- Department of Neurosurgery, Ehime University School of Medicine, Toon, Japan
- Department of Neurosurgery, HITO Hospital, Shikokuchuo, Japan.
Correspondence Address:
Akihiro Inoue, Department of Neurosurgery, Ehime University School of Medicine, Toon, Japan.
DOI:10.25259/SNI_120_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seiji Shigekawa1, Seishi Matsui1, Akihiro Inoue1, Naoki Shinohara2, Takeharu Kunieda1. Usefulness of cyst-subarachnoid shunt using syringo-subarachnoid shunt tube for symptomatic enlarging ventriculus terminalis: A case report and review of the literature. 05-May-2023;14:165
How to cite this URL: Seiji Shigekawa1, Seishi Matsui1, Akihiro Inoue1, Naoki Shinohara2, Takeharu Kunieda1. Usefulness of cyst-subarachnoid shunt using syringo-subarachnoid shunt tube for symptomatic enlarging ventriculus terminalis: A case report and review of the literature. 05-May-2023;14:165. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12310
Abstract
Background: The ventriculus terminalis (VT) is a cystic embryological remnant of the conus medullaris that usually regresses after birth. This structure rarely persists into adulthood and may produce neurological symptoms. We recently encountered three cases of symptomatic enlarging VT.
Case Description: The three female patients were 78, 64, and 67 years old. Symptoms included pain, numbness, motor weakness, and frequent urination that gradually worsened. Magnetic resonance imaging revealed cystic dilatations of slow growing VT. These patients showed marked improvement after cyst-subarachnoid shunt using a syringo-subarachnoid shunt tube.
Conclusion: Symptomatic enlarging VT is an extremely rare cause of conus medullaris syndrome and the optimal treatment strategy remains unclear. Surgical management may thus be appropriate for patients with symptomatic enlarging VT.
Keywords: Cyst-subarachnoid shunt, Enlarging ventriculus terminalis, Slow growing, Symptomatic case, Syringosubarachnoid shunt tube
INTRODUCTION
The ventriculus terminalis (VT), also known as the fifth ventricle, is a small ependymal-lined fusiform dilatation of the terminal central canal of the spinal cord, located at the transition from the tip of the conus medullaris to the origin of the filum terminale.[
CASE DESCRIPTION
The clinical study of the following cases was approved by the Ethics Committee for Clinical Research at Ehime University Hospital, and informed consent was obtained from the patients before initiating the study.
Case 1
A 78-year-old woman with no contributory history of illness or medical treatment was admitted to our hospital with low back pain radiating to both limbs, numbness in both soles, intermittent claudication, and frequent urination. No paralysis was apparent in either lower limb. Evaluation of the superficial and deep tendon reflexes did not demonstrate any abnormality. She had been asymptomatic until 12 years earlier. Magnetic resonance imaging (MRI) revealed the presence of a cystic lesion located in the conus medullaris, with a well-defined outline and no enhancement on gadolinium-enhanced T1-weighted imaging, confirming cystic dilation of the VT as so-called enlarging VT. The size of this cyst appeared to have increased over the 12 years [
Figure 1:
Results of magnetic resonance imaging (MRI). (a) T2-weighted sagittal image from 12 years before this presentation shows cystic dilatation of the conus medullaris. (b-1) T1-weighted image. (b-2) T1-weighted image with gadolinium enhancement. (b-3) T2-weighted image. (c) Postoperative T2-weighted images obtained 3 years after surgical treatment reveal regression of the dilatation without evidence of relapse (white bold arrow).
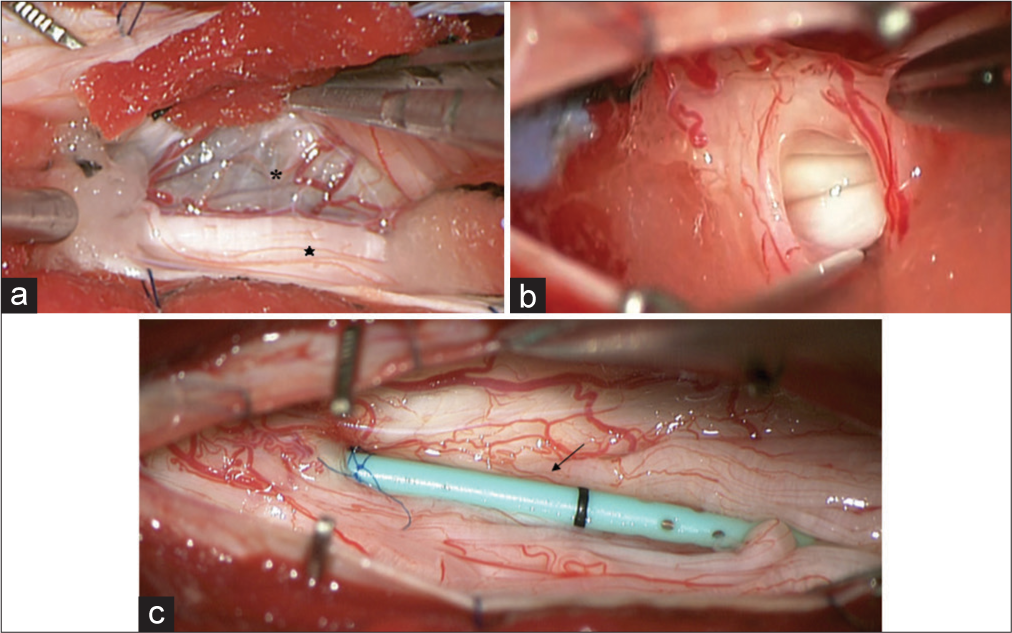
Figure 2:
Cystic dilation of the ventriculus terminalis from an intraoperative view. (a and b) On opening the dura, the expanded conus began herniating outward under pressure, which was relieved by fenestration. (c) Cystsubarachnoid shunt was created using a syringo-subarachnoid shunt tube (diameter: 1.2 mm, length: 40 mm). Black asterisk: Cyst wall, black star: Cauda equina, black arrow: Syringo-subarachnoid shunt tube.
Case 2
A 62-year-old woman with no contributory medical or surgical history presented with the right thigh pain that had gradually worsened over 3 years. No paralysis was apparent in either lower limb. MRI on admission demonstrated a cystic lesion in the conus medullaris spanning from the 12th thoracic to first lumbar level [
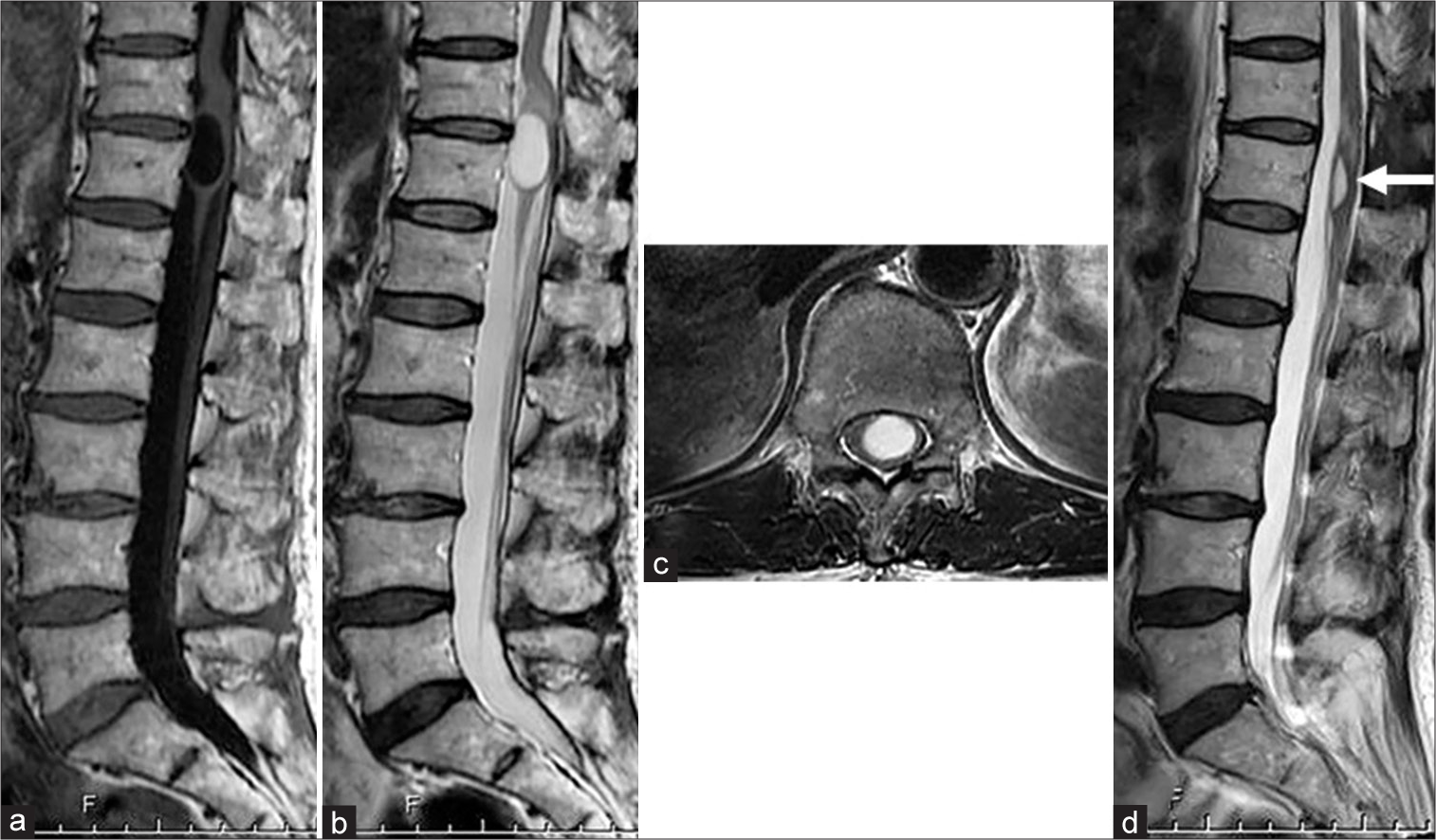
Figure 3:
Preoperative sagittal and axial spinal magnetic resonance imaging demonstrating a cystic lesion near the conus medullaris. (a) Sagittal T1-weighted image with non-contrast sequence. (b) Sagittal T2-weighted image. (c) Axial T2-weighted image. (d) Postoperative sagittal T2-weighted image 2 years after surgery reveals complete regression of the dilation (white bold arrow).
Case 3
A 67-year-old woman with no contributory surgical or medical history presented with numbness in both lower limbs and weakness in the left lower limb. MRI on admission showed findings similar to those in Cases 1 and 2 [
Figure 4:
Sagittal and axial magnetic resonance imaging on admission demonstrating a cystic lesion near the conus medullaris. (a) Sagittal T1-weighted image with non-contrast sequence. (b) Sagittal T2-weighted image. (c) Axial T2-weighted image. (d) Postoperative sagittal T2-weighted image 1 year after surgery shows complete regression of the dilation (white bold arrow).
DISCUSSION
The VT is an ependymal-lined cavity in the conus medullaris that is anatomically continuous with the central canal of the spinal cord. This structure usually forms during embryogenesis and subsequently disappears during the regressive differentiation period.[
Optimal treatment for asymptomatic patients seems to be conservative, but the best treatment strategy for symptomatic enlarging VT has yet to be clarified.[
Several limitations to our report must be kept in mind. At present, symptomatic enlarging VT is a rare neurological condition, and few cases have been reported. Further research, accumulation of more cases, and longer follow-up of patients are required to obtain a better understanding of the pathological conditions and appropriate therapies associated with this entity.
CONCLUSION
We have reported three cases of symptomatic enlarging VT treated with cyst-subarachnoid shunt using a syringosubarachnoid shunt tube. Symptomatic enlarging VT is an extremely rare cause of conus medullaris syndrome and the optimal treatment strategy remains unclear. Our successful surgical management of these three cases by cysticsubarachnoid shunting using a syringo-subarachnoid shunt tube for drainage of the enlarging VT provides a potential option for treating symptomatic enlarging VT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Coleman LT, Zimmerman RA, Rorke LB. Ventriculus terminalis of the conus medullaris: MR findings in children. AJNR Am J Neuroradiol. 1995. 16: 1421-6
2. Ganau M, Talacchi A, Cecchi P, Ghimenton C, Gerosa M, Faccioli F. Cystic dilation of the ventriculus terminalis. J Neurosurg Spine. 2012. 17: 86-92
3. Kawanishi M, Tanaka H, Yokoyama K, Yamada M. Cystic dilation of the ventriculus terminalis. J Neurosci Rural Pract. 2016. 7: 581-3
4. Lotfinia I, Mahdkhah A. The cystic dilation of ventriculus terminalis with neurological symptoms: Three case reports and a literature review. J Spinal Cord Med. 2018. 41: 741-7
5. Nassar SI, Correll JW, Housepian EM. Intramedullary cystic lesions of the conus medullaris. J Neurol Neurosurg Psychiatry. 1968. 31: 106-9
6. Pencovich N, Bensira L, Constantini S. Massive cystic dilatation within a tethered filum terminale causing cauda equina compression and mimicking syringomyelia in a young adult patient. Childs Nerv Syst. 2013. 29: 141-4
7. Sigal R, Denys A, Halimi P, Shapeero L, Doyon D, Boudghène F. Ventriculus terminalis of the conus medullaris: MR imaging in four patients with congenital dilatation. Am J Neuroradiol. 1991. 12: 733-7
8. Suh SH, Chung TS, Lee SK, Cho YE, Kim KS. Ventriculus terminalis in adults: Unusual magnetic resonance imaging features and review of the literature. Korean J Radiol. 2012. 13: 557-63
9. Van Rillaer O, Vandaele P, Ramboer K. Malformative persistence of terminal ventricle. JBR BTR. 2009. 92: 178-9
10. Weisbrod LJ, Liu C, Surdell D. Enlarging ventriculus terminalis in a patient with polyarteritis nodosa. Cureus. 2021. 13: e14460
11. Zhang L, Zhang Z, Yang W, Jia W, Xu Y, Yang J. Cystic dilation of the ventriculus terminalis (CDVT): Report of six surgical cases treated with cyst-subarachnoid shunting using T-catheter. World Neurosurg. 2017. 104: 522-7