- Department of Neurosurgery, King Fahad Hospital, Jeddah, Saudi Arabia
- Division of Neurosurgery, Neuroscience Center, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia.
Correspondence Address:
Abdulgadir Talal Atteiah, Department of Neurosurgery, King Fahad Hospital Jeddah, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_94_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulgadir Talal Atteiah1, Mosab Abbas2, Taghreed Abdulhameed Al-Sinani1. Tuberculoma mimicking en-plaque meningioma in a 45-year-old male: A case report. 05-Apr-2024;15:118
How to cite this URL: Abdulgadir Talal Atteiah1, Mosab Abbas2, Taghreed Abdulhameed Al-Sinani1. Tuberculoma mimicking en-plaque meningioma in a 45-year-old male: A case report. 05-Apr-2024;15:118. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12845
Abstract
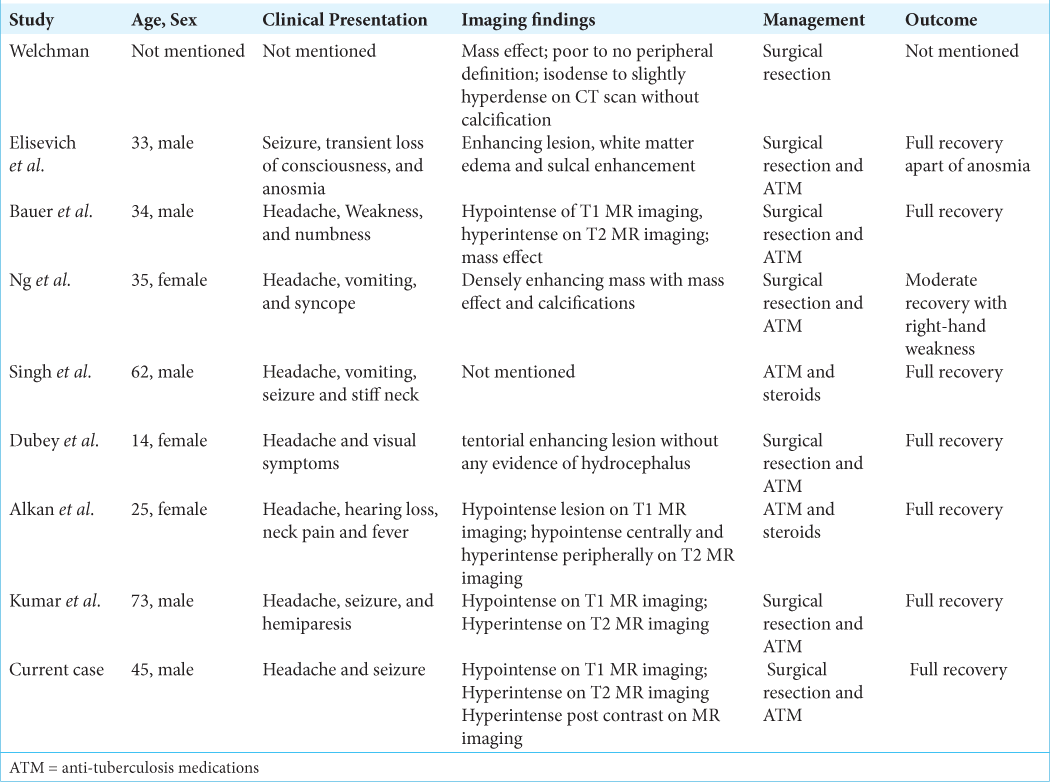
Background: Tuberculoma mimicking en-plaque meningioma is a rare variant of tuberculoma. A few cases were reported in the literature. The radiological appearance can be mistakenly diagnosed as en-plaque meningioma.
Case Description: We report a rare case of a 45-year-old male with tuberculoma mimicking en-plaque meningioma who underwent surgical excision followed by anti-tuberculosis (TB) medications. Follow-up brain imaging after three months showed a favorable outcome.
Conclusion: Tuberculoma mimicking en-plaque meningioma should be considered in the differential diagnosis where TB is endemic.
Keywords: En-plaque tuberculoma, Leptomeningeal tuberculoma, Tuberculoma, Tuberculosis
INTRODUCTION
Tuberculosis (TB) infection of the central nervous system (CNS) carries a high risk of mortality rate and can lead to serious neurological complications and long-term consequences.[
CASE REPORT
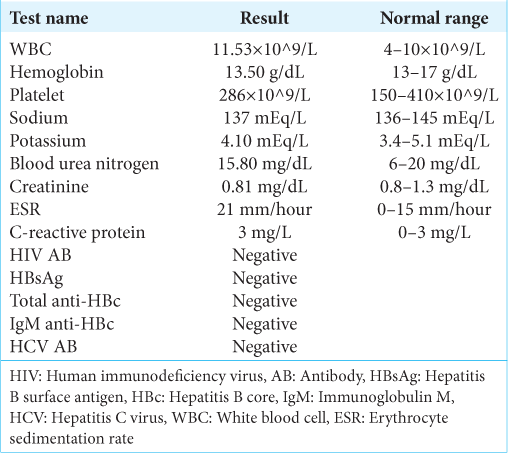
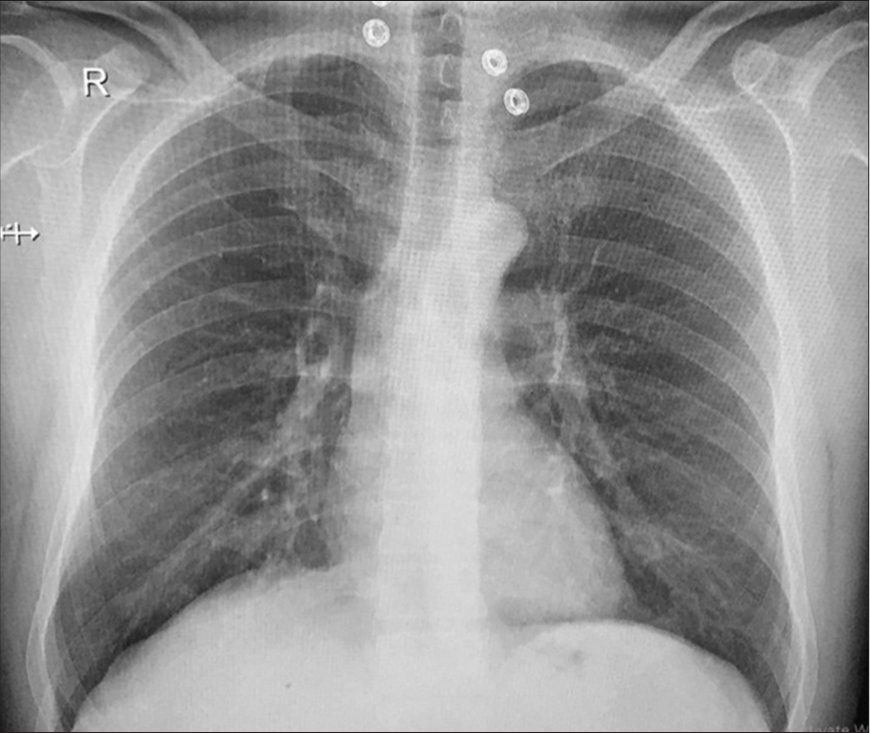
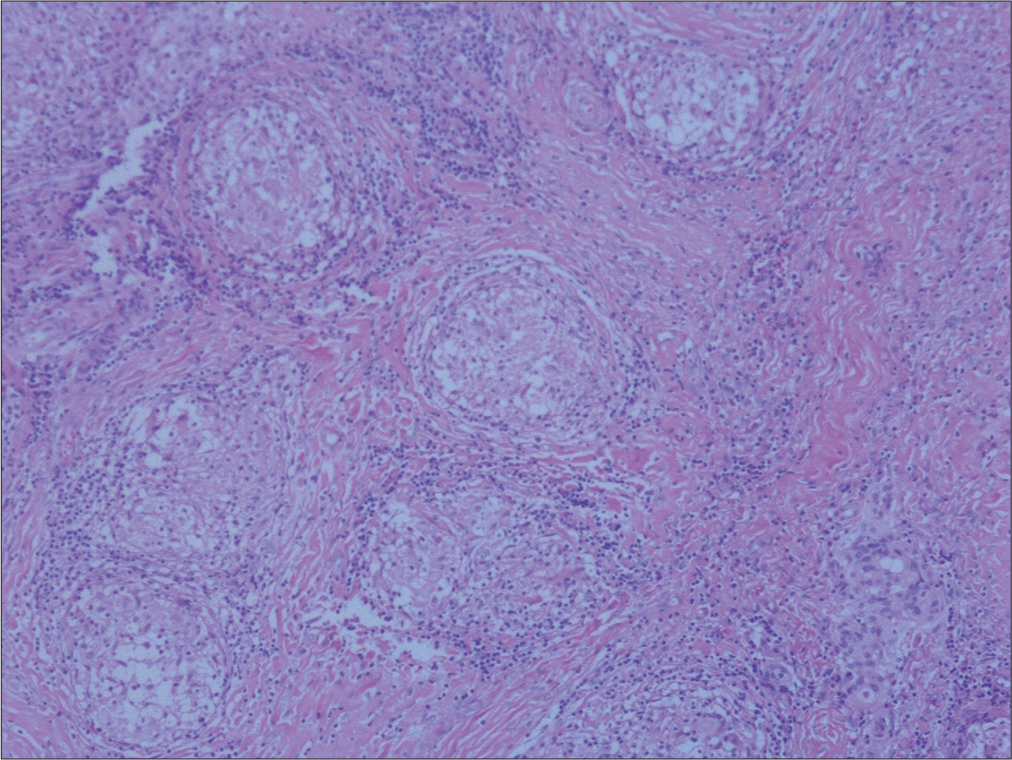
This patient is a 45-year-old male patient who was previously well and immunocompetent. He had a new onset of generalized tonic-clonic convulsion. He denied having head trauma, fever, previous similar attacks, contact with sick patients, and malignancy. Neurological examination was normal without papilledema. Initial blood investigations showed a slightly abnormal raise in white blood cells: 11.53 × 10^9/L (normal range: 4–10 × 10^9/L) and also slightly abnormal elevation erythrocyte sedimentation rate: 21 mm/hour (normal range: 0–15 mm/hour); otherwise, the rest of laboratory results were within the normal range including electrolytes and C-reactive protein [
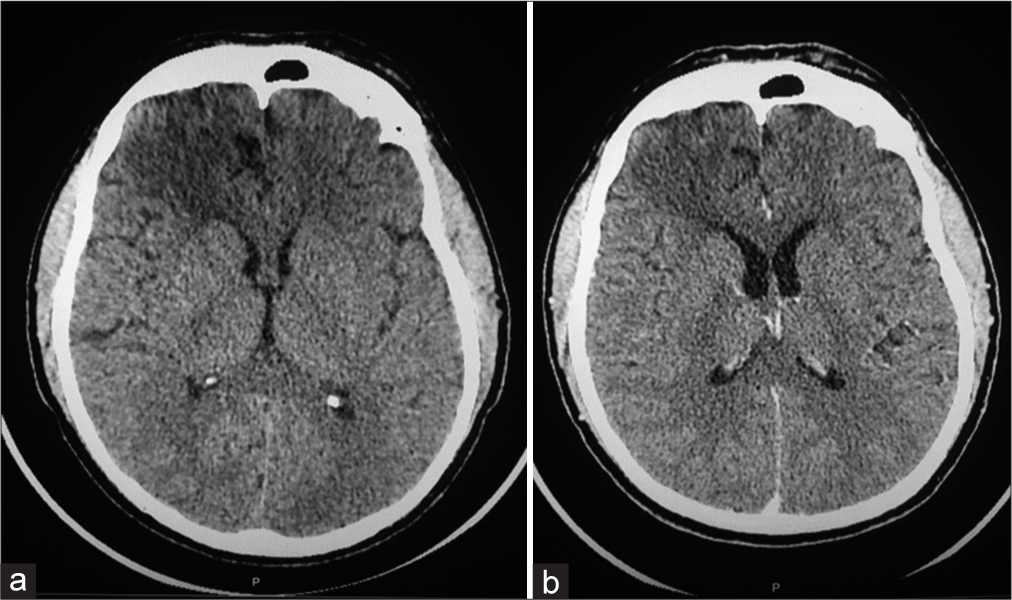
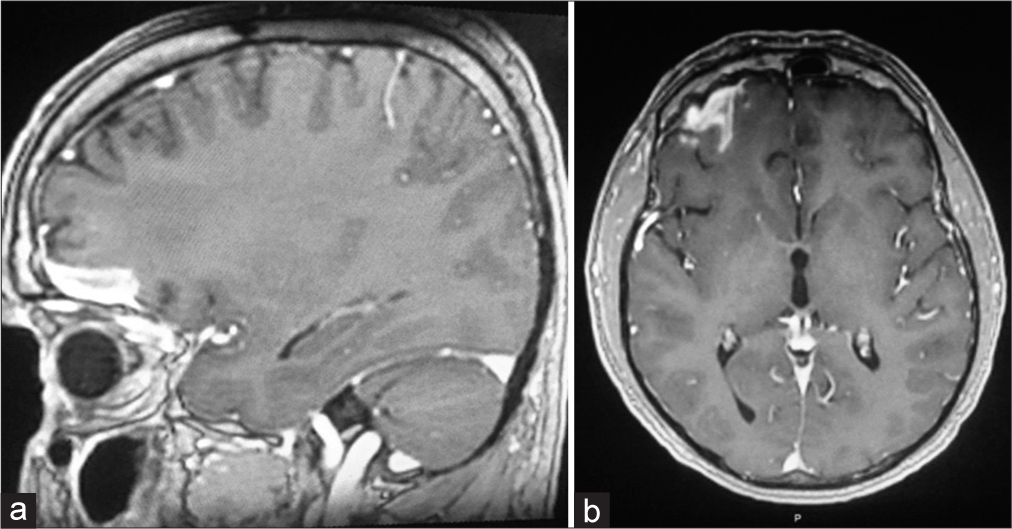
Computerized tomography (CT) scan of the brain without contrast showed a hypodense signal in the right frontal lobe involving the gray and white matter without mass effect or sulcal effacement that was not enhancing post-contrast administration [
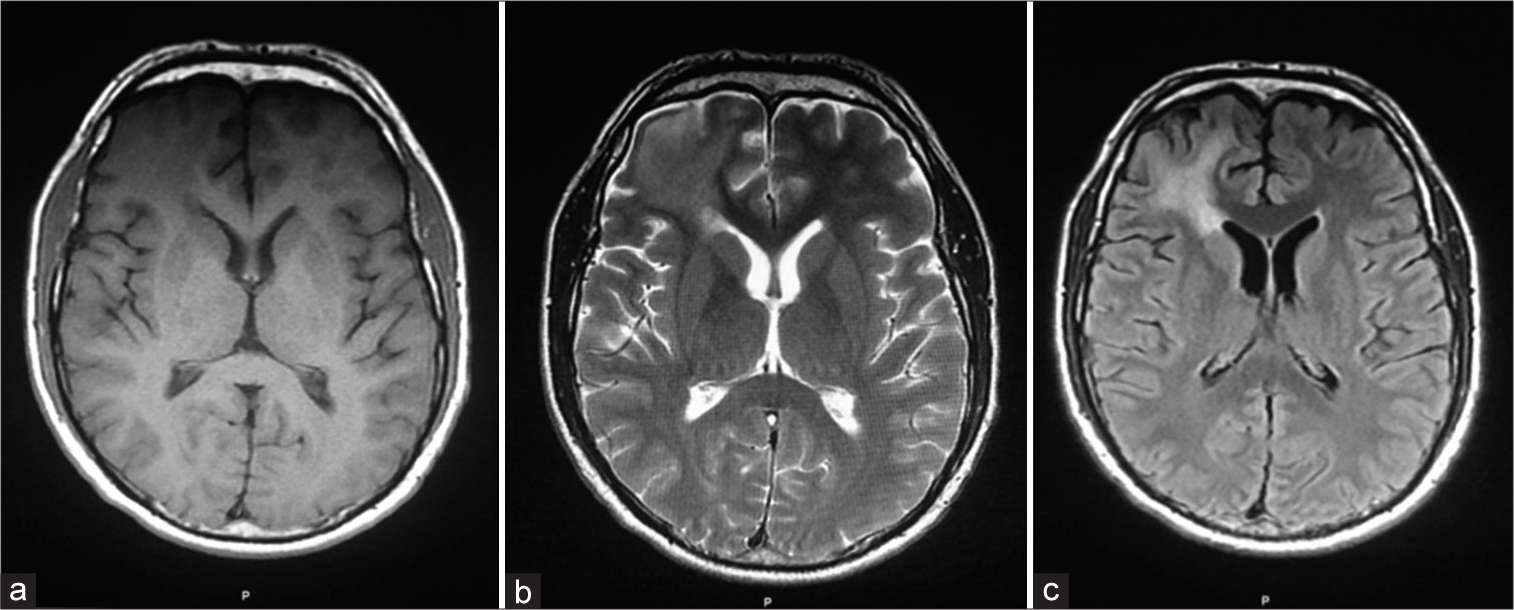
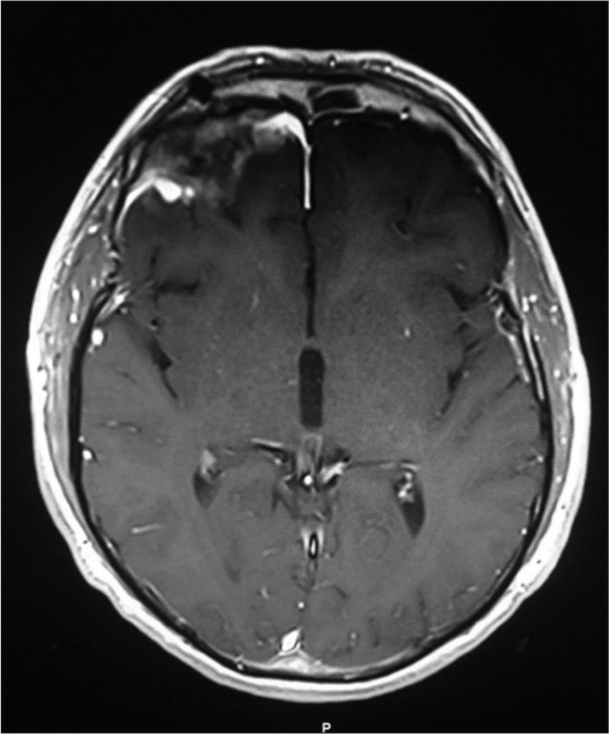
At three months of follow-up visits, MR imaging of the brain showed total resection of the tuberculoma without recurrence, and the patient was well [
DISCUSSION
CNS TB is more frequently diagnosed in developing countries in comparison with other developed countries. [
CONCLUSION
Tuberculoma mimicking en-plaque meningioma should be considered in the differential diagnosis where TB is endemic. The anti-TB treatment is the effective management of en-plaque tuberculoma when the diagnosis is made.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alkan A, Parlak M, Baysal T, Sıgırcı A, Kutlu R, Altınok T. En-plaque-tuberculomas-of-tentorium-in-a-pregnant-woman-followup--2003. Eur Radiol. 2003. 13: 1190-3
2. Aggarwal A, Patra DP, Gupta K, Sodhi HB. Dural tuberculoma mimicking meningioma: A clinicoradiologic review of dural en-plaque lesions. World Neurosurg. 2016. 88: 686.e1-7
3. Arseni C. Two hundred and one cases of intracranial tuberculoma treated surgically. J Neurol Neurosurg Psychiatry. 1958. 21: 308-11
4. Artico M, De Caro GM, Carloia S, Salvati M, D’Ambrosio M, Delfini R. Advances in diagnosis, treatment and prognosis of intracerebral tuberculomas in the last 50 years. Report of 21 cases. Neurochirurgie. 1999. 45: 129-33
5. Bauer J, Johnson RF, Levy JM, Pojman DV, Ruge JR. Tuberculoma presenting as an en plaque meningioma. Case report. J Neurosurg. 1996. 85: 685-8
6. Bernaerts A, Vanhoenacker FM, Parizel PM, Van Goethem JW, van Altena R, Laridon A. Tuberculosis of the central nervous system: Overview of neuroradiological findings. Eur Radiol. 2003. 13: 1876-90
7. Chang CM, Chan FL, Yu YL, Huang CY, Woo E. Tuberculous meningitis associated with meningeal tuberculoma. J R Soc Med. 1986. 79: 486-7
8. Dastur HM, Desai AD. A compartive study of brain tuberculomas and gliomas based upon 107 case records of each. Brain. 1965. 88: 375-96
9. Dubey S, Devi BI, Jawalkar VK, Bhat DI. Tuberculoma en plaque: A case report. Neurol India. 2002. 50: 497-9
10. Elisevich K, Arpin EJ. Tuberculoma masquerading as a meningioma. Case report. J Neurosurg. 1982. 56: 435-8
11. Fishbein NJ, Dillon WP, Bakovich AJ, editors. Teaching atlas of brain imaging. United States: Thieme; 2000. p.
12. Gray F. Bacterial infections. Brain Pathol. 1997. 7: 629-47
13. Gupta RK, Jena A, Singh AK, Sharma A, Puri V, Gupta M. Role of magnetic resonance (MR) in the diagnosis and management of intracranial tuberculomas. Clin Radiol. 1990. 41: 120-7
14. Harder E, Al-Kawi MZ, Carney P. Intracranial tuberculoma: Conservative management. Am J Med. 1983. 74: 570-6
15. Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical response to tuberculostatic chemotherapy: Case report and review of the literature. Neurosurg Q. 1999. 9: 154-61
16. Jacques C, Boukobza M, Polivka M, Ferrario A, George B, Merland JJ. Cranial epidural tuberculoma. A case report. Acta Radiol. 2000. 41: 367-70
17. Jamjoom ZA, Assaf HM, Hamid F, Haddad Q, Jamjoom AH, Naim-Ur-Rahman . Intracranial epidural tuberculoma presenting as a scalp swelling. Surg Neurol. 1994. 42: 322-5
18. Kumar J, Mallik J, Strickland B, Harsh V, Kumar A. Intracranial en-plaque tuberculoma impersonating en-plaque meningioma: Case report and brief review of literature. Asian J Neurosurg. 2017. 12: 576
19. Mayers MM, Kaufman DM, Miller MH. Recent cases of intracranial tuberculomas. Neurology. 1978. 28: 256-60
20. Monteiro R, Carneiro JC, Costa C, Duarte R. Cerebral tuberculomas-A clinical challenge. Respir Med Case Rep. 2013. 9: 34-7
21. Ng SH, Tang LM, Lui TN, Ko SF, Wong HF, Wai YY. Tuberculoma en plaque: CT. Neuroradiology. 1996. 38: 453-5
22. Okada T, Yoshida T, Asai T, Shintani A. Unusual meningeal tuberculoma-Case report. Neurol Med Chir (Tokyo). 1993. 33: 710-2
23. Salgado P, Del Brutto OH, Talamas O, Zenteno MA, Rodríguez-Carbajal J. Intracranial tuberculoma: MR imaging. Neuroradiology. 1989. 31: 299-302
24. Singh KK, Nair MD, Radhakrishnan K, Tyagi JS. Utility of PCR assay in diagnosis of en-plaque tuberculoma of the brain. J Clin Microbiol. 1999. 37: 467-70
25. Sinh G, Pandya SK, Dastur DK. Pathogenesis of unusual intracranial tuberculomas and tuberculous space-occupying lesions. J Neurosurg. 1968. 29: 149-59
26. Teoh R, Humphries MJ, O’Mahony G. Symptomatic intracranial tuberculoma developing during treatment of tuberculosis: A report of 10 patients and review of the literature. Q J Med. 1987. 63: 449-60
27. Uysal G, Köse G, Güven A, Diren B. Magnetic resonance imaging in diagnosis of childhood central nervous system tuberculosis. Infection. 2001. 29: 148-53
28. Vengsarkar US, Pisipaty RP, Parekh B, Panchal VG, Shetty MN. Intracranial tuberculoma and the CT scan. J Neurosurg. 1986. 64: 568-74
29. Weisberg L, Nice C, editors. Cerebral computed tomography. Philadelphia, PA: Saunders; 1988. p.
30. Welchman JM. Computerized tomography of intracranial tuberculomata. Clin Radiol. 1979. 30: 567-73
31. Witrak BJ, Ellis G. Intracranial tuberculosis: Manifestations on computerized tomography. South Med J. 1985. 78: 386-92