- Department of Neurosurgery, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
Correspondence Address:
Muhammad Arifin Parenrengi, Department of Neurosurgery, Faculty of Medicine Universitas Airlangga, Dr. Soetomo General Academic Hospital, Surabaya, East Java, Indonesia.
DOI:10.25259/SNI_606_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmad Data Dariansyah, Wihasto Suryaningtyas, Muhammad Arifin Parenrengi. Tuberculoma mimicking postoperative VP shunt seeding of craniopharyngioma: A rare case report. 06-Sep-2021;12:450
How to cite this URL: Ahmad Data Dariansyah, Wihasto Suryaningtyas, Muhammad Arifin Parenrengi. Tuberculoma mimicking postoperative VP shunt seeding of craniopharyngioma: A rare case report. 06-Sep-2021;12:450. Available from: https://surgicalneurologyint.com/surgicalint-articles/11091/
Abstract
Background: Tuberculosis (TB) is still a big problem in developing and TB endemic countries such as Indonesia. The most common manifestations of TB in the central nervous system are tuberculous meningitis and tuberculoma. In developing and TB endemic countries, tuberculomas account for 33% of intracranial space-occupying lesions. Isolated tuberculoma without systemic TB is rarely seen. On physical and radiological examination, tuberculoma often gives an atypical appearance. From imaging, tuberculoma often mimics another intracranial tumor. Oftentimes the accurate diagnosis can only be made after postoperative histopathological and microbiology examination.
Case Description: An 11-year-old, Indonesian girl has been complaining persistent headache in the past 3 years. The patient had a history of surgical excision of craniopharyngioma 8 years ago, and placement of ventriculoperitoneal shunt due to postoperative hydrocephalus. Patient was immunocompetent with no sign of systemic TB nor tuberculous meningitis. Brain magnetic resonance imaging (MRI) revealed a 4 × 2.3 × 2.1 cm mass surrounding the ventricular drain which was attached in the anterior horn of the right lateral ventricle to the right frontal cortex. From dynamic susceptibility contrast MRI perfusion and MR Spectroscopy suggested a process of seeding metastases surrounding the ventricular drain. Postoperative histopathological examination results were consistent with tuberculoma.
Conclusion: Tuberculoma should always be considered as one of the differential diagnoses along with primary and secondary intracranial neoplasm, particularly in developing and TB endemic countries, and inpatient with immunocompromised state.
Keywords: Brain tumor, Craniopharyngioma, Tuberculoma, Tuberculosis, Ventriculoperitoneal shunt seeding
INTRODUCTION
Tuberculosis (TB) is still a big problem in developing and TB endemic countries such as Indonesia. TB is a disease caused by Mycobacterium tuberculosis[
The most common manifestations of TB in the central nervous system (CNS) are tuberculous meningitis at 1–2% and tuberculoma.[
Tuberculomas are common in patients with systemic TB, pediatric population, or immunocompromised conditions such as AIDS, diabetes mellitus, pregnancy, elderly transplantation, alcoholism, and chemotherapy.[
To the best of our knowledge, tuberculoma surrounding the ventricular drain in a patient with a history of surgical excision of brain tumor and insertion of ventriculoperitoneal (VP) shunt has not been previously reported.
In this case report, we present an isolated tuberculoma surrounding ventricular drain in a pediatric patient with a history of craniopharyngioma excision and VP shunt placement without sign of systemic TB or tuberculous meningitis.
CASE PRESENTATION
An 11-year-old, Indonesian girl has been complaining persistent headache in the past 3 years. The headache was getting worse.
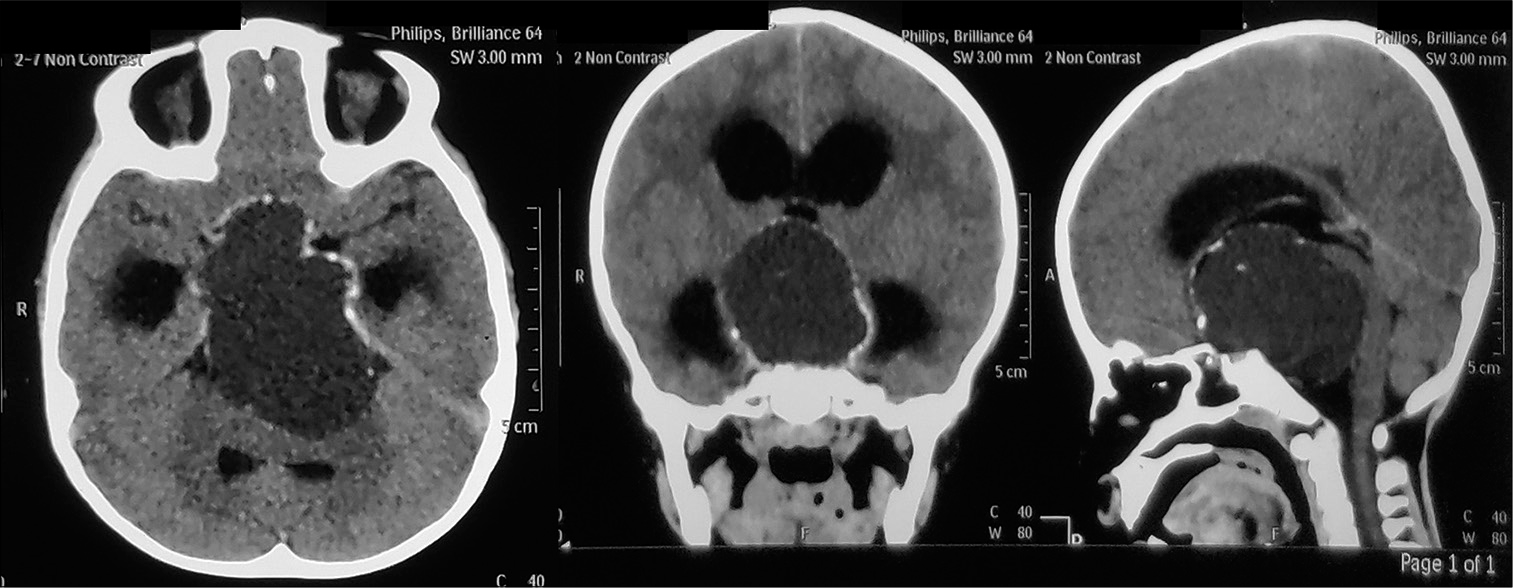
The patient had a history of surgical excision of craniopharyngioma [
From the anamnesis, the patient did not have TB symptoms such as prolonged cough, unexplained fever, weight loss, and night sweats. The patient had no history of contact with family, friends, or surrounding people with TB disease. The patient had no history of previous routine antibiotics treatment.
On examination, the patient had a stable vital sign with normothermia. She was fully conscious with GCS E4M6V5. There were no meningeal sign nor nuchal rigidity. Other neurological examinations were normal. The patient was immunocompetent and well-nourished. There was no sign of systemic TB nor meningoencephalitis. Routine laboratory tests and chest X-ray were all normal.
Imaging
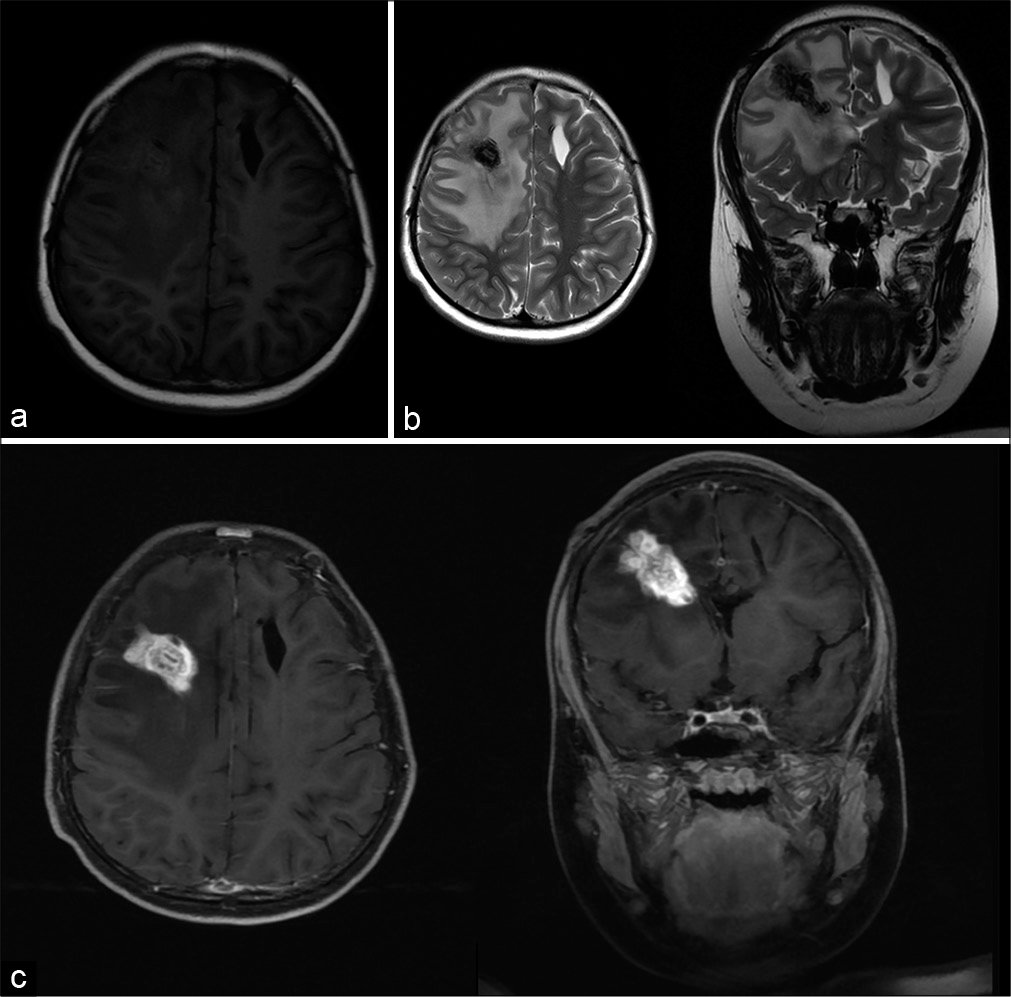
Brain magnetic resonance imaging (MRI) [
Figure 2:
Preoperative radiological examination Brain MRI (2021) revealed 4 × 2.3 × 2.1 cm mass surrounding the ventricular drain which was attached in the anterior horn of the right lateral ventricle to the right frontal cortex. T1 (a) showed the mass was isointense, T2 (b) showed the mass was hypointense. After administration of gadolinium (c), the mass was highly heterogeneous contrast enhancement. There was perifocal edema around the tumor.
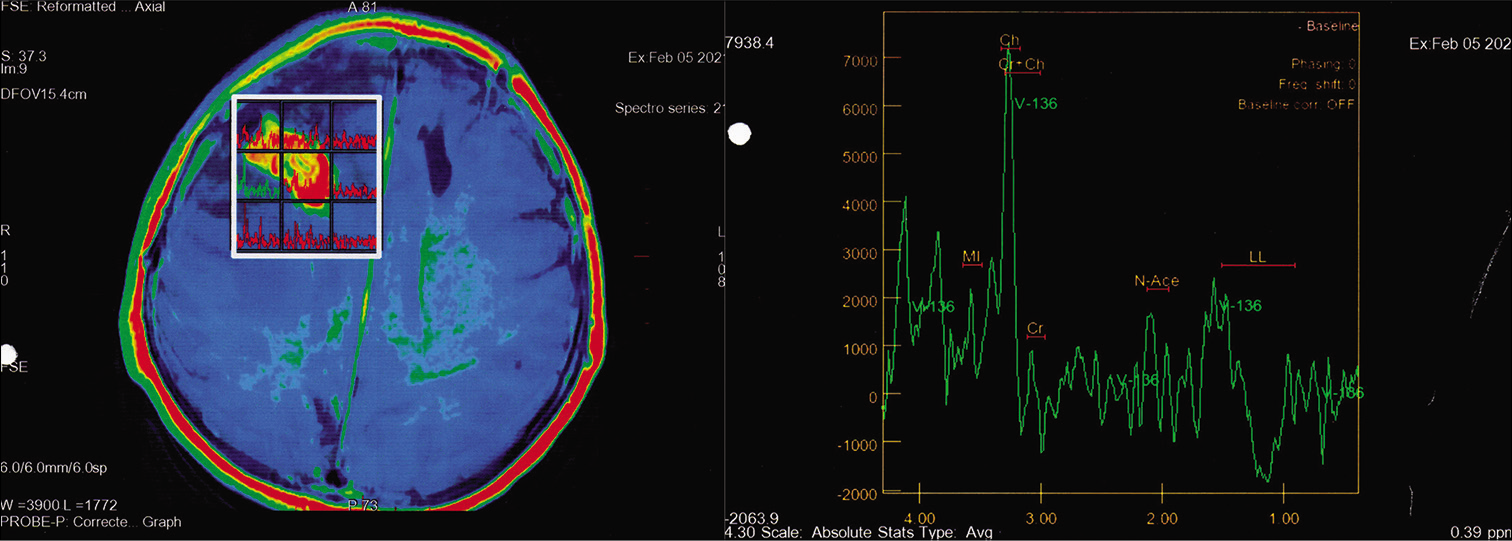
On dynamic susceptibility contrast (DSC) MRI perfusion, the relative cerebral blood volume appeared to be elevated, leading to a malignant process. On MR Spectroscopy (MRS) [
There was no sign of hydrocephalus nor residual of craniopharyngioma. No sign of meningoencephalitis was seen.
From brain MRI examination suggested a process of seeding metastases surrounding the ventricular drain in the area of the anterior horn of the right lateral ventricle to the right frontal cortex.
Surgical procedure
From the preoperative anamnesis, physical examination, and imaging, the mass suggested a metastatic process with no suspicion of tuberculoma. Therefore, we did not give trial antibiotics or TB treatment before surgery.
Surgery was done to reduce mass effect symptoms, as well as to obtain tissue to establish the diagnosis. The initial goal of surgery was gross total resection. A right frontotemporal craniotomy was performed. The existing chamber and peritoneal drain of VP shunt were disconnected and removed.
The lesion appeared to be surrounding the ventricular drain. The lesion was solid, firm, calcified, and adheres tightly to the ventricular drain. The lesion was very hard and cannot be easily separated by electrocautery and suction. Therefore, careful piecemeal debulking of the tumor was carried out using scissors, until the tumor was completely removed and healthy parenchymal tissue was seen.
Histopathology
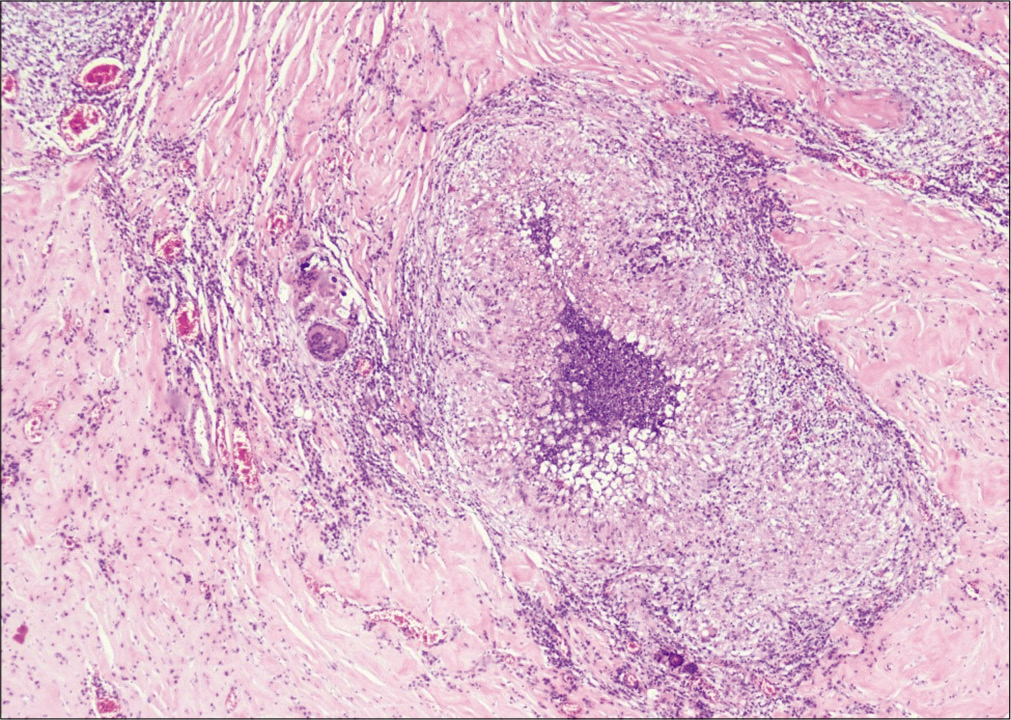
Histopathology examination [
Figure 4:
Histopathology examination revealed a large fibrotic area containing many granulomas (red arrow), consisting of epithelial cells surrounded by lymphocytes. Langhans giant cells (green arrow) were also seen at the periphery of the granuloma. There was no sign of malignancy. Histopathological findings were consistent with tuberculoma.
Unfortunately, the samples of operation were only examined for histopathology. There were no samples sent to the microbiology department for culture examination.
Post-operative course
There was no complication after surgery. The patient was discharged on postoperative day 3 in good condition. Five months after surgery, the patient is still routinely checked in to the outpatient clinic. There are no complaints or neurological deficits. Currently, the patient is receiving treatment for extrapulmonary TB.
DISCUSSION
CNS manifestation of TB is one of the most dangerous forms of TB. This disease is caused by hematogenic spread of M. tuberculosis. The most common CNS manifestations of TB are tuberculous meningitis and tuberculoma.[
Tuberculomas are common in patients with systemic TB, pediatric population, or immunocompromised conditions. In developing and TB endemic countries, tuberculomas account for 33% of the intracranial space-occupying lesions.[
On physical and radiological examination, tuberculoma often gives an atypical appearance. Tuberculoma can give symptoms of increased intracranial pressure due to mass effect. From imaging, tuberculoma often mimics another intracranial tumor.[
From brain MRI, tuberculoma could appear hypo or isointense in T1 and hypointense in T2. After administration of contrast, the mass will homogenously contrast enhancement, and often there was massive perifocal edema. MR spectroscopy could be useful to differentiate tuberculoma with other abscess or neoplasm. On MRS, the NAA/Creatine and NAA/Choline ratio appears to be decreased in tuberculoma cases.[
Because brain MRI are often inconclusive, sometimes the accurate diagnosis can only be made after postoperative histopathological and microbiology examination. Surgical biopsy or pathological tissue examination is the most accurate diagnostic method and should be considered in cases of tuberculoma without tuberculous meningitis or systemic TB, especially in developing and TB endemic countries.[
In our case, the patient came with symptoms of elevated intracranial pressure with a history of craniopharyngioma excision and VP shunt placement. The patient had no sign of systemic TB or tuberculous meningitis. From brain MRI it appears there was a mass surrounding the ventricular drain and there was no sign of meningitis. From DSC MR perfusion and MR spectroscopy suggesting a metastatic process. Surgery has been done to reduce the effect of increased intracranial pressure. Histopathological examination results were consistent with tuberculoma.
From our case, before the surgery, we did not think the mass will be tuberculoma, because from the preoperative examination, the mass suggested to a metastatic process. Therefore, we did not give trial of antibiotics or TB treatments prior the surgery.
Since there was no suspicion of infection or tuberculoma, we only sent operative samples to pathology and did not send samples for microbiological examination. Hence, we could not obtain M. tuberculosis culture from the samples. At our policy, treatment for extrapulmonary TB can still be given based on the pathological results of tuberculoma, without waiting for the culture results.
CONCLUSION
Tuberculoma is one of the most common intracranial lesions, especially in developing and TB endemic countries. From physical and radiological examination, tuberculoma could seem atypical and mimic other intracranial lesions.
In our opinion, neurosurgeons in TB endemic countries should always think of tuberculoma as one of the differential diagnoses along with primary and secondary intracranial neoplasm, particularly in developing and TB endemic countries, and inpatient with immunocompromised state. Trial of TB drugs before surgery may be considered, especially in dubious cases, and inpatient with stable and non-life-threatening state. Learning from our experience, it is recommended that samples of operation always be sent to pathology and microbiology departments for a thorough postoperative examination.
To the best of our knowledge, this is the first reported case of tuberculoma surrounding the ventricular drain in patient with a history of craniopharyngioma excision and VP shunt placement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
1. Anuradha HK, Garg RK, Sinha MK, Agarwal A, Verma R, Singh MK. Intracranial tuberculomas in patients with tuberculous meningitis: Predictors and prognostic significance. Int J Tuberc Lung Dis. 2011. 15: 234-9
2. Binesh F, Zahir ST, Bovanlu TR. Isolated cerebellar tuberculoma mimicking posterior cranial fossa tumour. BMJ Case Rep. 2013. 2013: bcr2013009965
3. Hejazi N, Hassler W. Multiple intracranial tuberculomas with atypical response to tuberculostatic chemotherapy: Case report and review of the literature. Acta Neurochir (Wien). 1997. 139: 194-202
4. Jinkins JR. Computed tomography of intracranial tuberculosis. Neuroradiology. 1991. 33: 126-35
5. Khatri GD, Krishnan V, Antil N, Saigal G. Magnetic resonance imaging spectrum of intracranial tubercular lesions: One disease, many faces. Pol J Radiol. 2018. 83: e524-35
6. Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 2015. 78: 47-55
7. Mezochow A, Thakur K, Vinnard C. Tuberculous meningitis in children and adults: New insights for an ancient foe. Curr Neurol Neurosci Rep. 2017. 17: 85
8. Monteiro R, Carneiro JC, Costa C, Duarte R. Cerebral tuberculomas-a clinical challenge. Respir Med Case Rep. 2013. 9: 34-7
9. Osborn AG.editors. Tuberculosis and fungal, parasitic, and other infections In: 14 Osborn’s Brain Imaging, Pathology, and Anatomy. Philadelphia, PA: Elsevier. Inc; 2018. 1: 377-89
10. Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ. Extrapulmonary tuberculosis: Pathophysiology and imaging findings. Radiographics. 2019. 39: 2023-37
11. Sharma G, Kaushal P, Vaidya B, Kumar P. Third ventricular tuberculoma mimicking as a tumor: Report of a very rare case. Asian J Neurosurg. 2017. 12: 58-61
12. Ssenyonga P.editors. Neurosurgical management of tuberculous meningitis Tuberculous Meningitis Manual of Diagnosis and Therapy. London: Elsevier. Inc; 2020. 1: 106-7
13. Turan Suslu H, Bozbuga M, Bayindir C. Cerebral tuberculoma mimicking high grade glial tumor. Turk Neurosurg. 2011. 21: 427-9
14. 15. Zahrou F, Elallouchi Y, Ghannane H, Benali SA, Aniba K. Diagnosis and management of intracranial tuberculomas: About 2 cases and a review of the literature. Pan Afr Med J. 2019. 34: 1-6