- Department of Neurosurgery, National Oncologic Institute “Dr. Juan Tanca Marengo,” Guayaquil, Ecuador.
- Department of Pathology, National Oncologic Institute “Dr. Juan Tanca Marengo,” Guayaquil, Ecuador.
Correspondence Address:
Xavier Wong-Achi, Department of Neurosurgery, National Oncologic Institute “Dr. Juan Tanca Marengo,” Guayaquil, Ecuador.
DOI:10.25259/SNI_55_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: César Chong1, Xavier Wong-Achi1, Marlon Pozo2, Janio Pico1. Uncommon metastases to the brain: Frontal lobe myoepithelial carcinoma. 24-Feb-2023;14:74
How to cite this URL: César Chong1, Xavier Wong-Achi1, Marlon Pozo2, Janio Pico1. Uncommon metastases to the brain: Frontal lobe myoepithelial carcinoma. 24-Feb-2023;14:74. Available from: https://surgicalneurologyint.com/surgicalint-articles/12164/
Abstract
Background: Myoepithelial tumors have been widely described as a rare form of salivary gland neoplasm, although currently soft-tissue phenotypes have also been identified. These are tumors composed entirely of myoepithelial cells that exhibit a dual epithelial and smooth muscle phenotype. The occurrence of myoepithelial tumors within the central nervous system is also extremely rare, with only a few cases reported. Treatment options include surgical resection, chemotherapy, radiotherapy, or a combination of these approaches.
Case Description: The authors present a case of soft-tissue myoepithelial carcinoma with an unusual brain metastasis, rarely described in the literature. The purpose of this article is to present an update on the diagnosis and treatment of this pathology when affecting the central nervous system, through the review of the current evidence.
Conclusion: However, despite complete surgical resection, there is about a significative high rate of local recurrence and metastasis. Careful patient follow-up and staging is essential for better characterization and understanding of this tumor’s behavior.
Keywords: Brain neoplasms, Intracranial, Myoepithelioma, Neuro-oncology, Pathology
INTRODUCTION
Myoepithelial tumors are rare neoplasms arising from myoepithelial cells. Most tumors arise from the salivary glands, but usual sites of presentation include the oral cavity and pharynx. However, there have been reported cases seen in soft tissue, upper respiratory tract, breast, skin, and gastrointestinal tract.[
CASE PRESENTATION
A 43-year-old male, with a smoking history (3 pack-years), attended the soft-tissue surgery department presenting a lesion in the plantar area of the first metatarsal of the left foot (12 × 12 cm). On the surface, the lesion appeared ulcerated and deeply infiltrated soft tissues and contacted with the base of the first phalanx, demonstrated by magnetic resonance imaging (MRI). A biopsy reported: Malignant mixed tumor (myoepithelial carcinoma), ulcerated. The patient was scheduled for amputation of the first toe + inguinal lymphadenectomy, with pathological analysis confirming the initial diagnosis and metastasis 1/2 lymphatic nodes examined. Subsequently, the patient received radiotherapy on the inguinal area, total dose 66 Gy.
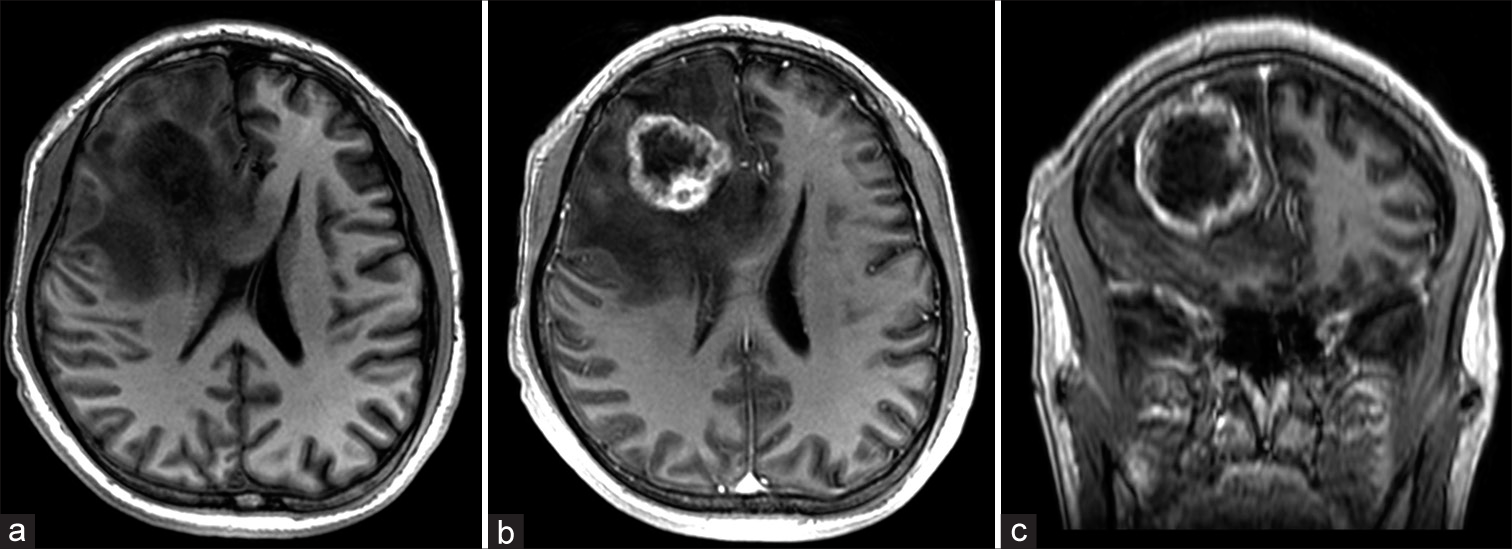
Three months after completing adjuvant therapy, the patient presented to the emergency department with headache and cognitive impairment. A contrast-enhanced brain MRI revealed an intra-axial single lesion located in the deep white matter of the right frontal lobe. Hypointense and heterogeneous in T1 and T2 sequences, with irregular edges and significant vasogenic edema conditioning compression and displacement of the anterior horn of the lateral ventricle [
Figure 1:
(a) T1-weighted axial magnetic resonance imaging (MRI) and (b) contrast-enhanced T1-weighted MRI showing a tumor within the frontal lobe with irregular peripheral enhance causing significant mass effect and midline shift; (c) contrast-enhanced T1-weighted coronal MRI showing tumor extension on the underlying brain parenchyma.
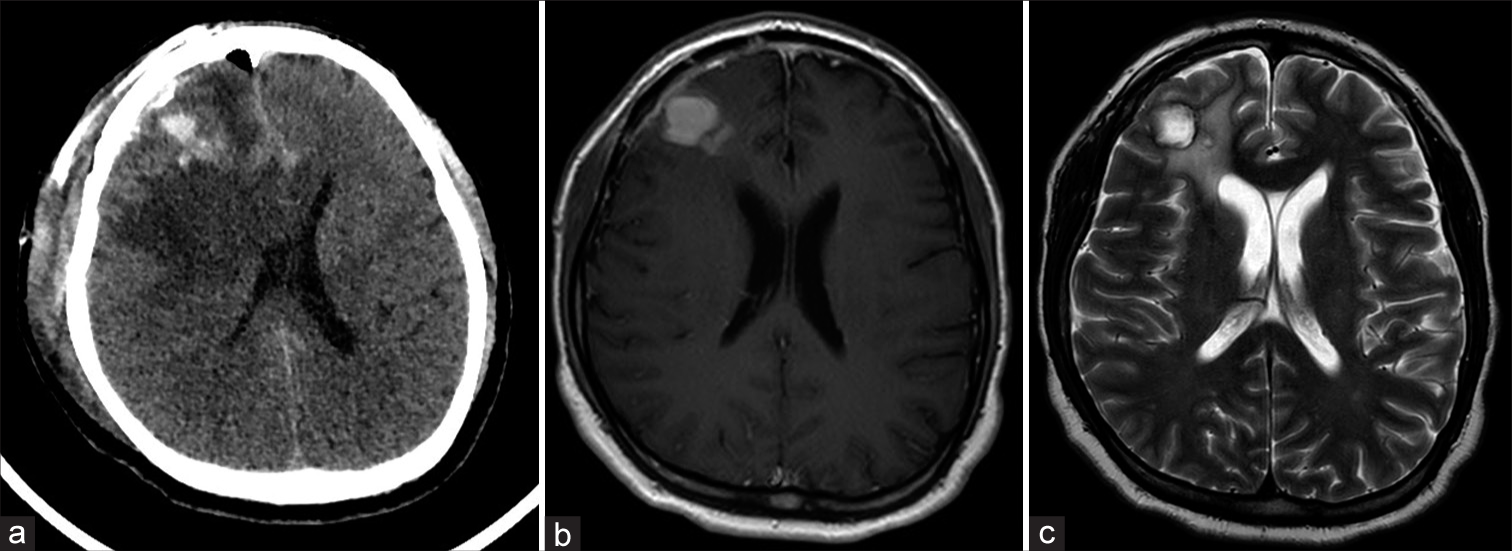
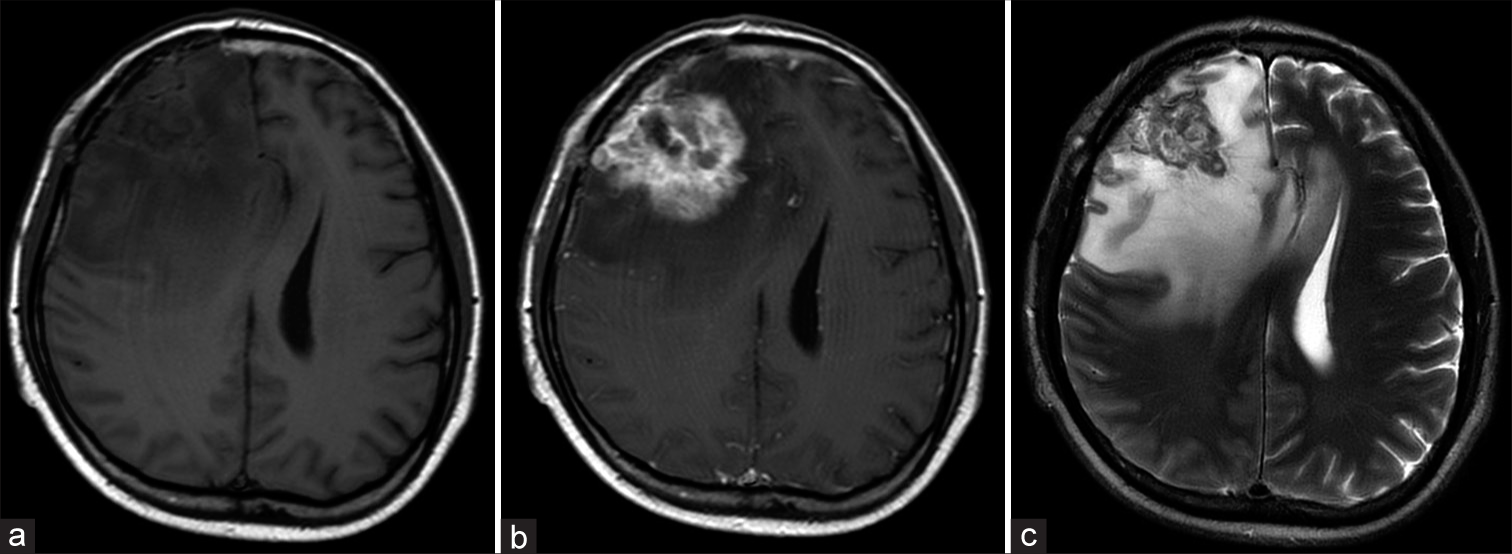
The patient did well for 7 months (Karnofsky index of 100), integrating himself into daily activities. He is currently under control but has returned to present headache and cognitive impairment (Karnofsky index of 60), a control MRI seven months after surgery evidenced a significant tumor recurrence in the frontal area accompanied again by perilesional edema and important mass effect [
DISCUSSION
Myoepithelial tumors are a rare form of salivary gland neoplasms composed entirely of myoepithelial cells that exhibit a dual epithelial and smooth muscle phenotype. Furthermore, the spectrum and classification of these tumors is diverse and complex. Although extensively described as a salivary gland tumor, soft-tissue phenotypes have been sparsely described. They are now increasingly being recognized in varied anatomical sites including head and neck (tongue, paranasal sinuses, pharynx, and larynx), breast, skin, vulva, respiratory, and gastrointestinal tract.[
Most commonly these tumors present as benign myoepitheliomas, but malignant myoepithelial carcinomas have been known to metastasize to the lungs, bone, soft tissue, skin, liver, and brain. As reported by Ren et al.,[
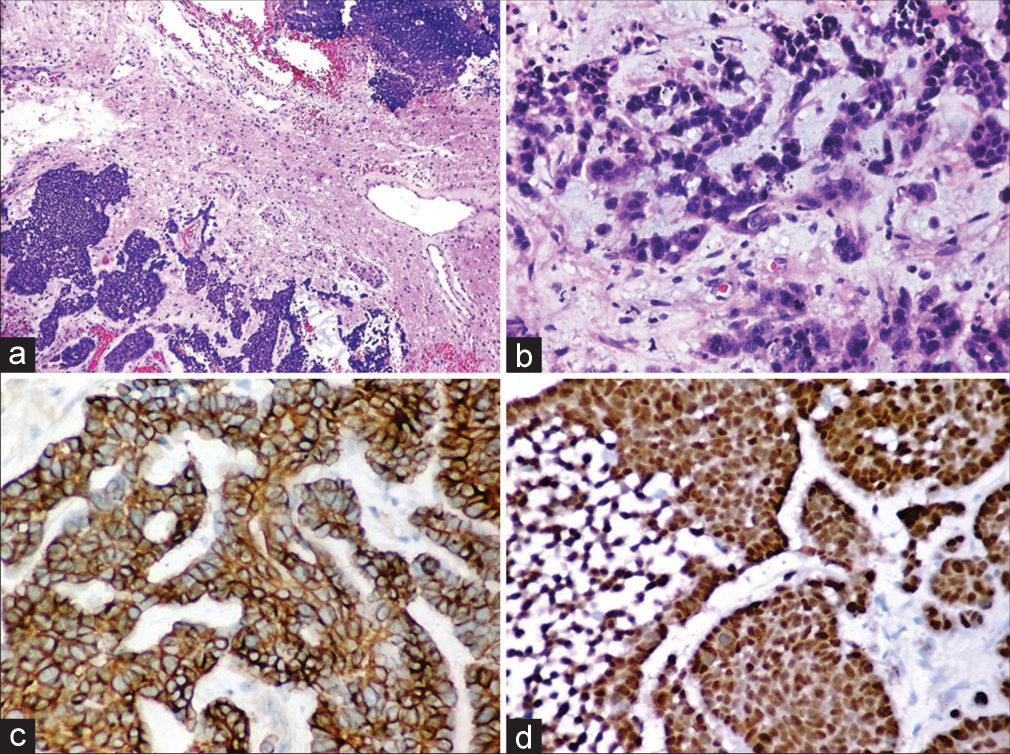
Preoperative diagnosis is difficult due to nonspecific clinical manifestations and imaging characteristics; thus, diagnosis can only be made based on histopathological and immunohistochemical analysis. Microscopically, these tumors exhibit a wide range of morphological heterogeneity, with the need for immunohistochemical analysis for accurate diagnosis. Furthermore, the accurate diagnosis is particularly important considering the high mortality related to tumor metastasis. Studies have described myoepithelial tumors with various morphological cellularities including spindle, epithelioid, plasmacytoid, clear, and stellate.[
Overall, in immunohistochemistry, most of the antibodies used to detect myoepithelial neoplasm target myofilament and keratin.[
This particularity, as postulated by Ellens et al.,[
Because central nervous system is a rare site for malignant myoepithelioma development, we found only a few cases reporting intracranial primary or metastatic malignant myoepithelioma with the help of PubMed. We found a compiled series of cases reported by other authors, where the most common sites of intracranial affection correspond to the sellar area, the cavernous sinus, the cerebellopontine angle, the dura, temporal lobe, and from direct extension from the orbital apex into the middle cranial fossa.[
The case illustrated herein is unique in some respects. Interestingly, the patient developed a single frontal lobe metastasis, being very unusual, and to our knowledge and due to the lack of data in the literature, the determination of this biological behavior and pattern of dissemination is challenging. Further, imaging did not show metastases elsewhere in the body.
Particularly due to its rarity, we did not find a consensus evidence-based treatment modality for intracranial malignant myoepithelioma.[
Radiation therapy is an important postsurgical adjuvant therapy, but evidence is not clear either, some authors report that is effective; however, other studies confirm the lack of effectiveness of this adjuvant treatment.[
Several factors have been postulated as possible prognostic markers: clinical stage, tumor location and size, high proliferative activity with extensive invasion of surrounding tissue, perineural permeation, abnormal presence of nuclear DNA content, and marked cellular pleomorphism.[
CONCLUSION
Tumors with myoepithelial differentiation occurring either as dura-based lesions or within the central nervous system are exceedingly rare, and as such, seldom considered in the spectrum of differential diagnoses for intracranial/ dura-based lesions. Metastatic intracranial myoepithelial carcinoma is an extremely rare tumor and may not possess many of the classic immunohistochemical features present in other myoepithelial tumors. At present, there is no standard therapy for these patients with metastatic spread of myoepithelial carcinoma to the central nervous system. Complete excision with tumor-free margin is always the preferred treatment, while adjuvant therapy is a suggestive treatment option, although this remains controversial. The prognosis of malignant myoepithelioma seems to be unfavorable; therefore, further information is needed to provide diagnostic and therapeutic recommendations for this rare intracranial lesion.
Search strategy and selection criteria
References for this Review were identified through searches of PubMed with the search terms “brain neoplasms,” “intracranial,” “neuro-oncology,” “myoepithelioma,” and “pathology” from 2000 to January, 2023. Articles were also identified through searches of the institution’ own files. Only papers published in Spanish and English were reviewed. The final reference list was generated based on originality and relevance to the broad scope of this review.
Author contributions
The authors confirm contribution to the paper as follows: Study Conception and Design: César Chong, Xavier Wong Achi; Data Collection: Xavier Wong Achi, Marlon Pozo, Janio Pico; Analysis and Interpretation of Results: César Chong, Xavier Wong Achi, Marlon Pozo; Draft Manuscript Preparation: Xavier Wong Achi, Marlon Pozo. All authors reviewed the results and approved the final version of the manuscript.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Choy B, Pytel P. Primary intracranial myoepithelial neoplasm: A potential mimic of meningioma. Int J Surg Pathol. 2016. 24: 243-7
2. Ellens N, Camelo-Piragua S, Ellens S, Simon J, Clark J. Metastasis of malignant myoepithelial carcinoma to the brain. BMJ Case Rep. 2018. 2018: bcr2018224285
3. Endo Y, Sugiura H, Yamashita H, Takahashi S, Yoshimoto N Iwas M. Myoepithelial carcinoma of the breast treated with surgery and chemotherapy. Case Rep Oncol Med. 2013. 2013: 164761
4. Gowripriya G, Sridhar K, Vij M. Intracranial myoepithelioma: A case report and review of literature. Neurol India. 2019. 67: 1347-51
5. Hayward D, Yoo D, Lee J, Wild E, Prabhu V. Myoepithelioma of the orbital apex and middle Cranial Fossa: Case report and review of the literature. Neuroophthalmology. 2014. 38: 14-20
6. Hong Y, Guo S, Chen S, Klebe D, Zhang J, Wu Q. Rapid-developed primary malignant myoepithelioma in the cavernous sinus: A case report. BMC Neurol. 2013. 13: 40
7. Hornick J, Fletcher CD. Myoepithelial tumors of soft tissue: A clinicopathologic and immunohistochemical study of 101 cases with evaluation of prognostic parameters. Am J Surg Pathol. 2003. 27: 1183-96
8. Hungermann D, Roeser K, Buerger H, Jäkel T, Löning T, Herbst H. Relative paucity of gross genetic alterations in myoepitheliomas and myoepithelial carcinomas of salivary glands. J Pathol. 2002. 198: 487-94
9. Jo V, Fletcher C. Myoepithelial neoplasms of soft tissue: An updated review of the clinicopathologic, immunophenotypic, and genetic features. Head Neck Pathol. 2015. 9: 32-8
10. Kong M, Drill E, Morris L, West L, Klimstra D, Gonen M. Prognostic factors in myoepithelial carcinoma of salivary glands: A clinicopathologic study of 48 cases. Am J Surg Pathol. 2015. 39: 931-8
11. Li L, Ho R, Tsang A. Coincidence of intracranial myoepithelioma and adrenocortical carcinoma in a young man. Asian J Neurosurg. 2021. 16: 598-602
12. Magrini E, Pragliola A, Farnedi A, Betts C, Cocchi R, Foschini M. Cytogenetic analysis of myoepithelial cell carcinoma of salivary gland. Virchows Arch. 2004. 444: 82-6
13. Nakatsu K, Kishi T, Kusano J, Hiratsuka Y, Ishigaki T. Postoperative intensity-modulated radiation therapy for myoepithelial carcinoma in the parotid gland. Cureus. 2022. 14: e21197
14. Noronha V, Cooper D, Higgins S, Murren J, Kluger H. Metastatic myoepithelial carcinoma of the vulva treated with carboplatin and paclitaxel. Lancet Oncol. 2006. 7: 270-1
15. Ren J, Liu Z, Liu X, Li Y, Zhang X, Li Z. Primary myoepithelial carcinoma of palate. World J Surg Oncol. 2011. 9: 104
16. Ugwuegbulem E, Hlaing S, deFreitas G, McIntosh W, Patel D. Impending doom: A rare case of metastatic myoepithelial carcinoma. Cureus. 2022. 14: e25785
17. Zeitouni N, Huang D, Row D. An unusual presentation and aggressive course of metastatic myoepithelial carcinoma. J Clin Aesthet Dermatol. 2019. 12: 46-8