- Department of Neurosurgery, Clinical Research Institute, National Hospital Organization, Kyushu Medical Center, Japan
Correspondence Address:
Sei Haga
Department of Neurosurgery, Clinical Research Institute, National Hospital Organization, Kyushu Medical Center, Japan
DOI:10.4103/2152-7806.143366
Copyright: © 2014 Haga S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Haga S, Nagata S. Usefulness of continuous suture using short-thread double-armed micro-suture for cerebral vascular anastomosis. Surg Neurol Int 21-Oct-2014;5:153
How to cite this URL: Haga S, Nagata S. Usefulness of continuous suture using short-thread double-armed micro-suture for cerebral vascular anastomosis. Surg Neurol Int 21-Oct-2014;5:153. Available from: http://surgicalneurologyint.com/surgicalint_articles/usefulness-of-continuous-suture-using-short-thread-double-armed-micro-suture-for-cerebral-vascular-anastomosis/
Abstract
Background:When microvascular anastomosis is performed in a deep, narrow operating field, securing space to throw knots is difficult. To simplify the procedure and avoid obstruction of the anastomosis, we use a continuous suturing with short-thread double-armed micro-suture.
Methods:Sixty-four patients (38 cerebral revasculazation, 16 moyamoya disease, and 10 aneurysm surgery) undergoing microvaucular anastomosis were included. During anastomosis, a continuous suture was placed with short-thread double-armed micro-suture.
Results:During 64 microanastomosis procedures, 64 consecutive continuous sutures were performed with 1-year follow up. All patients showed patency of anastomosis with long-term follow up.
Conclusions:This technique is especially useful for anastomosis in a deep, narrow surgical field, such as in superior cerebellar artery anastomosis.
Keywords: Anastomosis, continuous suture, double-armed micro-suture
INTRODUCTION
During microvascular anastomosis, patency of the anastomosis is critical. However, when anastomosis is performed in a deep, narrow operating field, securing space to throw knots is difficult, even on the more easily accessible side of the vessel in the operating microscope field. To simplify the procedure and avoid obstruction of the anastomosis, we use short-thread double-armed micro-suture to place a running suture.
MATERIALS AND METHODS
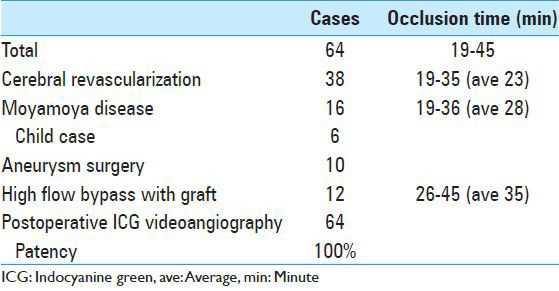
Sixty-four patients (38 cerebral revasculazation, 16 moyamoya disease, and 10 aneurysm surgery) receiving microvascular anastomosis participated in the 5-year study at our institute [
Operative technique
We use 6 cm 10-0 nylon double-armed micro-suture (Bear Medic Corp., Tokyo, Japan) with a needle at both suture ends [
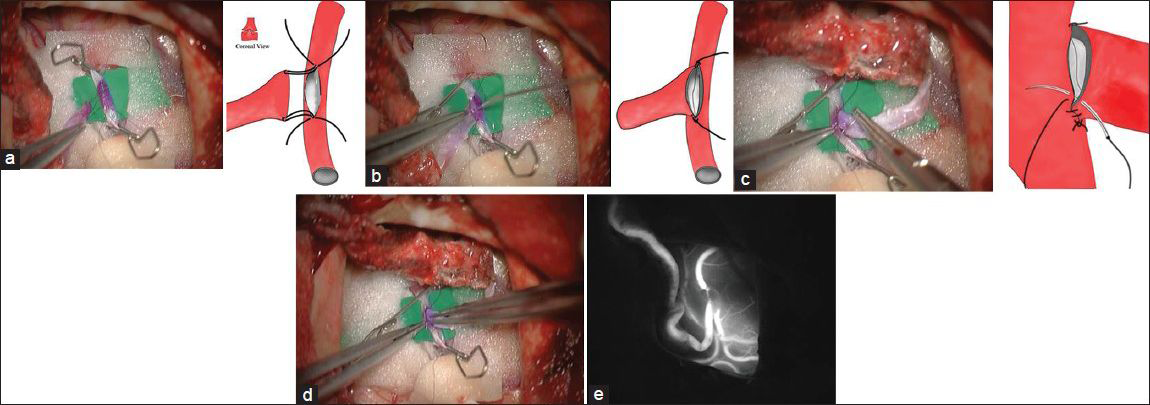
Figure 2
Intraoperative photographs of superficial temporal artery-middle cerebral artery anastomosis and schemas showing microanastomosis with short-thread double-armed microsuture. (a) Microsuture insertion. Out-in for donor artery, In-out for recipient artery. (b) Mattress sutures are placed for anchoring. This technique causes eversion of the vessel ends for attachment of recipient endothelium to the donor artery. (c) Running suture is placed without the “purse string” and puckering effects. (d) Vessel ends are visualized with pyoctanin (crystal violet) for attachment of endothelium. (e) Patency of anastomosis is confirmed by indocyanine green videoangiography
RESULTS
During the 64 anastomosis procedures, 64 consecutive continuous suture using short-thread double-armed microsuture were performed. An average occlusion time of recipient artery was 19-45 min [
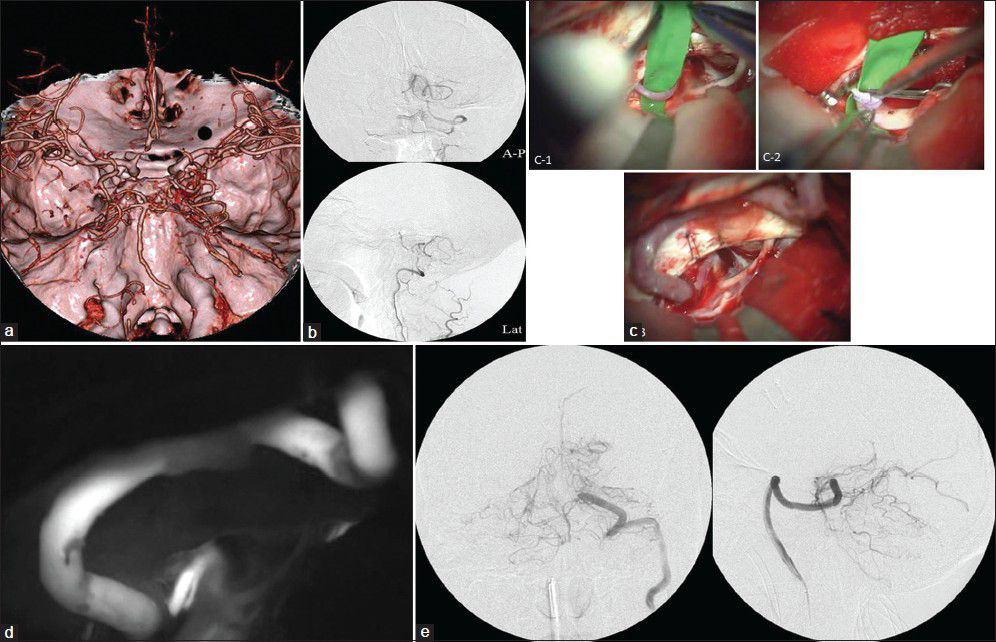
Illustrative case: External carotid artery-superior cerebellar artery bypass with a saphenous vein graft
A 65-year-old male with right vertebral artery and basilar artery occlusion was suffering from progressive hemodynamic vertebra-basilar stroke in spite of medical treatment. To prevent progressive stroke, we treated the patient with external carotid artery-cerebellar artery high-flow bypass with a saphenous vein graft (ECA-SV-superior cerebellar artery [SCA] bypass).
A continuous suture was placed with short-thread double-armed microsuture. An occlusion time of SCA was 38 min. Flow through the SCA and the bypass was confirmed intraoperatively with ICG videoangiography [
Figure 3
Illustrative Case: External carotid artery-superior cerebellar artery bypass with a saphenous vein graft (ECA-SV-SCA bypass). (a) Preoperative three-dimensional computed tomographic angiography. (b) Preoperative angiography of vertebral artery, right. (c) Intraoperative photographs of ECA-SV-SCA bypass. (d) ECA-SV-SCA with indocyanine green videoangiography. (e) Postoperative angiography of vertebral artery, right
DISCUSSION
Since its original description by Yaşargil[
The continuous suture technique is easier to perform, is associated with less anastomotic leakage, and requires less surgical time than other techniques.[
A disadvantage of our procedure is it required many needles. Sometimes, it might be troublesome in a narrow deep surgical field. We think it improves by experience.
The creation of an intracranial micro-anastomosis within a deep and narrow surgical field is extremely technically difficult. Our technique allows for an easier and faster micro-anastomosis with less anastomotic leakage intraoperatively and good postoperative results.
References
1. Abdulrauf SI. Extracranial-to-intracranial bypass using radial artery grafting for complex skull base tumors: Technical note. Skull Base. 2005. 15: 207-13
2. Aihara M, Fujimaki H, Shintoku R, Osawa T, Asakura K, Miyazaki M. Mattress anastomosis in micro vascular reconstruction: Technical note. Acta Neurochir (Wien). 2013. 155: 607-9
3. Gerdisch M, Hinkamp T, Ainsworth SD. Blood flow pattern and anastomotic compliance for interrupted versus continuous coronary bypass grafts. Heart Surg Forum. 2003. 6: 65-71
4. Mura J, Rojas-Zalazar D, de Oliveira E. Revascularization for complex skull base tumors. Skull Base. 2005. 15: 63-70
5. Sekhar LN, Duff JM, Kalavakonda C, Olding M. Cerebral revascularization using radial artery grafts for the treatment of complex intracranial aneurysms: Techniques and outcomes for 17 patients. Neurosurgery. 2001. 49: 646-58
6. Spetzler RF, Fukushima T, Martin N, Zabramski JM. Petrous carotid-to-intradural carotid saphenous vein graft for intracavernous giant aneurysm, tumor, and occlusive cerebrovascular disease. J Neurosurg. 1990. 73: 496-501
7. Wanebo JE, Zabramski JM, Spetzler RF. Superficial temporal artery-to-middle cerebral artery bypass grafting for cerebral revascularization. Neurosurgery. 2004. 55: 395-9
8. Yaşargil MG.editors. Anastomosis between the superficial temporal artery and a branch of the middle cerebral artery: Microsurgery Applied to Neurosurgery. Stuttgart: George Thieme Verlag; 1969. p. 105-15