of the orthopaedic surgeon: Part-II, certification examination case mix. J Bone Joint Surg Am. 2006. 88: 660-7
5. Katz AD, Mancini N, Karukonda T, Greenwood M, Cote M, Moss IL. Approach-based comparative and predictor analysis of 30-day readmission, reoperation, and morbidity in patients undergoing lumbar interbody fusion using the ACS-NSQIP Dataset. Spine (Phila Pa 1976). 2019. 44: 432-41
6. Katz JN, Harris MB. Clinical practice. Lumbar spinal stenosis. N Engl J Med. 2008. 358: 818-25
7. Kepler CK, Vaccaro AR, Hilibrand AS, Anderson DG, Rihn JA, Albert TJ. National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976). 2014. 39: 1584-9
8. Oezel L, Okano I, Hughes AP, Sarin M, Shue J, Sama AA. Longitudinal trends of patient demographics and morbidity of different approaches in lumbar interbody fusion: An analysis using the American college of surgeons national surgical Quality improvement program database. World Neurosurg. 2022. 164: e183-93