- Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, New York, USA
Correspondence Address:
Jonathan Nakhla
Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, New York, USA
DOI:10.4103/2152-7806.196766
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Merritt D. Kinon, Jonathan Nakhla, Kenroy Brown, Niketh Bhashyam, Reza Yassari. Ultra-delayed lumbar surgical wound hematoma. 26-Dec-2016;7:
How to cite this URL: Merritt D. Kinon, Jonathan Nakhla, Kenroy Brown, Niketh Bhashyam, Reza Yassari. Ultra-delayed lumbar surgical wound hematoma. 26-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/ultra%e2%80%91delayed-lumbar-surgical-wound-hematoma/
Abstract
Background:There exists an inherent risk of increased venous thromboembolism (VTE) in surgical spine patients, which is independent of their existing risk factors. Prophylaxis and treatment of VTE is an imprecise practice and may have serious complications even well after the initial surgery. Furthermore, there are no clear guidelines on how to manage postoperative spine patients with regards to the timing of anticoagulation.
Case Description:Here, we present the case of a middle-aged male, status post L2/3 laminectomy and discectomy who developed bilateral below the knee deep venous thrombosis. He was started on Enoxaparin and transitioned to Warfarin and returned with axial back pain, and was found to have a postoperative hematoma almost 3 weeks later in a delayed fashion.
Conclusion:Delayed surgical wound hematoma with neural compression is an important complication to identify and should remain high on the differential diagnosis in patients on warfarin who present with axial spinal pain.
Keywords: Anticoagulation, complication, spinal decompression, venous thromboembolism, wound hematoma
INTRODUCTION
The risk of venous thromboembolism (VTE) in a post-surgical spine patient can be increased due to existing comorbidities in addition to the inherent increased risk of the spine surgery itself. The current literature suggests that, although there are no specific recommendations for VTE, prophylaxis, elastic compression stockings, low molecular weight heparin (LMWH), low dose unfractionated heparin (LDUH), early ambulation, or intermittent pneumatic compression may help in VTE prevention in these patients.[
Wound hematoma is an important differential diagnosis for patients on warfarin who have a “relatively” recent history of spinal surgery and present with axial spinal pain and swelling around their surgical wound. In general, such a complication occurs within a few days to a week after starting postoperative anticoagulation therapy.[
CASE PRESENTATION
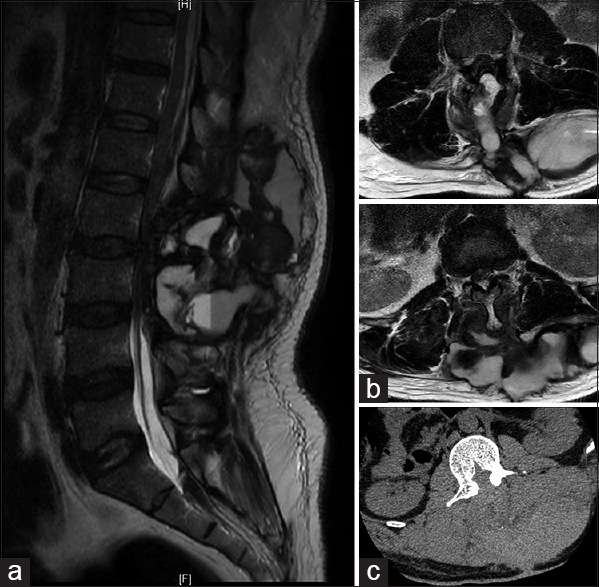
Our patient, a middle-aged male, status post L2-L3 laminectomy and discectomy for acute lower extremity weakness, developed bilateral below the knee deep venous thrombosis (DVT) on postoperative day 10 (POD) and was started on therapeutic Enoxaparin immediately. On POD 18, he was transitioned to Warfarin. Two days after starting Warfarin (POD 20), he developed terrible low back pain as well as worsening lower extremity weakness. At the time of arrival to our Emergency Department, his international normalized ratio (INR) was 2.8. His surgical wound was well healed, however, it was extremely tense and tender to touch. There was significant swelling that tracked from his lumbar wound out laterally to his flanks. Magnetic resonance (MR) imaging of the lumbar spine was done and showed a large, heterogeneous, multiloculated collection concerning for hematoma extending from the laminectomy defect to the overlying subcutaneous fat and dissecting out laterally to his flanks with significant epidural compression [
DISCUSSION
Little evidence exists supporting post-surgical delayed wound hematoma in a patient over a week after starting anticoagulation therapy.[
Large wound hematomas in a spine surgery patient can cause neural compression and also have symptoms consistent with acute spinal epidural hematomas. The symptoms of acute spinal epidural hematoma, as described in the medical literature, are sudden onset of severe pain along the spinal column lasting from a few minutes to a few hours, possibly with focal or evolving neurological symptoms such as flaccid paralysis or loss of sphincter control.[
Certain conditions appear to predispose individuals to VTE. The American College of Chest Physicians Consensus Conference on Antithrombotic and Thrombolytic Therapy has a scoring to predict VTE, which includes the following as major risk factors: Age, bed confinement, history of malignancy, history of DVT, obesity, and spinal cord injury with paralysis.[
As the complexity of spinal surgery has increased, so has the incidence of DVT and pulmonary embolism (PE). In spite of the use of different prophylactic methods, VTE is still a significant complication following spinal surgery. In surgery of the lumbosacral spinal, the lowest quoted rates are 0.6% for DVT and 0.3% for PE.[
CONCLUSION
The incidence of VTE has risen along with the rise of complexity in spinal surgery. Neurological procedures themselves have an inherent risk of VTE and there is no consensus as to when to begin anticoagulant therapy. With many unknowns and individual patient treatment needs, one should maintain high suspicion for wound hematoma even in patients 3 weeks out from surgery on anticoagulants.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Stein P, Goldhaber S, Gottschalk A, Hull R, Hyers T, Leeper K. Opinions regarding the diagnosis and management of venous thromboembolic disease. ACCP Consensus Committee on Pulmonary Embolism. American College of Chest Physicians. Chest. 1998. 113: 499-504
2. Brambilla S, Ruosi C, La Maida GA, Caserta S. Prevention of venous thromboembolism in spinal surgery. Eur Spine J. 2004. 13: 1-8
3. Browd SR, Ragel BT, Davis GE, Scott AM, Skalabrin EJ, Couldwell WT. Prophylaxis for deep venous thrombosis in neurosurgery: A review of the literature. Neurosurg Focus. 2004. 17: E1-
4. Carroll SG, Malhotra R, Eustace D, Sharr M, Morcos S. Spontaneous spinal extradural hematoma during pregnancy. J Matern Fetal Med. 1997. 6: 218-9
5. Crisi G, Sorgato P, Colombo A, Scarpa M, Falasca A, Angiari P. Gadolinium-DTPA-enhanced MR imaging in the diagnosis of spinal epidural haematoma. Report of a case. Neuroradiology. 1990. 32: 64-6
6. Daniels PR. Peri-procedural management of patients taking oral anticoagulants. BMJ. 2015. 351: h2391-
7. Dziedzic T, Kunert P, Krych P, Marchel A. Management and neurological outcome of spontaneous spinal epidural hematoma. J Clin Neurosci. 2015. 22: 726-9
8. Galzio RJ, Zenobii M, D’Ecclesia G. Spontaneous spinal epidural hematoma: Report of a case with complete recovery. Surg Neurol. 1980. 14: 263-5
9. Hawryluk GW, Furlan JC, Austin JW, Fehlings MG. Individual characteristics and management decisions affect outcome of anticoagulated patients with intracranial hemorrhage. World Neurosurg. 2014. 81: 742-51
10. Janku GV, Paiement GD, Green HD. Prevention of venous thromboembolism in orthopaedics in the United States. Clin Orthop Relat Res. 1996. p. 313-21
11. Kunkala MR, Kehl J, Zielinski MD. Spontaneous rectus sheath hematomas: When to restart anticoagulation?. World J Surg. 2013. 37: 2555-9
12. Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: Relationship between surgical timing and neurological outcome. J Neurosurg. 1995. 83: 1-7
13. Liao CC, Hsieh PC, Lin TK, Lin CL, Lo YL, Lee SC. Surgical treatment of spontaneous spinal epidural hematoma: A 5-year experience. J Neurosurg Spine. 2009. 11: 480-6
14. Minato T, Miyagi M, Saito W, Shoji S, Nakazawa T, Inoue G. Spinal Epidural Hematoma after Thoracolumbar Posterior Fusion Surgery without Decompression for Thoracic Vertebral Fracture. Case Rep Orthop. 2016. 2016: 6295817-
15. Nicol M, Sun Y, Craig N, Wardlaw D. Incidence of thromboembolic complications in lumbar spinal surgery in 1,111 patients. Eur Spine J. 2009. 18: 1548-52
16. Oda T, Fuji T, Kato Y, Fujita S, Kanemitsu N. Deep venous thrombosis after posterior spinal surgery. Spine. 2000. 25: 2962-7
17. Rangwala SD, Birk DM, Tobin MK, Hahn YS, Nikas DC. Spontaneous Resolution of Spinal Epidural Hematoma Resulting from Domestic Child Abuse: Case Report. Pediatr Neurosurg. 2016. p.