- Virginia Tech Carilion School of Medicine, Riverside Circle, Roanoke, Virginia, USA
- Institute for Orthopedics and Neurosciences, Carilion Clinic, Roanoke, Virginia, USA
- Rothman Institute at Jefferson, Philadelphia, Pennsylvania, USA
Correspondence Address:
Alireza K. Nazemi
Virginia Tech Carilion School of Medicine, Riverside Circle, Roanoke, Virginia, USA
Institute for Orthopedics and Neurosciences, Carilion Clinic, Roanoke, Virginia, USA
DOI:10.4103/sni.sni_460_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Alireza K. Nazemi, Anirudh K. Gowd, Alexander R. Vaccaro, Jonathan J. Carmouche, Caleb J. Behrend. Unilateral S2 alar-iliac screws for spinopelvic fixation. 09-Apr-2018;9:75
How to cite this URL: Alireza K. Nazemi, Anirudh K. Gowd, Alexander R. Vaccaro, Jonathan J. Carmouche, Caleb J. Behrend. Unilateral S2 alar-iliac screws for spinopelvic fixation. 09-Apr-2018;9:75. Available from: http://surgicalneurologyint.com/surgicalint-articles/unilateral-s2-alar%e2%80%91iliac-screws-for-spinopelvic-fixation/
Abstract
Background:This study compared the clinical complications, radiographic measurements of deformity, and quality of life outcomes for patients with de novo scoliosis undergoing thoracolumbar fusions for spinopelvic fixation (SPF) utilizing unilateral S2 alar-iliac (S2AI) screw or unilateral iliac bolt fixation.
Methods:This retrospective review was performed in 29 patients who underwent SPF at one institution; 10 patients received unilateral S2AI screws, and 19 patients received unilateral iliac bolts. The following variables were studied: reoperation rates, pseudarthrosis, sacral insufficiency fracture, hardware prominence, infection, proximal junctional kyphosis (PJK), deformity correction (radiographs), windshield wipering, hardware fracture, and hardware removal. Outcomes were analyzed utilizing both the visual analog scale (VAS) and Oswestry Disability Index (ODI). The mean follow-up period was 27 months.
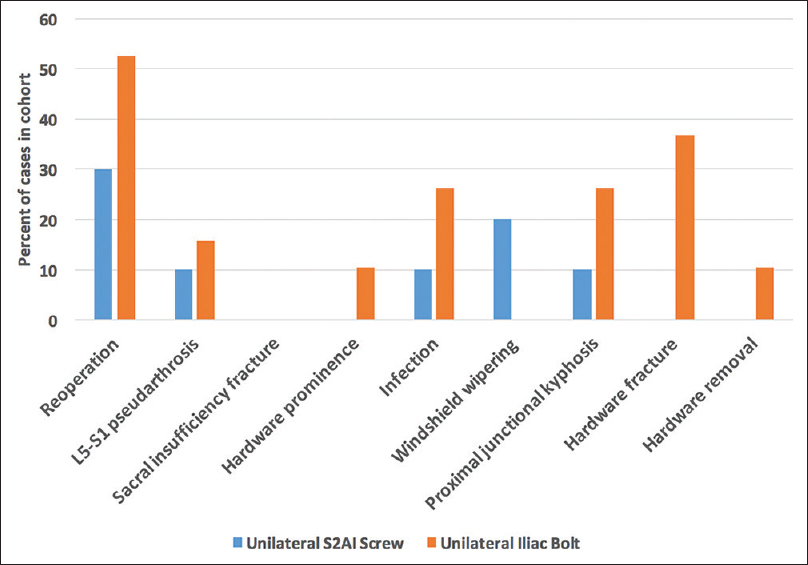
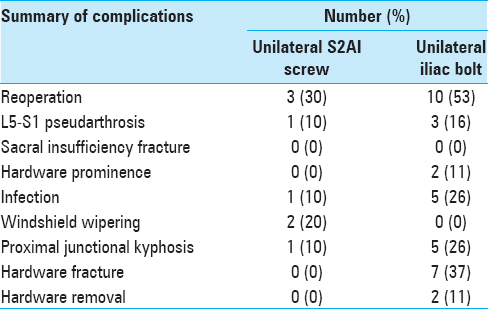
Results:The reoperation rate for unilateral S2AI screws was 30% vs. 53% for unilateral iliac bolts (P = 0.43); reoperations were performed with a 1:5 ratio for infection, a 1:4 ratio for pseudarthrosis, and 1:1 a ratio for PJK comparing S2AI screws to iliac bolts, respectively.
Conclusion:There were no significant differences in postoperative complications and reoperation rates between unilateral S2AI screws and unilateral iliac bolts utilized for SPF. For the S2AI screw group, there were no instances of hardware prominence or need for removal. The use of unilateral S2AI screws resulted in adequate fixation and comparably low complication rates.
Keywords: Iliac bolts, reoperation rates, S2 alar-iliac screws, spinopelvic fixation, unilateral fixation
INTRODUCTION
Some traditional spinopelvic fixation (SPF) techniques have high reported complication rates.[
MATERIALS AND METHODS
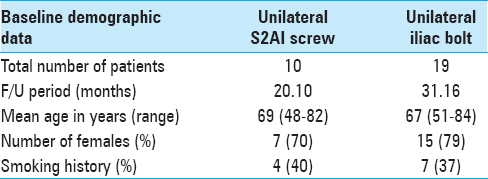
Deformity correction, complication rates, and outcomes were studied in patients undergoing unilateral S2AI screws vs. unilateral iliac bolts for SPF for de novo scoliosis or kyphosis. Nineteen patients received unilateral iliac bolts vs. 10 who received unilateral S2AI screws [
Charts were reviewed for reoperation rates, L5-S1 pseudarthrosis, sacral insufficiency fracture, hardware prominence, infection, proximal junctional kyphosis (PJK), windshield wipering, hardware fracture, and hardware removal.
Radiographic and clinical assessment of outcomes
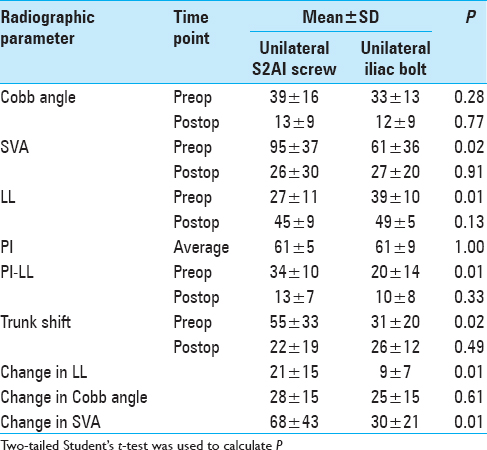
All radiographic measurements utilized the Surgimap Spine 2.2.10 (Nemaris Inc., New York, NY, USA) software and included assessment of lumbar lordosis (LL), pelvic tilt (PT), pelvic incidence (PI), PI-LL mismatch, sagittal vertical axis (SVA), Cobb angle, and trunk shift.
Statistical evaluation
Fisher's exact test or Pearson Chi-square tests determined the statistical significance for reoperation rates. For continuous variables, a two-tailed Student's t-test was performed. Statistical significance was set at P < 0.05.
RESULTS
Radiographic outcomes
Utilizing postoperative lumbar posterioanterior and lateral films (1.5 and 3 months) and full-length scoliosis standing radiographs (0.5 and 1 year) [
Figure 1
Preoperative and two-year postoperative posteroanterior and lateral radiographs of spinopelvic fixation in (upper row) a patient who underwent direct lateral interbody fusion (DLIF) L2-L5 and SPF with a unilateral S2 sacro-iliac screw and (lower row) a patient who underwent SPF with a unilateral iliac bolt
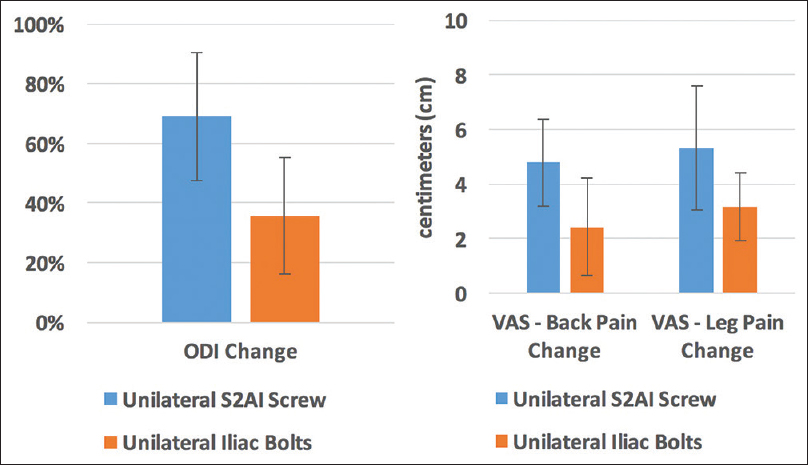
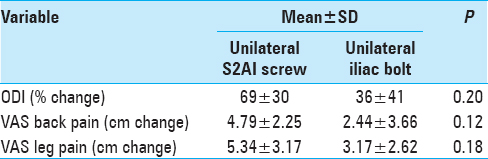
The VAS and ODI showed no significant difference between the two groups [
Figure 3
Change in clinical quality of life measures including (left) Oswestry disability index (ODI), (right) visual analog scale (VAS) for back pain and VAS for leg pain. Preoperative and most recent postoperative measurements are used to measure change for both the unilateral S2AI screw and unilateral iliac bolt groups. Error bars indicate 95% confidence interval
Postoperative complications
The reoperation rate for unilateral S2AI screws was 30% vs. a 53% rate for unilateral iliac bolts; reoperations were for infection (1 vs. 5), pseudarthrosis (1 vs. 4), and PJK (1 vs. 1) [
DISCUSSION
The present study provides comparative clinical data of SPF constructs using unilateral S2AI screws vs. unilateral iliac bolts. Here, no significant differences were found between the two groups regarding change in quality of life measures (ODI, VAS for back pain, and VAS for leg pain). Furthermore, both groups achieved significant clinical improvement using accepted values of minimal clinically important difference of 20%.[
The reoperation rate for unilateral S2AI screws was comparable to the unilateral iliac bolts; these data were comparable to those found in two published retrospective series.[
CONCLUSIONS
This study documented no significant differences in postoperative complications for unilateral S2AI screws vs. unilateral iliac bolts for performing SPF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Burns CB, Dua K, Trasolini NA, Komatsu DE, Barsi JM. Biomechanical comparison of spinopelvic fixation constructs: Iliac screw versus S2-alar-iliac screw. Spine Deform. 2016. 4: 10-5
2. Ilyas H, Place H, Puryear A. A comparison of early clinical and radiographic complications of iliac screw fixation versus S2 alar iliac (S2AI) fixation in the adult and pediatric populations. J Spinal Disord Tech. 2015. 28: E199-E205
3. Mazur MD, Ravindra VM, Schmidt MH, Brodke DS, Lawrence BD, Riva-Cambrin J. Unplanned reoperation after lumbopelvic fixation with S-2 alar-iliac screws or iliac bolts. J Neurosurg Spine. 2015. 23: 67-76
4. Saigal R, Lau D, Wadhwa R, Le H, Khashan M, Berven S. Unilateral versus bilateral iliac screws for spinopelvic fixation: Are two screws better than one?. Neurosurg Focus. 2014. 36: E10-
5. Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med. 2008. p. 161-3
6. Weistroffer JK, Perra JH, Lonstein JE, Schwender JD, Garvey TA, Transfeldt EE. Complications in long fusions to the sacrum for adult scoliosis: Minimum five-year analysis of fifty patients. Spine (Phila Pa. 1976. 2008;33: 1478-83