- Department of Orthopaedics, Cedars-Sinai Medical Center, Los Angeles, California, United States.
- Department of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, California, United States.
Correspondence Address:
Robert C. Ryu
Department of Orthopaedics, Cedars-Sinai Medical Center, Los Angeles, California, United States.
DOI:10.25259/SNI_587_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Robert C. Ryu1, Phillip H. Behrens1, Blake A. Burkert1, J. Patrick Johnson2, Terrence T. Kim1. Two-level cervical disc arthroplasty in patients with Klippel-Feil syndrome: A case report and review of the literature. 02-Oct-2020;11:322
How to cite this URL: Robert C. Ryu1, Phillip H. Behrens1, Blake A. Burkert1, J. Patrick Johnson2, Terrence T. Kim1. Two-level cervical disc arthroplasty in patients with Klippel-Feil syndrome: A case report and review of the literature. 02-Oct-2020;11:322. Available from: https://surgicalneurologyint.com/surgicalint-articles/10300/
Abstract
Background: Klippel-Feil syndrome (KFS) is defined by multiple abnormal segments of the cervical spine with congenital synostosis of two or more cervical vertebrae. KFS patients who demonstrate progressive symptomatic instability and/or neurologic sequelae are traditionally managed with operative decompression and arthrodesis.
Case Description: A 44-year-old female with chronic neck pain and radiculopathy and a C7-T1 KFS presented with adjacent segment degenerative disc disease at the C5-6 and C6-7 levels. She was successfully managed with a two-level cervical disc arthroplasty (CDA).
Conclusion: Patients with KFS and disease at two contiguous, adjacent levels (e.g., cervical disc disease) may be safely and effectively managed with two-level CDA.
Keywords: Adjacent segment disease, Artificial disc replacement, Cervical disc arthroplasty, Congenital cervical fusion, Klippel-Feil syndrome, Motion preservation surgery
INTRODUCTION
The United States Food and Drug Administration investigational device exemption trial documented that 10 years following two adjacent level cervical disc arthroplasty (CDA), patients continued to show clinical improvement and preservation of motion at the operated levels.[
In this case study, a 44-year-old female with a history of a C7-T1 Klippel-Feil syndrome (KFS) and two-level adjacent disc disease, successfully and safely underwent a contiguous two-level CDA (i.e., at the C5-C6 and C6-C7 levels).
CASE REPORT
History and examination
A 44-year-old female with a history of C7-T1 KFS presented with the chief complaint of neck and right-arm pain with radiculopathy. On examination, she had limited cervical flexion and extension, right paraspinal cervical tenderness, and weakness in the right C6 and C7 root distributions (both 4/5).
Imaging
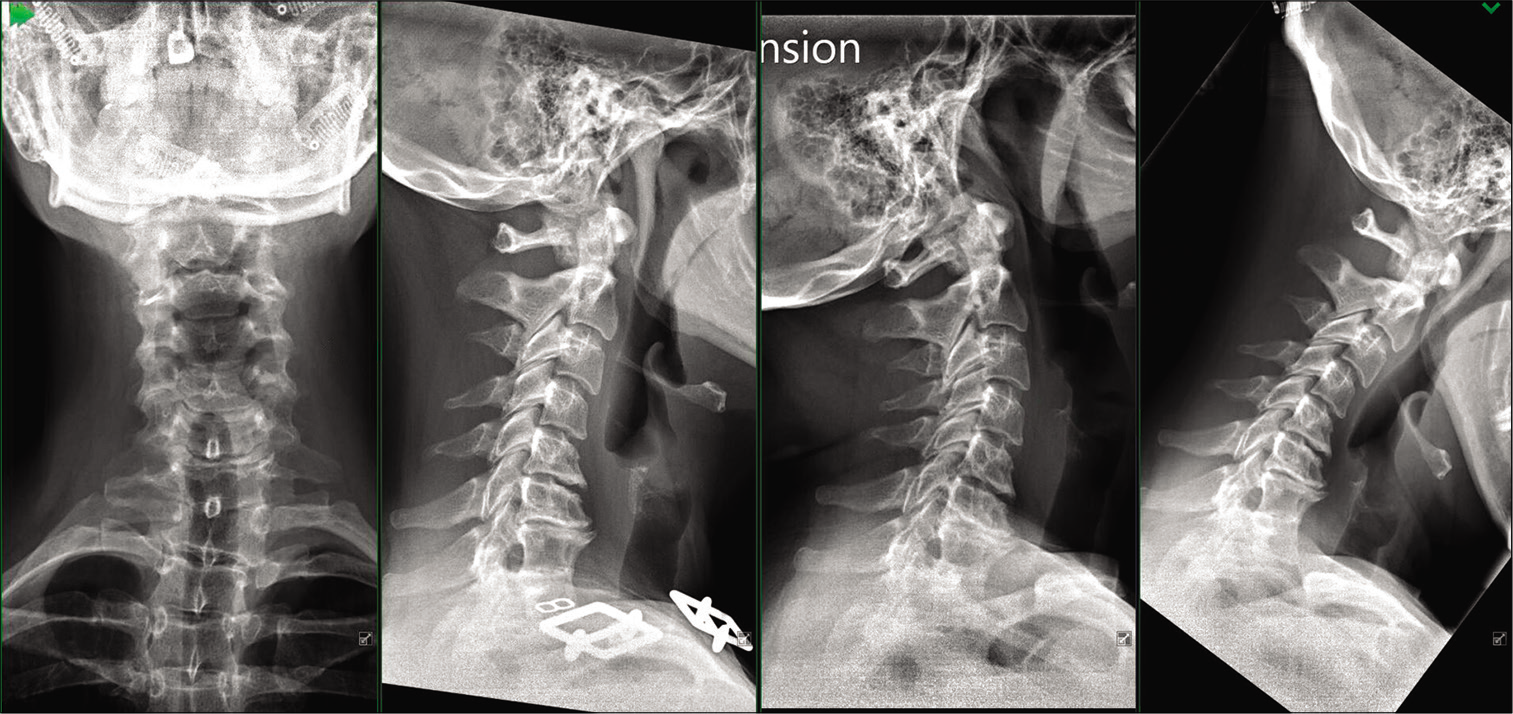
Cervical dynamic X-rays showed a loss of the normal cervical lordosis with a congenital KFS fusion at the C7-T1 level; dynamic studies confirmed no instability at that level [
CASE DESCRIPTION
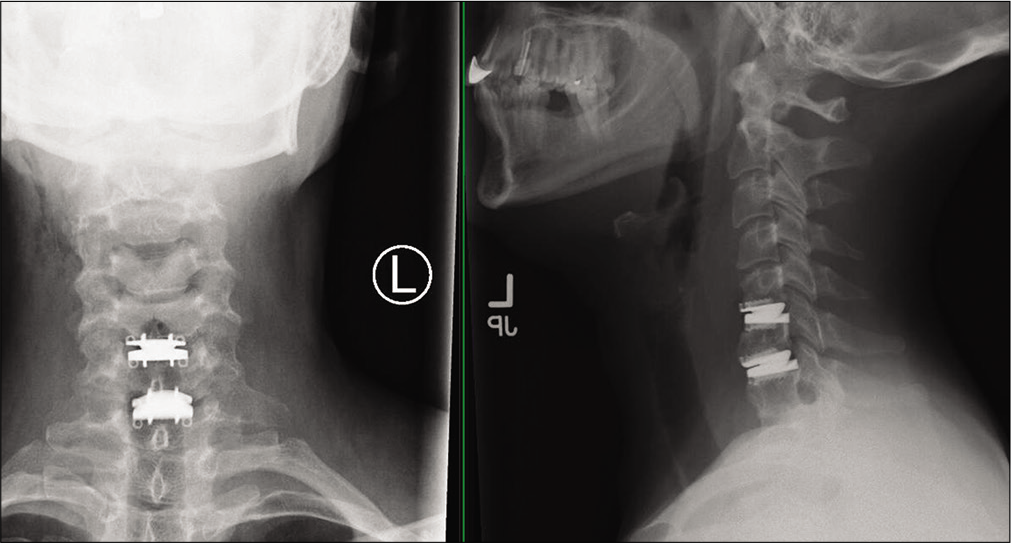
The patient underwent a two-level C5-C6 and C6-C7 CDA. A routine exposure was performed. Complete C5-C6 and C6-C7 discectomies, including resection of the posterior longitudinal ligament, were performed. In addition, the endplates at both levels were contoured and keels were cut to allow for implantation of the CDA devices [
Postoperatively, the patient regained full 5/5 strength of her right C6 and C7 root distributions. Formal upright vertical radiographs the next day, before discharge, confirmed adequate CDA positioning [
DISCUSSION
Klippel-Feil patients with progressive symptomatic instability and/or neurologic sequelae are traditionally managed with ACDF. However, adjacent segment disease with the added loss of cervical range of motion is of particular concern in this patient population.
Symptomatic adjacent segment disease
Hilibrand and Robbins established that symptomatic adjacent segment disease occurs in 2.9% of patients/year and that 25% develop adjacent segment disease requiring additional surgery within 10 years following an ACDF.[
Theory behind CDA
The theory behind utilizing CDA, specifically adjacent to a KFS, is to decrease the incidence of future adjacent cervical disc disease. Gornet and Lanman’s multicenter data demonstrated the superiority of two-level CDA over ACDF at 10 postoperative years; the overall success was 80.4% for CDA versus 62.2% for ACDF.[
A recent meta-analysis of 19 trials found that CDA was superior to ACDF in terms of overall neck disability index (NDI), neurological recovery of function, higher 36-Item Short Form Health Survey (SF-36) results, higher patient satisfaction, greater range of motion, and fewer secondary operations (P < 0.05).[
CONCLUSION
Here, we have demonstrated that a patient with a C7-T1 KFS and two-level adjacent segment disease (e.g., C5-C6 and C6-C7) could be safely and successfully managed with a contiguous, two-level C5-C6/C6-C7 CDA.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, Hodges SD. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-Year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine. 2019. 1: 1-11
2. Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: The consequences of spinal fusion?. Spine J. 2004. 4: 190S-4S
3. Kan SL, Yuan ZF, Ning GZ, Liu FF, Sun JC, Feng SQ. Cervical disc arthroplasty for symptomatic cervical disc disease: Traditional and Bayesian meta-analysis with trial sequential analysis. Int J Surg. 2016. 35: 111-9
4. McAfee PC. The indications for lumbar and cervical disc replacement. Spine J. 2004. 4: 177S-81S
5. Wu TK, Meng Y, Liu H, Hong Y, Wang BY, Rong X. Primary cervical disc arthroplasty versus cervical disc arthroplasty adjacent to previous fusion. A retrospective study with 48 months of follow-up. Medicine (Baltimore). 2018. 97: e11755
6. Zou S, Gao J, Xu B, Lu X, Han Y, Meng H. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: A meta-analysis of randomized controlled trials. Eur Spine J. 2017. 26: 985-97