- Department of Surgery, Suwa Central Hospital, Chino,
- Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, The University of Tokyo, Tokyo,
- Department of Internal Medicine, Suwa Central Hospital, Chino, Japan.
Correspondence Address:
Naoki Ishimaru, Department of Surgery, Suwa Central Hospital, Chino, Japan.
DOI:10.25259/SNI_444_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naoki Ishimaru1, Hirohisa Fujikawa2, Hirohisa Fujikawa3, Kazuya Niwa1. Unexpected findings during colon cancer surgery: A rare complication of ventriculoperitoneal shunt. 05-Aug-2022;13:339
How to cite this URL: Naoki Ishimaru1, Hirohisa Fujikawa2, Hirohisa Fujikawa3, Kazuya Niwa1. Unexpected findings during colon cancer surgery: A rare complication of ventriculoperitoneal shunt. 05-Aug-2022;13:339. Available from: https://surgicalneurologyint.com/surgicalint-articles/11767/
Abstract
Background: Complications such as infections and obstructions of the ventriculoperitoneal (VP) shunt are common. However, VP shunt trapped on the serosal side of colon cancer is rare, and there is no clear treatment strategy.
Case Description: A 72-year-old man presented with a 1-month history of constipation, diarrhea, and weight loss. His medical history consisted of subarachnoid hemorrhage and hydrocephalus 13 years earlier, for which endovascular coiling and VP shunting were performed. Colonoscopy showed a sigmoid mass, the biopsy of which revealed tubular adenocarcinoma. Computed tomography demonstrated circumferential wall thickening of the sigmoid colon without evidence of metastasis, with the lesion surrounding the tip of the VP shunt. He underwent laparoscopic surgery for sigmoid colon cancer. Unexpectedly, the VP shunt was trapped in the serous side of the tumor, and both the shunt and tumor were excised. Microscopic examination revealed inflammation and fibrosis, but no cancer cells were found in the serosa surrounding the embedded VP shunt tip.
Conclusion: Bowel perforation due to a VP shunt is a rare but emergency condition. If the perforation occurs around cancerous tissue, it must be handled with extreme care; excising the shunt along with the tumor may be the safest treatment method. Clinicians need to pay attention to the end of the VP shunt when performing surgery for patients with cancer and VP shunt.
Keywords: Colon cancer, Complications, Perforation, Serosal side, Ventriculoperitoneal shunt
INTRODUCTION
Complications such as infections and obstructions of the ventriculoperitoneal (VP) shunt are common. However, VP shunt trapped on the serosal side of colon cancer is rare, and there is no clear treatment strategy.
CASE REPORT
A 72-year-old man presented with a 1-month history of constipation, diarrhea, and weight loss. His medical history included subarachnoid hemorrhage and hydrocephalus 13 years previously, requiring endovascular coiling and ventriculoperitoneal (VP) shunt construction. Abdominal examination revealed hyperperistalsis and no tenderness. Colonoscopy showed a sigmoid mass [
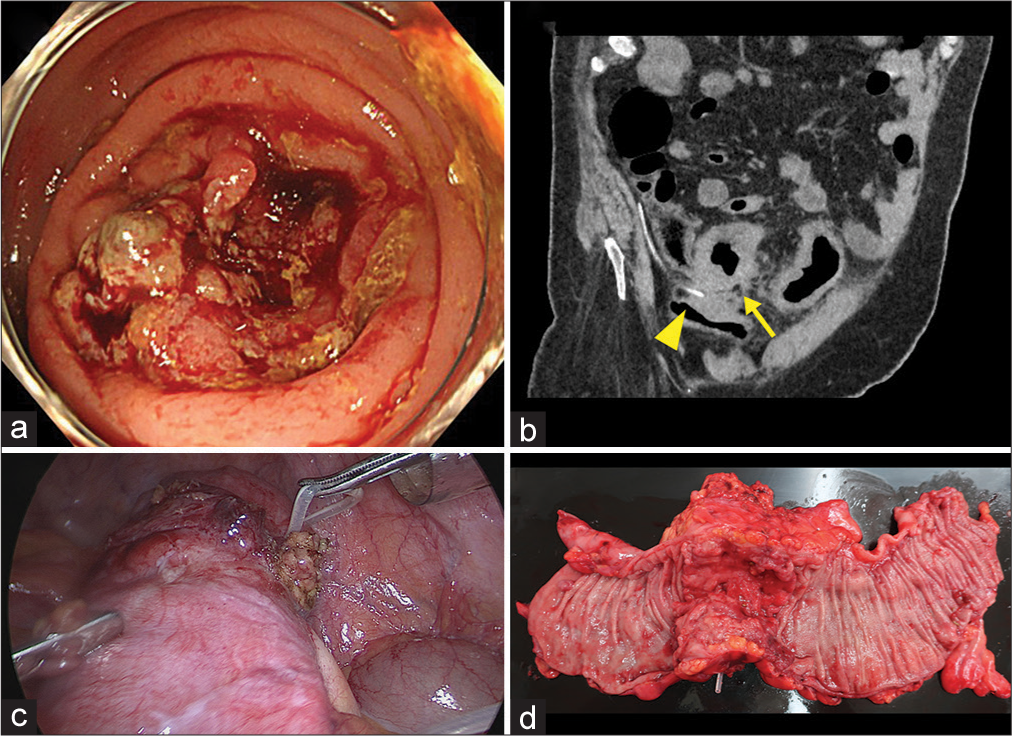
Figure 1:
(a) Colonoscopy photograph showing a circumferential lesion in the sigmoid colon that induced stenosis and prevented the scope from passing through. (b) Abdominal computed tomography revealing the sigmoid colon’s thickened wall (yellow arrow) and the ventriculoperitoneal (VP) shunt’s tip surrounded by the lesion (yellow arrowhead). (c) Laparoscopic photograph showing the VP shunt trapped in the tumor’s serosal side. (d) Resected tissue demonstrating the tip of the VP shunt that was removed along with the tumor. No catheter was found in the colonic lumen.
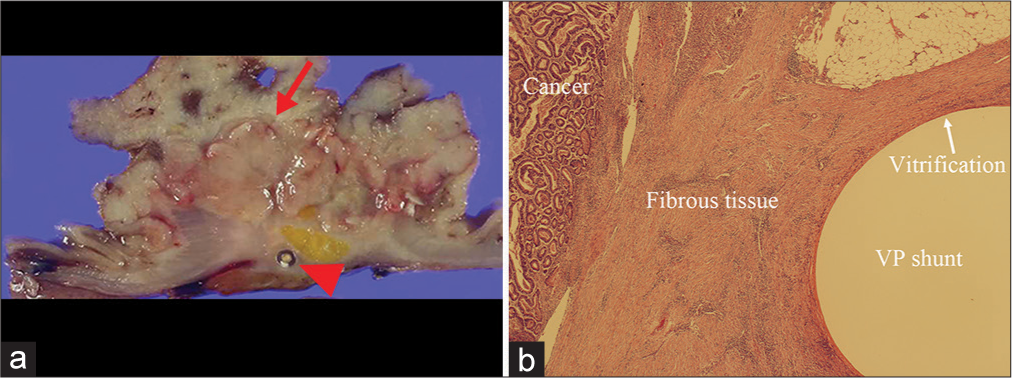
Figure 2:
(a) Macroscopic photograph showing the ventriculoperitoneal (VP) shunt (red arrowhead) embedded in a deeper layer than the tumor (red arrow). (b) Microscopic image revealing the VP shunt’s tip, covered in vitrification, located on the tumor’s serosal side. Fibrosis can be seen outside of the vitrification zone, but no cancer cells are observed (hematoxylin and eosin stain, original magnification ×20).
DISCUSSION
Hydrocephalus is the pathological accumulation of cerebrospinal fluid (CSF) in the ventricular system. The etiology of hydrocephalus can be congenital, acquired, or idiopathic. Hydrocephalus is primarily treated with a VP shunt implant that drains excess CSF from the cerebral ventricles into the peritoneal cavity. VP shunt complications are common, with most of them being obstructions and infections.[
Bowel perforation is a rare complication of VP shunt placement, occurring in only 0.1–0.7 % of cases.[
VP shunt-associated bowel perforation is a surgical emergency, and if the perforation is around cancerous tissue, it must be handled with great care. As the VP shunt in this case was trapped on the tumor’s serosal side, complete removal increased the risk of cancer cell dissemination or peritonitis. Therefore, excision of the shunt was deemed the safest treatment option. VP shunt placement is a common neurosurgical procedure, and clinicians often see patients post-VP shunt placement. VP shunt-related complications remain a major concern. When treating patients with cancer following VP shunt placement, clinicians should pay particular attention to the position of the end of the VP shunt and provide appropriate intervention.
CONCLUSION
Bowel perforation due to a VP shunt is a rare but emergency condition. If the perforation occurs around cancerous tissues, it must be handled with extreme care; excising the shunt along with the tumour may be the safest treatment method. Therfore, clincians need to pay attention to the end of the VP shunt when performing surgery for patients with cancer and VP shunt.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Brownlee JD, Brodkey JS, Schaefer IK. Colonic perforation by ventriculoperitoneal shunt tubing: A case of suspected silicone allergy. Surg Neurol. 1998. 49: 21-4
2. Paff M, Alexandru-Abrams D, Muhonen M, Loudon W. Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg. 2018. 13: 66-70
3. Thiong’o GM, Luzzio C, Albright AL. Ventriculoperitoneal shunt perforations of the gastrointestinal tract. J Neurosurg Pediatr. 2015. 16: 36-41