- Department of Neuroscience (Neurosurgery), Winthrop University Hospital, Mineola, NY 11501, USA
Correspondence Address:
Nancy E. Epstein
Department of Neuroscience (Neurosurgery), Winthrop University Hospital, Mineola, NY 11501, USA
DOI:10.4103/2152-7806.163958
Copyright: © 2015 Epstein NE. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Epstein NE. Unnecessary multiple epidural steroid injections delay surgery for massive lumbar disc: Case discussion and review. Surg Neurol Int 31-Aug-2015;6:
How to cite this URL: Epstein NE. Unnecessary multiple epidural steroid injections delay surgery for massive lumbar disc: Case discussion and review. Surg Neurol Int 31-Aug-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/unnecessary-multiple-epidural-steroid-injections-delay-surgery-for/
Abstract
Background:Epidural steroid injections (ESI) in the lumbar spine are not effective over the long-term for resolving “surgical” lesions. Here, we present a patient with a massive L2–L3 lumbar disk herniation whose surgery was delayed for 4 months by multiple unnecessary ESI, resulting in a cauda equina syndrome.
Methods:A 54-year-old male acutely developed increased low back and radiating left leg pain in October of 2014. In December of 2014, a magnetic resonance imaging (MRI) scan showed a massive central/left sided disk herniation at the L2–L3 level resulting in marked thecal sac and left L2 foraminal and L3 lateral recess root compression. Despite the marked degree of neural compression, pain management treated him with 3 ESI over the next 3 months.
Results:At the end of April of 2015, he presented to spine surgeon with a cauda equina syndrome. When the new MRI scan confirmed the previously documented massive central-left sided L2–L3 disk herniation, the patient emergently underwent an L1–L3 laminectomy with central-left sided L2–L3 lateral/foraminal diskectomy. Postoperatively, the patient was neurologically intact.
Conclusions:Pain specialists performed multiple unnecessary lumbar ESI critically delaying spinal surgery for 4 months in this patient with a massive lumbar disk herniation who ultimately developed a cauda equina syndrome. Unfortunately, pain specialists (e.g., radiologists, anesthesiologists, and physiatrists), not specifically trained to perform neurological examinations or spinal surgery, are increasingly mismanaging spinal disease with ESI/variants. It is time for spine surgeons to speak out against this, and “take back” the care of patients with spinal surgical disease.
Keywords: Cauda equina syndrome, epidural steroid injections/variants, lumbar disk herniation, massive discs, pain specialists, spinal surgeons, unnecessary delay
INTRODUCTION
Pain management specialists, typically comprised of radiologists, physiatrists, and anesthesiologists, who are neither trained to perform neurological examinations or spinal surgery, are increasingly performing not only epidural spinal injections (ESI) and their variants, but even on occasion, “spinal surgery” (e.g., percutaneous discectomy). Most studies show ESI/variants have no long-term efficacy, and not only expose patients to the major risks and complications of the injections themselves, but also lead to critical delays in surgery that may lead to permanent neurological injury.[
CASE REPORT
A 54 year-old-male developed acute, radiating left sided low back, thigh, and buttock pain in October 2014. In December of 2014, an initial lumbar MRI documented a massive central-left sided disc nearly filling the spinal canal at the L2–L3 level accompanied by left foraminal/lateral recess compression of the L2 and L3 roots respectively [Figures
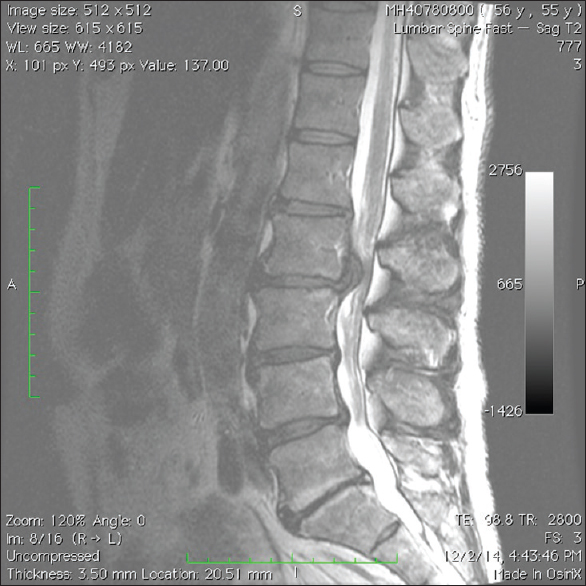
Figure 1
The preoperative December 2014 magnetic resonance imaging parasagittal study documented a massive central-left sided L2–L3 lumbar disk herniation resulting in severe thecal sac and left L2 and L3 foraminal/lateral recess root compression respectively. Notably the right mild/moderate sequestrated L4–L5 disc was asymptomatic
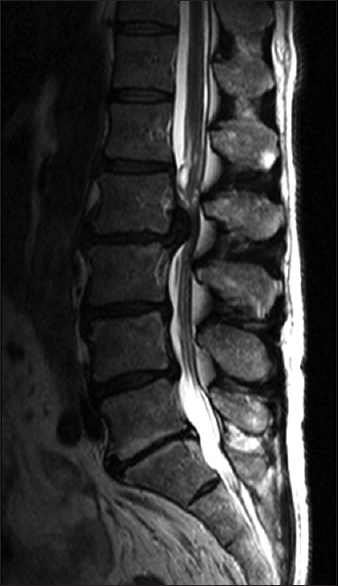
Figure 3
The immediate preoperative April 2015 parasagittal magnetic resonance imaging study documented the same massive central-left sided L2–L3 lumbar disk herniation seen on the magnetic resonance imaging from December of 2014. It still resulted in severe central-left sided thecal sac and left L2 and L3 foraminal/lateral recess root compression respectively
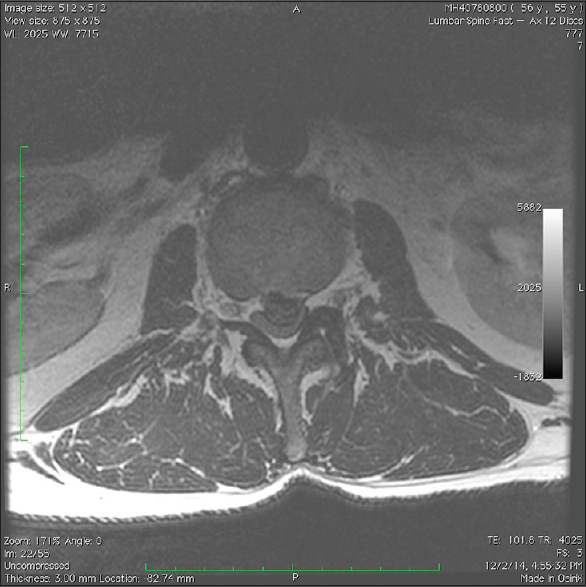
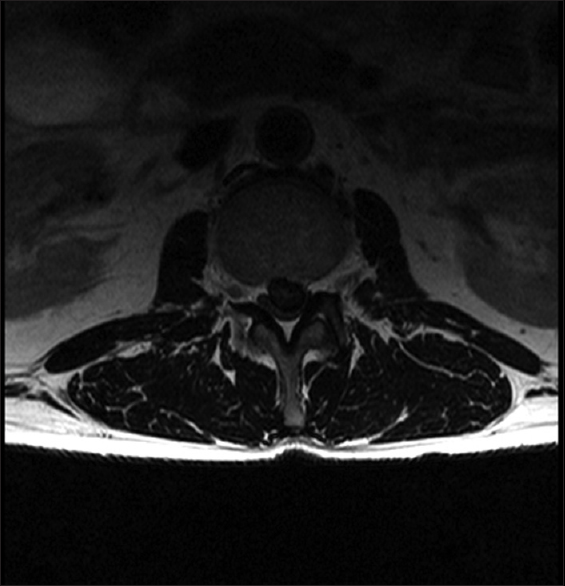
Figure 4
The immediate preoperative April 2015 axial magnetic resonance imaging study documented the same massive central-left sided L2–L3 lumbar disk herniation seen on the magnetic resonance imaging from December of 2014. It still resulted in severe central-left sided thecal sac and left L2 and L3 foraminal/lateral root compression respectively
FREQUENCY OF EPIDURAL/TRANSFORAMINAL FLUOROSCOPIC SPINAL INJECTIONS
Low back pain/sciatica accounts for 13% (the second most common) of the reasons for medical office visits in the US.[
EQUAL EFFICACY OF EPIDURAL VERSUS OTHER INJECTIONS PERFORMED WITH/WITHOUT STEROIDS
ESI/TLESI are equally effective as other types/locations of injections performed with/without steroids. In a randomized, double-blind trial, Carette et al. documented that ESI utilizing methylprednisolone acetate (80 mg methylprednisolone in 8 ml of isotonic saline) versus epidural injections performed with isotonic saline (1 ml) alone were equally effective when administered 3 times per patient in the management of sciatica.[
MULTIPLE COMPLICATIONS OF ESI/TLESI ARE OFTEN UNDERREPORTED
Many studies cite the fact that the multiple complications of ESI/TLESI/TFLESI injections are often underreported [
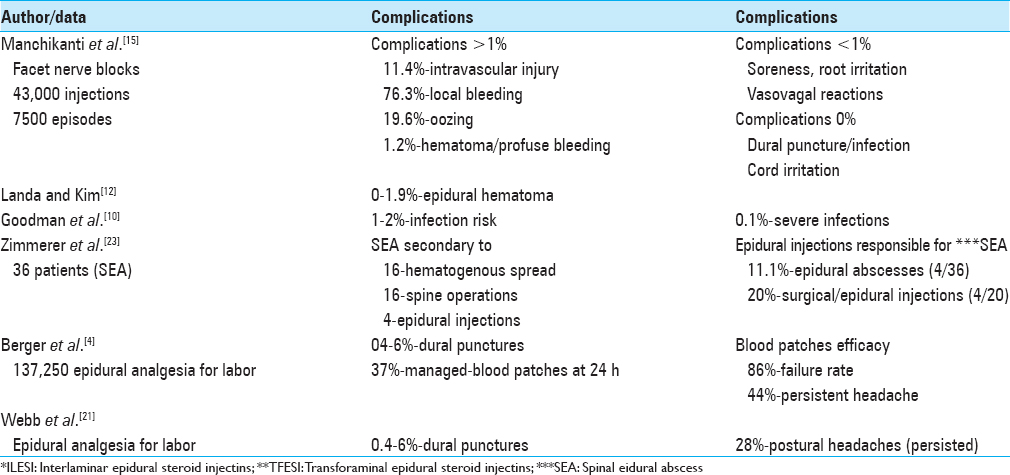
Table 1
Complications and outcomes of spinal interlaminar epidural steroid injections and and transforaminal epidural steroid injections (modified)[
ESI AVERT SURGERY IN PATIENTS WITH “SURGICAL” DISC DISEASE
In Riew et al. prospective, randomized, controlled, double-blind study, the authors compared the efficacy of selective nerve root injections utilizing bupivacaine/steroid (28 patients) versus bupivacaine alone (27 patients) in patients with radiculopathy attributed to “surgical” disk herniations.[
EPIDURAL STEROIDS DO NOT REDUCE NEED FOR SPINAL SURGERY
For truly surgical spinal lesions, epidural injections (ESI, TLESI, TFLESI) do not avoid/reduce the need for surgery. In Carette et al. randomized double blind trial for patients with disc disease, epidural steroids vs. epidural isotonic saline injections, “offered no significant functional benefit, nor did it reduce the need for surgery” up to 1-year later.[
CONCLUSION
ESI/TLESI/TFESI are the most commonly performed procedures in the US for managing chronic low back pain. The procedures are not Food and Drug Administration (FDA) approved for this application, and are associated with major risks/complications.[
References
1. Anderberg L, Annertz M, Persson L, Brandt L, Säveland H. Transforaminal steroid injections for the treatment of cervical radiculopathy: A prospective and randomised study. Eur Spine J. 2007. 16: 321-8
2. Andersson GB. Epidural glucocorticoid injections in patients with lumbar spinal stenosis. N Engl J Med. 2014. 371: 75-6
3. Arden NK, Price C, Reading I, Stubbing J, Hazelgrove J, Dunne C. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: The WEST study. Rheumatology (Oxford). 2005. 44: 1399-406
4. Berger CW, Crosby ET, Grodecki W. North American survey of the management of dural puncture occurring during labour epidural analgesia. Can J Anaesth. 1998. 45: 110-4
5. Bicket MC, Horowitz JM, Benzon HT, Cohen SP. Epidural injections in prevention of surgery for spinal pain: Systematic review and meta-analysis of randomized controlled trials. Spine J. 2015. 15: 348-62
6. Carette S, Leclaire R, Marcoux S, Morin F, Blaise GA, St-Pierre A. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997. 336: 1634-40
7. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: A comprehensive, evidence-based review. Reg Anesth Pain Med. 2013. 38: 175-200
8. Epstein NE. The risks of epidural and transforaminal steroid injections in the Spine: Commentary and a comprehensive review of the literature. Surg Neurol Int. 2013. 4: S74-93
9. Friedly JL, Bresnahan BW, Comstock B, Turner JA, Deyo RA, Sullivan SD. Study protocol-Lumbar Epidural steroid injections for Spinal Stenosis (LESS): A double-blind randomized controlled trial of epidural steroid injections for lumbar spinal stenosis among older adults. BMC Musculoskelet Disord. 2012. p. 13-48
10. Goodman BS, Posecion LW, Mallempati S, Bayazitoglu M. Complications and pitfalls of lumbar interlaminar and transforaminal epidural injections. Curr Rev Musculoskelet Med. 2008. 1: 212-22
11. Hooten WM, Kinney MO, Huntoon MA. Epidural abscess and meningitis after epidural corticosteroid injection. Mayo Clin Proc. 2004. 79: 682-6
12. Landa J, Kim Y. Outcomes of interlaminar and transforminal spinal injections. Bull NYU Hosp Jt Dis. 2012. 70: 6-10
13. Manchikanti L, Candido KD, Kaye AD, Boswell MV, Benyamin RM, Falco FJ. Randomized trial of epidural injections for spinal stenosis published in the New England Journal of Medicine: Further confusion without clarification. Pain Physician. 2014. 17: E475-88
14. Manchikanti L, Cash KA, McManus CD, Pampati V, Fellows B. Results of 2-year follow-up of a randomized, double-blind, controlled trial of fluoroscopic caudal epidural injections in central spinal stenosis. Pain Physician. 2012. 15: 371-84
15. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: A prospective evaluation of 7,500 episodes with 43,000 nerve blocks. Pain Physician. 2012. 15: E143-50
16. Parr AT, Diwan S, Abdi S. Lumbar interlaminar epidural injections in managing chronic low back and lower extremity pain: A systematic review. Pain Physician. 2009. 12: 163-88
17. Pollack A.editors. Before a Wave of Meningitis, Shots Were Tied to Risks. Health: New York Times, October, 11; 2012. p. 18-
18. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000. 82-A: 1589-93
19. Rosas HG, Lee KS. Performing fluoroscopically guided interlaminar lumbar epidural injections. AJR Am J Roentgenol. 2012. p. 199-419
20. Valat JP, Giraudeau B, Rozenberg S, Goupille P, Bourgeois P, Micheau-Beaugendre V. Epidural corticosteroid injections for sciatica: A randomised, double blind, controlled clinical trial. Ann Rheum Dis. 2003. 62: 639-43
21. Webb CA, Weyker PD, Zhang L, Stanley S, Coyle DT, Tang T. Unintentional dural puncture with a Tuohy needle increases risk of chronic headache. Anesth Analg. 2012. 115: 124-32
22. Wilson-MacDonald J, Burt G, Griffin D, Glynn C. Epidural steroid injection for nerve root compression. A randomised, controlled trial. J Bone Joint Surg Br. 2005. 87: 352-5
23. Zimmerer SM, Conen A, Müller AA, Sailer M, Taub E, Flückiger U. Spinal epidural abscess: Aetiology, predisponent factors and clinical outcomes in a 4-year prospective study. Eur Spine J. 2011. 20: 2228-34






hamed gomez
Posted September 15, 2015, 12:34 am
thank`s for your report.
I have a young patient who arrives to emergency with a month of palsy of right L5 and s1nerves.
the MRI shows a multilevel lumbar discopathy (L3 – L4, L4 – L5. L5 – s1), and electrodiagnosis shows L5 radiculopathy with denervation.
What do you thing about the approach to a young patient (30 Y), obese with a month of palsy and 3 lumbar disc herniated.
thak`s for your attention.
James Whitaker
Posted May 16, 2018, 6:13 am
It is inaccurate to state that physiatrists are not trained to do Neuro examinations. Physiatrists are very well trained because they treat patients with spinal cord injuries, stroke and traumatic brain injuries as well as those with spinal stenosis or radiculopathies. The ASIA examination for spinal cord injuries is an example of the level of expertise physiatrists have with neurological examinations.
The real issue here is knowing when to refer patients to a spine surgeon.
Stephen
Posted October 13, 2022, 7:50 pm
And is there a possible conflict of interest to NOT refer patients to a spine surgeon until after three injections in one year?