- Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Udayana University, Prof. Dr. I.G.N.G. Ngoerah General Hospital, Denpasar, Indonesia
Correspondence Address:
Marthinson Andrew Tombeng, Division of Neurosurgery, Department of Surgery, Faculty of Medicine, Udayana University, Prof. Dr. I.G.N.G. Ngoerah General Hospital, Denpasar, Indonesia.
DOI:10.25259/SNI_526_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marthinson Andrew Tombeng, Christopher Lauren, Tjokorda Gde Bagus Mahadewa. Unilateral percutaneous balloon kyphoplasty for thoracic osteoporotic vertebral compression fractures: A case report and literature review. 30-Aug-2024;15:311
How to cite this URL: Marthinson Andrew Tombeng, Christopher Lauren, Tjokorda Gde Bagus Mahadewa. Unilateral percutaneous balloon kyphoplasty for thoracic osteoporotic vertebral compression fractures: A case report and literature review. 30-Aug-2024;15:311. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13070
Abstract
Background: Unilateral percutaneous balloon kyphoplasty (PBK) is increasingly utilized for the management of osteoporotic vertebral compression fractures (OVCFs). Its potential advantages include procedural simplicity, reduced tissue trauma, and minimal radiation exposure.
Case Description: A 59-year-old female with osteoporosis presented with back pain but was neurologically intact 2 weeks after a fall. The magnetic resonance imaging documented a thoracic 12 vertebral compression fracture that was successfully treated with a unilateral PBK.
Conclusion: Unilateral PBK appears promising for managing OVCFs in the aging population and offers rapid pain relief, vertebral height restoration, and functional improvement.
Keywords: Age-related osteoporosis, Kyphoplasty, Neurosurgical procedures, Vertebral column
INTRODUCTION
Percutaneous balloon kyphoplasty (PBK) has emerged as a safe and effective minimally invasive procedure for addressing osteoporotic vertebral compression fractures (OVCFs).[
CASE DESCRIPTION
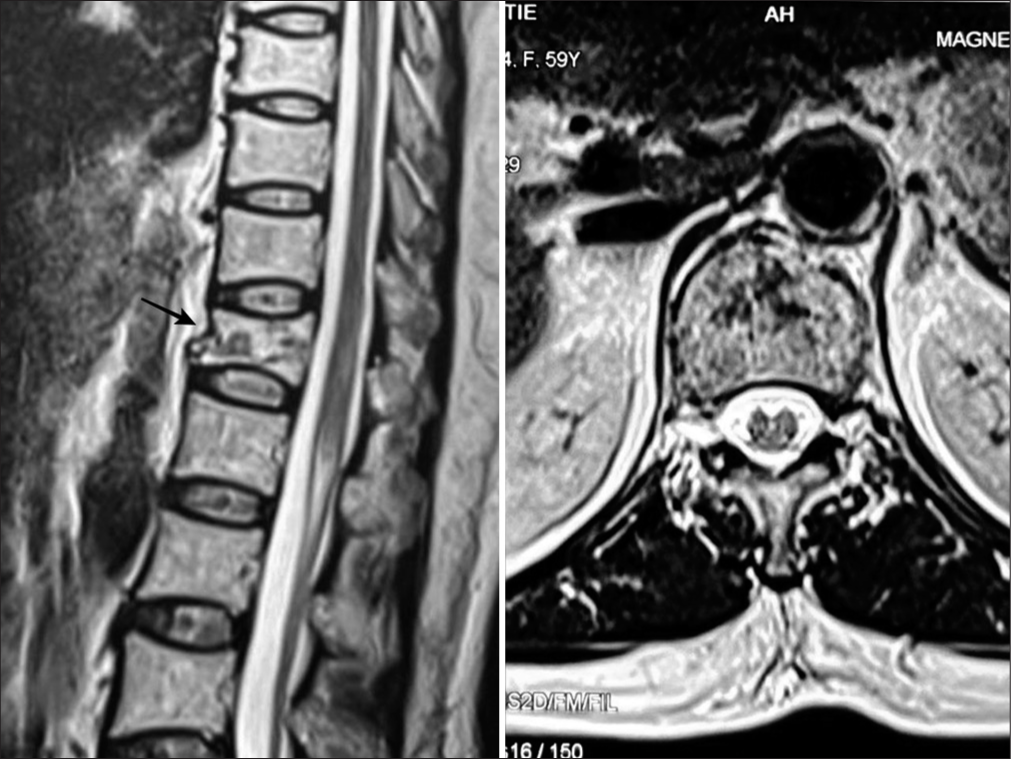
A 59-year-old female with osteoporosis presented 2 weeks following a fall with back pain but without a neurological deficit. The pain on the Visual Analog Scale (VAS) was 8/10, and the Oswestry Disability Index (ODI) score was 40%. The thoracic magnetic resonance imaging revealed a Th12 OVCF [
Operative procedure
Under general anesthesia, a unilateral PBK was performed with the patient prone [
Figure 2:
Intraoperative procedure. (a) Trocar insertion site is located approximately 4 cm to the right of the midline. (b and c) Balloon inflation to approximately 4 cc, as shown in the C-arm images in (b) anteroposterior (AP) and (c) lateral views. (d and e) C-Arm images (d) immediately and (e) after PMMA injection.
Follow-up and outcome
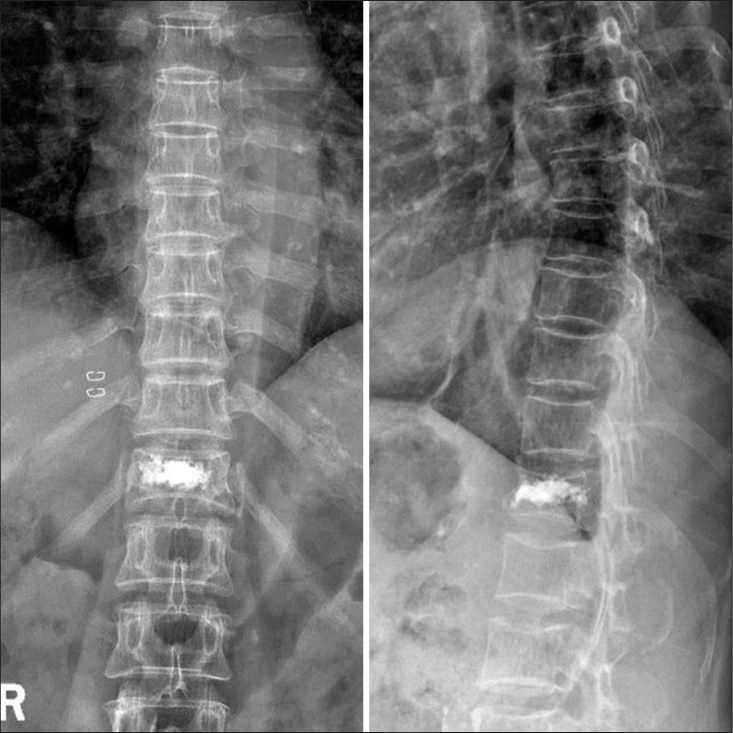
Postoperatively, back pain significantly improved, i.e., the VAS score improved to 2/10. X-rays showed restoration of both the vertebral height and alignment [
DISCUSSION
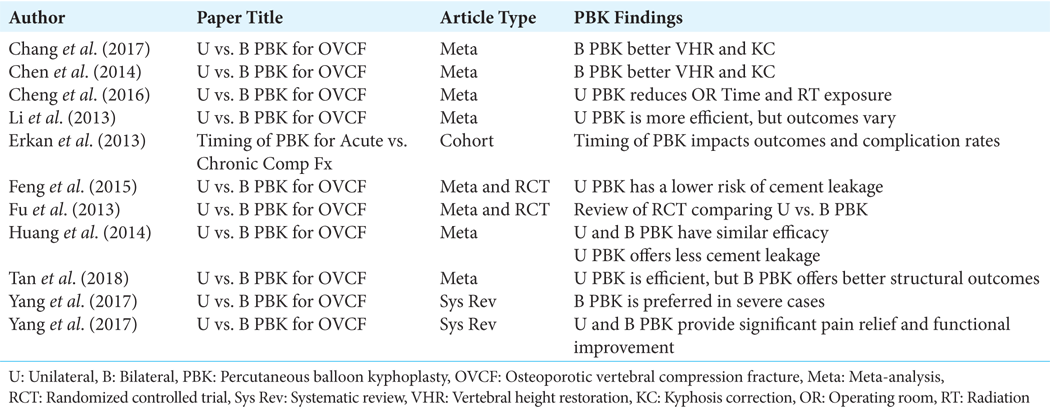
The primary goals of PBK surgery for OVCF patients are to reduce back pain, restore vertebral height/alignment, and improve patient mobilization. Although several meta-analyses have documented significant short-term improvement in VAS scores for unilateral versus bilateral PBK, no significant differences were found for long-term follow-ups.[
CONCLUSION
Unilateral PBK is a promising technique for treating OVCFs. Potential benefits include more pain relief, better functional improvement, and reduced surgical complexity versus routine bilateral approaches.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chang W, Zhang X, Jiao N, Yuwen P, Zhu Y, Zhang F. Unilateral versus bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures: A meta-analysis. Medicine. 2017. 96: e6738
2. Chen H, Tang P, Zhao Y, Gao Y, Wang Y. Unilateral versus bilateral balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Orthopedics. 2014. 37: e828-35
3. Cheng X, Long HQ, Xu JH, Huang YL, Li FB. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): A systematic review and meta-analysis. Eur Spine J. 2016. 25: 3439-49
4. Erkan S, Ozalp TR, Yercan HS, Okcu G. Does timing matter in performing kyphoplasty? Acute versus chronic compression fractures. Acta Orthop Belg. 2009. 75: 396-404
5. Feng H, Huang P, Zhang X, Zheng G, Wang Y. Unilateral versus bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures: A systematic review and meta-analysis of RCTs. J Orthop Res. 2015. 33: 1713-23
6. Fu Q, Yang LY, Wang XL, Zhou L. Systematic review a systematic review and meta-analysis of randomized controlled trials of unilateral versus bilateral kyphoplasty for osteoporotic vertebral compression fractures. Pain Physician. 2013. 16: 277-90
7. Huang Z, Wan S, Ning L, Han S. Is unilateral kyphoplasty as effective and safe as bilateral kyphoplasties for osteoporotic vertebral compression fractures? A Meta-analysis. Clin Orthop Relat Res. 2014. 472: 2833
8. Li LH, Sun TS, Liu Z, Zhang JZ, Zhang Y, Cai YH. Comparison of unipedicular and bipedicular percutaneous kyphoplasty for treating osteoporotic vertebral compression fractures: A meta-analysis. Chin Med J (Engl). 2013. 126: 3956-61
9. Tan G, Li F, Zhou D, Cai X, Huang Y, Liu F. Unilateral versus bilateral percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures a systematic review of overlapping meta-analyses. Medicine (Baltimore). 2018. 97: e11968
10. Yang H, Lin J, Zhang L. Systematic review unilateral versus bilateral balloon kyphoplasty for osteoporotic vertebral compression fractures. Pain Physician. 2019. 22: 15-28
11. Yang S, Chen C, Wang H, Wu Z, Liu L. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/ percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Orthop Traumatol Turc. 2017. 51: 290