- Department of Neurosurgery American University of Beirut Medical Center, Beirut, Lebanon.
- Department of Oncology, American University of Beirut Medical Center, Beirut, Lebanon.
Correspondence Address:
Houssein Darwish, Department of Neurosurgery, American University of Beirut Medical Center, Beirut, Lebanon.
DOI:10.25259/SNI_379_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamad El Houshiemy1, Shadi Abdelatif Bsat1, Ryan El Ghazal1, Charbel Moussalem1, Ali Amine1, Sarah Kawtharani1, Adham Halaoui1, Hazem Assi2, Houssein Darwish1. Trigeminal neuralgia secondary to onyx embolization of a right occipital arteriovenous malformation. 28-Jun-2021;12:318
How to cite this URL: Mohamad El Houshiemy1, Shadi Abdelatif Bsat1, Ryan El Ghazal1, Charbel Moussalem1, Ali Amine1, Sarah Kawtharani1, Adham Halaoui1, Hazem Assi2, Houssein Darwish1. Trigeminal neuralgia secondary to onyx embolization of a right occipital arteriovenous malformation. 28-Jun-2021;12:318. Available from: https://surgicalneurologyint.com/surgicalint-articles/10918/
Abstract
Background: Trigeminal neuralgia is a debilitating chronic condition characterized by severe recurrent hemifacial pain which is often caused by compression of the trigeminal nerve by an adjacent vessel loop. Microvascular decompression (MVD) surgery is an effective procedure that can lead to full symptomatic relief. Intracranial arteriovenous malformations (AVMs) are primarily congenital abnormalities that may be asymptomatic or manifest as seizures or focal neurologic deficits. They may cause intracranial bleeding and hence are promptly treated, often by endovascular embolization. This procedure is safe but may have a multitude of unpredictable complications.
Case Description: A 33-year-old female presented with medically refractory trigeminal neuralgia secondary to Onyx embolization of a right occipital AVM 3 years prior. She underwent surgical exploration and MVD of the trigeminal nerve root which was found to be compressed by the previously embolized superior cerebellar artery. The procedure was successful and full symptomatic resolution was immediately achieved.
Conclusion: Postprocedural trigeminal neuralgia is a procedural complication of Onyx endovascular embolization. It may be treated by MVD surgery regardless of the presence or absence of a compressive vascular loop on imaging.
Keywords: Adverse events, Arteriovenous malformation, Embolization, Microvascular decompression, Onyx, Trigeminal neuralgia
INTRODUCTION
Trigeminal neuralgia is a chronic condition characterized by severe, often unilateral, lancinating pain in the trigeminal nerve distribution of the face that is brief and recurrent. It is estimated to affect approximately 4/100,000 people/year in the United States.[
Intracranial arteriovenous malformations (AVMs), on the other hand, are rare primarily congenital vascular abnormalities estimated to affect <0.01% of the general population.[
Onyx liquid endovascular embolization has recently emerged as a versatile therapeutic choice. Often, it is employed perioperatively to reduce AVM nidus size; however, it is also a valid standalone curative modality in select cases.[
We present the case of a 33-year-old female with trigeminal neuralgia secondary to Onyx endovascular embolization of a right occipital AVM 3 years prior which we successfully treated by MVD surgery despite no evidence of a compressive vessel loop on imaging.
CASE DESCRIPTION
Initial presentation
A 33-year old female, known to have a history of right occipital AVM treated by Onyx endovascular embolization 3 years prior, presented with severe right-sided trigeminal neuralgia and occipital lobe visual seizures. Embolization was done at an outside hospital and right hemifacial pain began after it. She failed three lines of medical treatment since then and has been maintained on carbamazepine 800 mg twice daily with no improvement in pain.
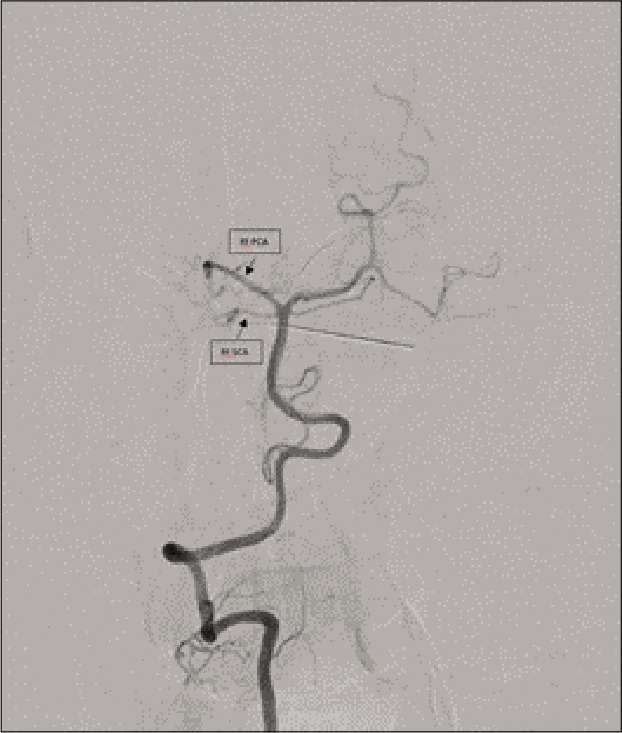
She underwent a diagnostic cerebral angiography which showed total occlusion of the previously embolized AVM along with distal occlusion of the right posterior cerebellar artery and SCA [
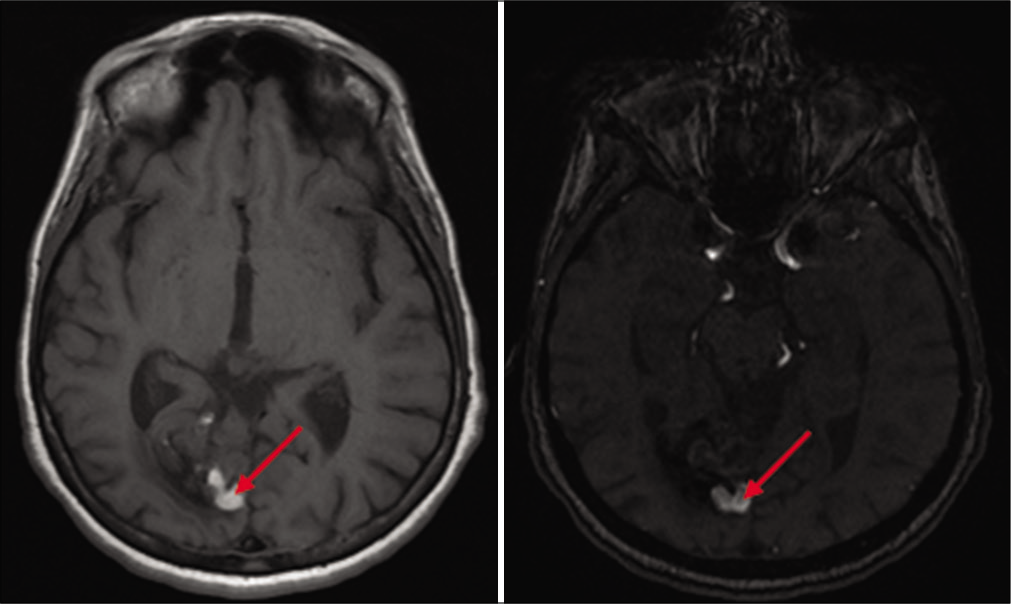
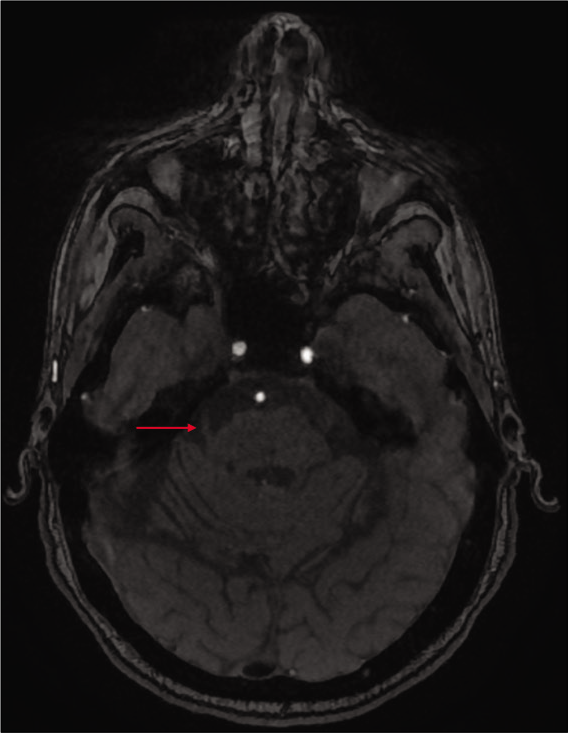
Subsequent brain MRI showed the previously embolized AVM in the right occipital lobe [
Operative procedure
One week after the angiogram, the patient underwent successful Jannetta MVD of the trigeminal nerve. She was positioned in lateral position and a retroauricular lazy-S skin incision was made two finger-widths away from the ear for a retrosigmoid approach. The flap was reflected from medial to lateral and the paravertebral muscles were elevated subperiosteally. A burr hole was made at the asterion just below the junction of the transverse and the sigmoid sinuses and a retrosigmoid craniotomy was done using a footplate. The craniotomy was enlarged by drilling the bone over the transverse and sigmoid sinuses. The mastoid air cells were covered with bone wax to avoid postoperative CSF leakage. The dura was then opened and reflected over the transverse and the sigmoid sinuses, and CSF was drained from the lateral cerebellomedullary cistern to relax the cerebellum.
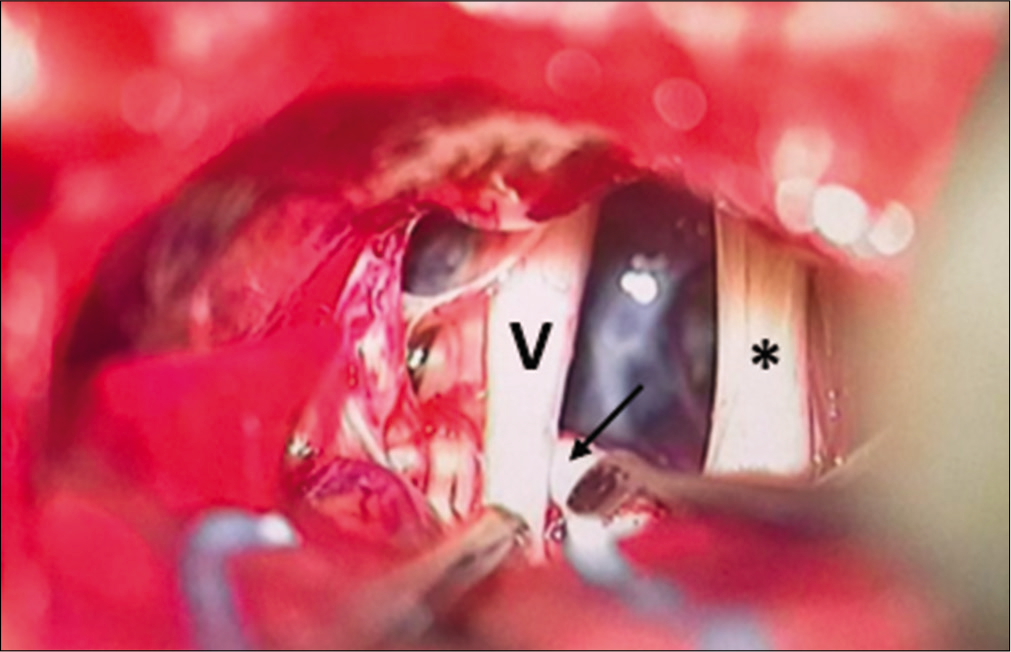
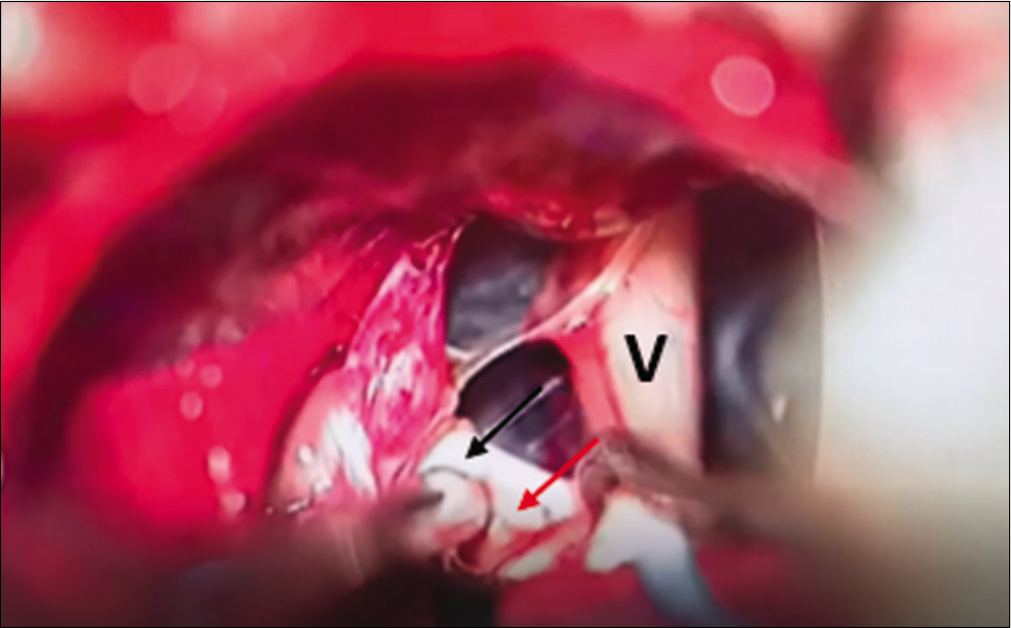
Initial inspection of the cerebellopontine angle showed the seventh and eighth nerve complex. More CSF drainage was attempted to provide additional working space and the trigeminal nerve was subsequently localized and freed from the surrounding arachnoid adhesions. A whitish tubular structure that resembled an empty vessel was noticed crossing and abutting the trigeminal nerve root entry zone [
The SCA was hence carefully dissected off the trigeminal nerve root entry zone and the brain stem, creating space for two small pieces of Teflon sponges which were inserted to separate the vessel from the mentioned structures it was compressing [
The patient did well postoperatively and left the hospital 2 days later with no reported hemifacial pain. She was seen 2 weeks after the surgery in clinic with full resolution of trigeminal neuralgia and her medication dosage was halved.
DISCUSSION
Onyx endovascular embolization is routinely performed as part of the management plan of intracerebral AVMs. It is deemed safe and effective, but it is in fact not without risk, and many adverse events have been described in the literature. A large retrospective study by Sato et al. found that complications arose in 13.1% of procedures,[
How such CN palsies arise after endovascular embolization is not clear, but many mechanisms have been proposed to explain this phenomenon, which is most likely due to downstream vascular effects of the procedure. As Nyberg et al. hypothesized, the transient CN dysfunctions they encountered may have been due to axonotmetic traction injuries during microcatheter removal from the Onyx cast.[
Any of these mechanisms, alone or in combination, may have contributed to the presentation we have encountered. The trigeminal neuralgia in our patient can be safely attributed to the embolization procedure as it began immediately after it. Another supporting piece of evidence is the fact that during the exploratory surgery, the previously embolized SCA, now empty, was found abutting the trigeminal nerve, and decompression lead to prompt resolution of symptoms.
CONCLUSION
By reporting this case, we hope to add to the repertoire of known adverse events attributable to Onyx embolization. We also aim to shed light on possible mechanisms of this event, which, if generalizable to other procedures involving different intracranial arteries, may provide an explanation to some of the more obscure complications and CN palsies. We also show that MVD is a valid and highly effective treatment of trigeminal neuralgia even when no compressing vessel loop is identifiable on imaging, lending credence to the mostly vascular etiology of the condition.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
References
1. Berman MF, Sciacca RR, Pile-Spellman J, Stapf C, Connolly ES, Mohr JP. The epidemiology of brain arteriovenous malformations. Neurosurgery. 2000. 47: 389-96
2. Buell TJ, Ding D, Starke RM, Crowley RW, Liu KC. Embolization-induced angiogenesis in cerebral arteriovenous malformations. J Clin Neurosci. 2014. 21: 1866-71
3. Derdeyn CP, Zipfel GJ, Albuquerque FC, Cooke DL, Feldmann E, Sheehan JP. Management of brain arteriovenous malformations: A scientific statement for healthcare professionals from the American heart association/ American stroke association. Stroke. 2017. 48: e200-24
4. Hofmeister C, Stapf C, Hartmann A, Sciacca RR, Mansmann U, terBrugge K. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke. 2000. 31: 1307-10
5. Jones MR, Urits I, Ehrhardt KP, Cefalu JN, Kendrick JB, Park DJ. A comprehensive review of trigeminal neuralgia. Curr Pain Headache Rep. 2019. 23: 74
6. Katusic S, Beard CM, Bergstralh E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol. 1990. 27: 89-95
7. Mineura K, Sasajima H, Itoh Y, Kowada M, Tomura N, Goto K. Development of a huge varix following endovascular embolization for cerebellar arteriovenous malformation. A case report. Acta Radiol. 1998. 39: 189-92
8. Nyberg EM, Chaudry MI, Turk AS, Turner RD. Transient cranial neuropathies as sequelae of Onyx embolization of arteriovenous shunt lesions near the skull base: Possible axonotmetic traction injuries. J Neurointerv Surg. 2013. 5: e21
9. Ozluoglu LN, Koycu A, Jafarov S, Hizal E, Boyvat F. Facial palsy following embolization of a dural arteriovenous fistula. Eur Arch Otorhinolaryngol. 2016. 273: 2843-6
10. Pierot L, Cognard C, Herbreteau D, Fransen H, van Rooij WJ, Boccardi E. Endovascular treatment of brain arteriovenous malformations using a liquid embolic agent: Results of a prospective, multicentre study (BRAVO). Eur Radiol. 2013. 23: 2838-45
11. Quinn JC, Mittal N, Baisre A, Cho ES, Sharer LR, Gandhi C. Vascular inflammation with eosinophils after the use of n-butyl cyanoacrylate liquid embolic system. J Neurointerv Surg. 2011. 3: 21-4
12. Sato K, Matsumoto Y, Tominaga T, Satow T, Iihara K, Sakai N. Complications of endovascular treatments for brain arteriovenous malformations: A nationwide surveillance. AJNR Am J Neuroradiol. 2020. 41: 669-75
13. Sharma A, Jagetia A, Loomba P, Singh D, Tandon M. Delayed brain abscess after embolization of arterio-venous malformation: Report of two cases and review of literature. Neurol India. 2011. 59: 620-3
14. Solli E, Jumah F, Narayan V, Quinoa T, Xiong Z, Gupta G. Resection of a posterior fossa arteriovenous malformation complicated by leaked Onyx: A case report and review of literature. Acta Neurochir (Wien). 2020. 162: 923-8
15. Wróbel-Wiśniewska G, Jaskólski DJ, Zawirski M. Neuralgia nerwu trójdzielnego po embolizacji wewnatrzczaszkowego oponowego zniekształcenia tetniczo-zylnego. Opis przypadku [Trigeminal neuralgia due to lengthy AVM treatment. A case report]. Neurol Neurochir Pol. 2003. 37: 259-63
16. Yamoto T, Nishibayashi H, Ogura M, Nakao N. Three-dimensional morphology of the superior cerebellar artery running in trigeminal neuralgia. J Clin Neurosci. 2020. 82: 9-12