- Department of Neurosurgery, Medical Research Institute Kitano Hospital, PIIF Tazuke-Kofukai, Osaka, Japan
- Department of Neurosurgery, Hikone Chuo Hospital, Hikone, Japan
Correspondence Address:
Hirokuni Hashikata, Department of Neurosurgery, Medical Research Institute Kitano Hospital, PIIF TazukeKofukai, Osaka, Japan.
DOI:10.25259/SNI_1015_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hirokuni Hashikata1, Yasunori Nagai1, Gen Futamura1, Naokado Ikeda1, Masanori Goto1, Yoshinori Maki2, Hiroki Toda1, Koichi Iwasaki1. Two reports of iatrogenic pseudoaneurysms intraoperatively induced by an ultrasonic surgical aspirator: A rare intraoperative complication. 19-Jul-2024;15:251
How to cite this URL: Hirokuni Hashikata1, Yasunori Nagai1, Gen Futamura1, Naokado Ikeda1, Masanori Goto1, Yoshinori Maki2, Hiroki Toda1, Koichi Iwasaki1. Two reports of iatrogenic pseudoaneurysms intraoperatively induced by an ultrasonic surgical aspirator: A rare intraoperative complication. 19-Jul-2024;15:251. Available from: https://surgicalneurologyint.com/surgicalint-articles/12995/
Abstract
Background: The ultrasonic surgical aspirator is widely used in intracranial tumor resection as this instrument is considered safe. The advantage of an ultrasonic surgical aspirator is that it does not damage vessels or nerves close to the tumor. Therefore, limited information exists regarding intraoperative arterial injury by the ultrasonic surgical aspirator.
Case Description: We report two cases. The first case was a 30-year-old woman who underwent surgery for a recurrent craniopharyngioma, and the second was a 50-year-old man who underwent surgery for a meningioma. A craniopharyngioma encased the basilar artery in the former case, and the superior cerebellar artery was encased by a meningioma in the latter. An ultrasonic surgical aspirator was used to resect the tumors in two cases. During surgery, the arteries involved in the tumors were unintentionally injured using an ultrasonic surgical aspirator. Intraoperative hemostasis was achieved for the bleeding from the injured arteries. However, postoperative digital cerebral angiography revealed pseudoaneurysms in the injured arteries. A subarachnoid hemorrhage occurred in the first case. The pseudoaneurysms were managed using endovascular embolization.
Conclusion: Intraoperative arterial injury can occur with the application of an ultrasonic surgical aspirator. Neurosurgeons should be cautious when using ultrasonic surgical aspirators to avoid damaging the arteries involved with the tumor.
Keywords: Brain tumor, Complication, Endovascular embolization, Pseudoaneurysm, Ultrasonic aspirator
INTRODUCTION
Central nervous system tumors, including malignant tumors, account for approximately 1% of all invasive neoplasms.[
The ultrasonic surgical aspirator is a surgical instrument that was first applied in the neurosurgical field in 1978.[
Here, we report two cases of arterial injury induced by an ultrasonic surgical aspirator, indicating the possibility of rare intraoperative complications.
CASE PRESENTATION
Case 1
A 30-year-old woman was admitted to our hospital. The patient had a past episode of recurrent and refractory craniopharyngioma for which she underwent tumor removal surgery, radiotherapy, and chemotherapy. As the growth of the residual craniopharyngioma resulted in incontinence and aggravated the recent memory disturbances, direct salvage surgery was planned. Neurological examination on admission revealed incontinence, aggravated memory disturbances, and total blindness. Preoperative magnetic resonance imaging revealed that the tumor extended near the brainstem and involved the basilar artery [
Figure 1:
Radiological characteristics before endovascular embolization of the pseudoaneurysm (case 1). (a-b) Gadolinium-enhanced T1-weighted magnetic resonance images showing the basilar artery (white arrowhead) involved in the tumor (a: sagittal image and b: axial image).(c) Magnetic resonance angiography reveals no apparent vascular lesions .(d-f) A pseudoaneurysm (white arrow) in the basilar artery increased chronologically on computed tomography angiography (d: the following day, e: 5 days, and f: 13 days after tumor removal).(g) Subarachnoid and intraventricular hemorrhages occur due to the ruptured pseudoaneurysms.
Figure 2:
Radiological characteristics during and after endovascular embolization of the pseudoaneurysm (case 1). (a-d) The pseudoaneurysm (white arrow) in the basilar artery is embolized using microcoils via the stent-assisted technique. After embolization, no flow into the pseudoaneurysm was observed (white arrowhead) (a and b: intraoperative angiography before embolization; c and d: after embolization). (e) Postoperative magnetic resonance imaging showing no ischemic complications.
Case 2
A 50-year-old man was referred for the surgical removal of an incidentally diagnosed tumor. Although the tumor was asymptomatic, it compressed the brainstem [
Figure 3:
Radiological characteristics before endovascular embolization of the pseudoaneurysm (case 2). (a-c) Gadolinium-enhanced T1-weighted magnetic resonance images showing involvement of the superior cerebellar artery (white arrowhead) by the tumor. The left posterior cerebral artery is compressed by the tumor (white arrow) (a: axial image, b: coronal image, and c: sagittal image). (d-e) Left vertebral angiography showing that the pathway of the left posterior cerebral artery (white arrow) is shifted by the tumor. The vascular-rich tumor is fed by the superior cerebellar artery (white arrowhead) (d: arterial phase; e: capillary phase). AP: anterior-posterior projection; Lat: lateral projection.
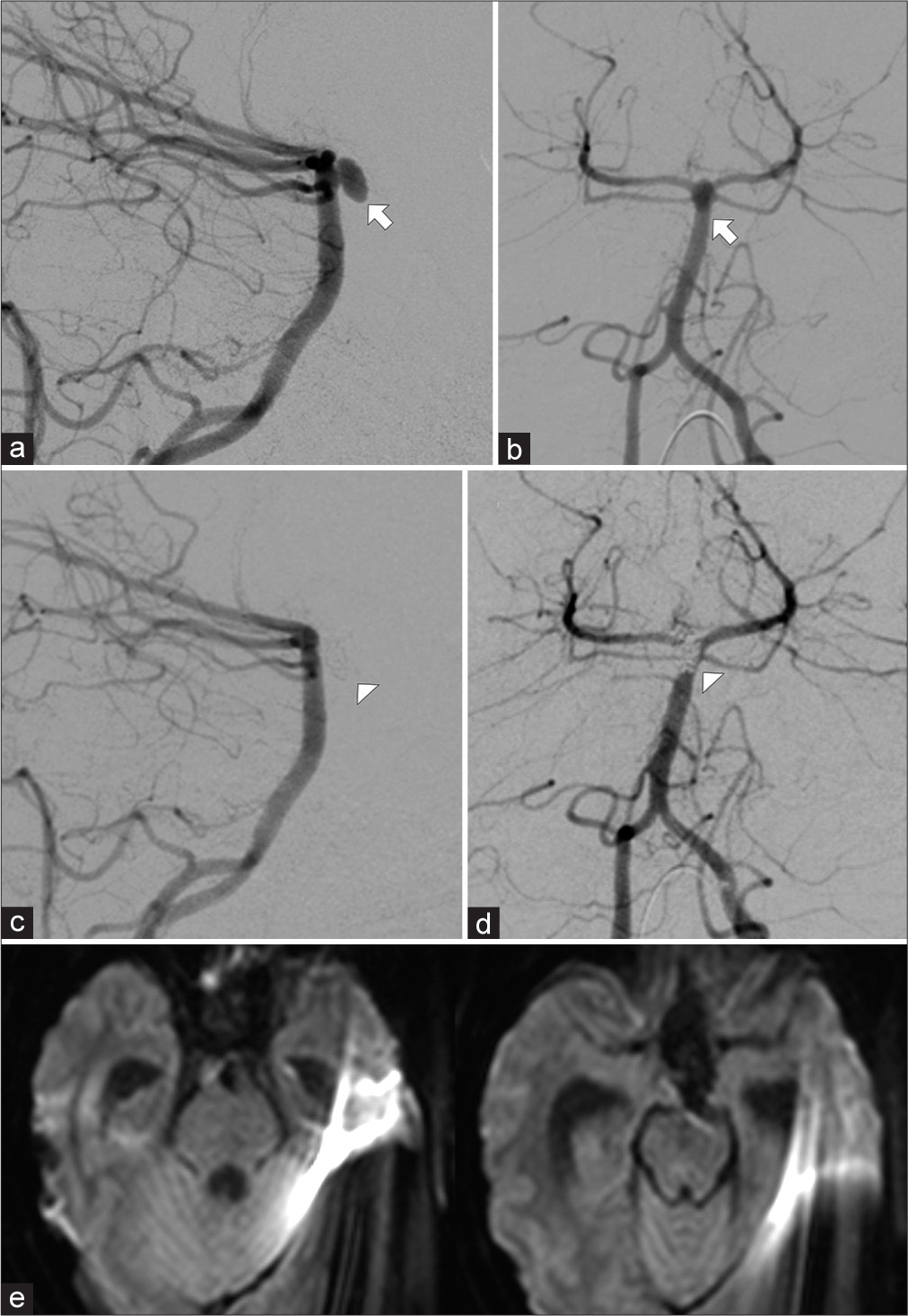
Figure 4:
Radiological characteristics during and after endovascular embolization of the pseudoaneurysm (case 2). (a) Left vertebral angiography shows a pseudoaneurysm (white arrowhead) in the left superior cerebellar artery (black arrowhead).The posterior cerebral artery (black arrow) is intact.(b) Three-dimensional reconstructed maximum intensity projection images also revealed a pseudoaneurysm (white arrowhead).(c) Parent artery occlusion, including the pseudoaneurysm (dagger), was performed using microcoils (white arrow).The posterior cerebral artery (black arrow) remained intact.(d) Postoperative magnetic resonance image showing cerebellar infarction due to the sacrificed superior cerebellar artery.
DISCUSSION
Here, we described two cases in which tumor resection was performed using an ultrasonic surgical aspirator. In both cases, the tumors encased the intracranial arteries, and were unexpectedly injured using an ultrasonic surgical aspirator. These accidents require intraoperative hemostasis, resulting in pseudoaneurysm formation. Endovascular embolization resolved these pseudoaneurysms, although a subarachnoid hemorrhage occurred in one case. No similar intraoperative complications related to ultrasonic surgical aspirators have been previously reported.
The rare incidence of arterial injury induced by the application of ultrasonic surgical aspirators is attributed to their excellent tissue selectivity. Kudo et al. reported an intraoperative arterial injury using an ultrasonic surgical aspirator.[
In managing intraoperative arterial injuries caused by the ultrasonic surgical aspirator, achieving complete hemostasis is an indispensable step. However, as observed in our cases, pseudoaneurysms can consequently form. Therefore, postoperative digital subtraction angiography should be performed. Because pseudoaneurysms are known for their high rate of rupture, direct surgery or endovascular embolization is also warranted to prevent rupture or re-rupture.
A subarachnoid hemorrhage occurred due to a gradually enlarging pseudoaneurysm, which was observed in the first case. In the first case, a pseudoaneurysm formed in the basilar artery. Therefore, the parent artery occlusion was not observed in this case. Stent-assisted coil embolization of the pseudoaneurysm was planned, and dual antiplatelet therapy was initiated. However, the pseudoaneurysm ruptured before endovascular embolization was performed. However, in the second case, because the pseudoaneurysm was located in the superior cerebellar artery, parent artery occlusion could be performed. Therefore, the pseudoaneurysm was embolized with parent artery occlusion soon after the tumor resection. Even if endovascular embolization cannot be performed soon after tumor surgery due to the pseudoaneurysmal location, patients should be frequently monitored using computed tomography or magnetic resonance angiography.
CONCLUSION
As observed in our cases, the intraoperative application of an ultrasonic surgical aspirator can result in iatrogenic pseudoaneurysms. In cases where intracranial arteries are involved in a tumor, neurosurgeons should be aware of this rare complication. Intraoperatively, caution should be exercised to avoid damaging the arteries involved in the tumor. Once intraoperative hemostasis is achieved, the injured arteries should be closely followed up by angiographic examinations.
Ethical approval
The research/study approved by the Institutional Review Board at Medical Research Institute KITANO HOSPITAL, PIIF Tazuke-kofukai, number P221000400, dated October 17, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Flamm ES, Ransohoff J, Wuchinich D, Broadwin A. Preliminary experience with ultrasonic aspiration in neurosurgery. Neurosurgery. 1978. 2: 240-5
2. Kudo T, Ueki S, Kobayashi H, Torigoe H, Tadokoro M. Experience with the ultrasonic surgical aspirator in a cavernous hemangioma of the cavernous sinus. Neurosurgery. 1989. 24: 628-31
3. Lochan R, Ansari I, Coates R, Robinson SM, White SA. Methods of haemostasis during liver resection--a UK national survey. Dig Surg. 2013. 30: 375-82
4. Miller KD, Ostrom QT, Kruchko C, Patil N, Tihan T, Cioffi G. Brain and other central nervous system tumor statistics, 2021. CA Cancer J Clin. 2021. 71: 381-406
5. Miyake K, Nakamura T, Fujimura H, Shibuya T, Sawa Y. Efficacy of the decalcification of heavily calcified femoral bifurcation lesions using a cavitron ultrasonic surgical aspirator. Ann Vasc Surg. 2020. 69: 274-84
6. Nakasu S, Hirano A, Llena JF, Shimura T, Handa J. Interface between the meningioma and the brain. Surg Neurol. 1989. 32: 206-12
7. Vällfors B, Hansson HA, Larsson S, Johansson G. Suction in neurosurgery. Acta Neurochir (Wien). 1980. 55: 35-42
8. Weibl P, Shariat SF, Klatte T. Partial nephrectomy driven by cavitron ultrasonic surgical aspirator under zero ischemia: A pilot study. World J Urol. 2015. 33: 2015-21