- Department of Neurosurgery, Osaka University Graduate School of Medicine, Osaka, Japan.
Correspondence Address:
Manabu Kinoshita, Department of Neurosurgery, Osaka University Graduate School of Medicine, Osaka, Asahikawa Medical University, Midorigaoka-higashi 2-1-1-1, Asahikawa, Hokkaido 078-8510 Japan.
DOI:10.25259/SNI_320_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Noriyuki Kijima, Manabu Kinoshita, Masatoshi Takagaki, Haruhiko Kishima. Utility of a novel exoscope, ORBEYE, in gravity-assisted brain retraction surgery for midline lesions of the brain. 06-Jul-2021;12:339
How to cite this URL: Noriyuki Kijima, Manabu Kinoshita, Masatoshi Takagaki, Haruhiko Kishima. Utility of a novel exoscope, ORBEYE, in gravity-assisted brain retraction surgery for midline lesions of the brain. 06-Jul-2021;12:339. Available from: https://surgicalneurologyint.com/surgicalint-articles/10939/
Abstract
Background: Midline brain lesions, such as falx meningioma, arteriovenous malformations, and cavernous malformations, are usually approached from the ipsilateral interhemispheric fissure. To this end, patients are positioned laterally with the ipsilateral side up. However, some studies have reported the usefulness of gravity-assisted brain retraction surgery, in which patients are placed laterally with the ipsilateral side down or up, enabling surgeons to approach the lesions through the ipsilateral side or through a contralateral interhemispheric fissure, respectively. This surgery requires less brain retraction. However, when using an operative microscope, performing this surgery requires the surgeon to operate in an awkward position. A recently developed high-definition (4K-HD) 3-D exoscope system, ORBEYE, can improve the surgeon’s posture while performing gravity-assisted brain retraction surgery.
Methods: We report five cases with midline brain tumors managed by resectioning with gravity-assisted brain retraction surgery using ORBEYE. We also performed an ergonomic analysis of gravity-assisted brain retraction surgery with a craniotomy model and a neuronavigation system.
Results: Gravity-assisted brain retraction surgery to the midline brain tumors was successfully performed for all five patients, using ORBEYE, without any postoperative neurological deficit.
Conclusion: Gravity-assisted brain retraction surgery to the midline brain lesions using ORBEYE is feasible, and ORBEYE is ergonomically more favorable than a microscope. ORBEYE has the potential to generalize neurosurgical approaches considered difficult due to the surgeon’s awkward position, such as gravity-assisted brain retraction surgery.
Keywords: Exoscope, Gravity-assisted brain retraction surgery, Neurosurgery, Operating microscope, Tumor
INTRODUCTION
Midline brain lesions, such as falx meningioma, arteriovenous malformations, and cavernous malformations, are usually approached from the ipsilateral interhemispheric fissure, and patients are positioned laterally with the ipsilateral side up. However, some studies have reported the usefulness of gravity-assisted brain retraction surgery. Thereby, patients are placed laterally with their ipsilateral side down and the lesions are approached through the ipsilateral side; alternatively, patients are positioned laterally with their ipsilateral side up and the lesions are approached through a contralateral interhemispheric fissure (contralateral transfalcine approach).[
Conversely, with gravity-assisted brain retraction surgery, less intraoperative brain retraction is required because gravity naturally retracts the brain. In this sense, gravity-assisted brain retraction surgery is also advantageous. However, this surgery is more difficult when using an operative microscope because the angle of the microscope limits the operative field; the surgeon is required to operate from awkward angles, and patients’ heads need to be fixed at a 40° vertex up position to achieve an optimal angle. Further, the location of the tumor, relative to the brain surface, is quite deep.
Although the operative microscope has remarkably advanced neurosurgical treatment, a recently developed exoscope system can improve neurosurgical approaches and the position of the patient and the surgeon during the surgery. The widespread use of exoscopes in neurosurgery was previously limited by the lack of stereopsis with two-dimensional (2-D) monitors. However, the features of a recently developed exoscope system, ORBEYE (Olympus, Tokyo, Japan), are different from those of traditional exoscopes and operative microscopes. ORBEYE combines the characteristics of an operative microscope and an endoscope. It has a high-definition (4K-HD) 3-D exoscope system, which allows the visualization of critical structures and provides portable and high-definition operative experience.
This study sought to investigate the feasibility of performing gravity-assisted brain retraction surgery of midline brain lesions with the recently introduced exoscope system, ORBEYE.
MATERIALS AND METHODS
Patient characteristics
We performed a gravity-assisted brain retraction surgery to midline brain tumors in five cases after the exoscope, ORBEYE, was introduced at our institution in April 2019. Gravity-assisted brain retraction surgery from the ipsilateral side of the tumor was performed in two patients, and a contralateral transfalcine approach was conducted in three patients. Perioperative clinical, surgical, and radiographic data were retrospectively acquired. We also reviewed the presenting symptoms, histopathology, and perioperative performance status. This analysis and informed consent were approved by the Institutional Review Board, and all the patients gave informed consent.
Gravity-assisted brain retraction surgery procedure
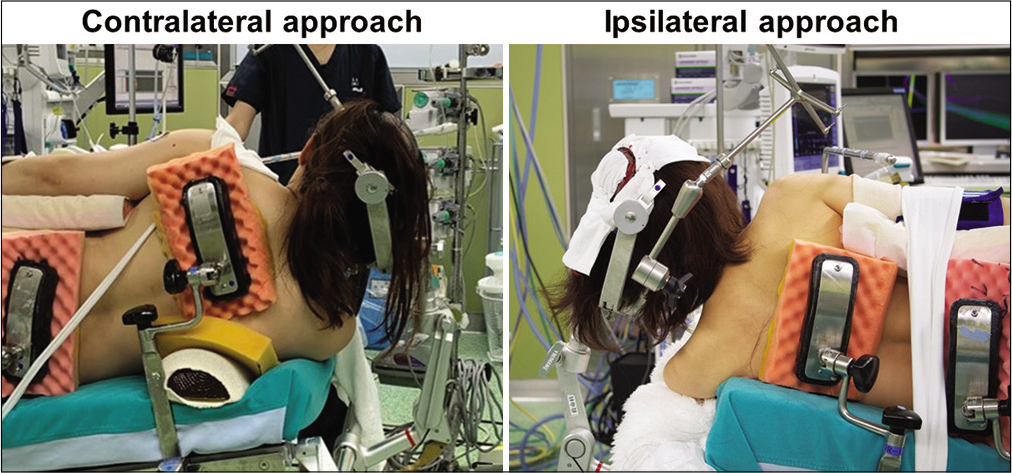
Gravity-assisted brain retraction surgery includes both an ipsilateral and a contralateral approach to the lesions. An ipsilateral approach is indicated when the tumor is located almost midline and is not extended laterally. A contralateral transfalcine approach is indicated when the tumor is extended laterally and/or cerebral edema is present on the ipsilateral tumor side. For the ipsilateral approach, the patients are placed in a lateral position with the tumor side facing downward at 40° vertex up. For the contralateral transfalcine approach, the patients are placed in a lateral position with the tumor side facing upward at 40° vertex up position [
Figure 1:
Patient’s position for gravity-assisted brain retraction surgery. For the ipsilateral approach, the patients are placed in a lateral position with the tumor side facing downward at 40° vertex up. For the contralateral transfalcine approach, the patients are placed in a lateral position with the tumor side facing upward at 40° vertex up position.
We performed a hemicraniotomy on the approach side. Next, we dissected the interhemispheric fissure and visualized the tumor. We coagulated and resected the tumor with gravity-assisted brain retraction.
Ergonomic analysis using craniotomy models and a neuronavigation system
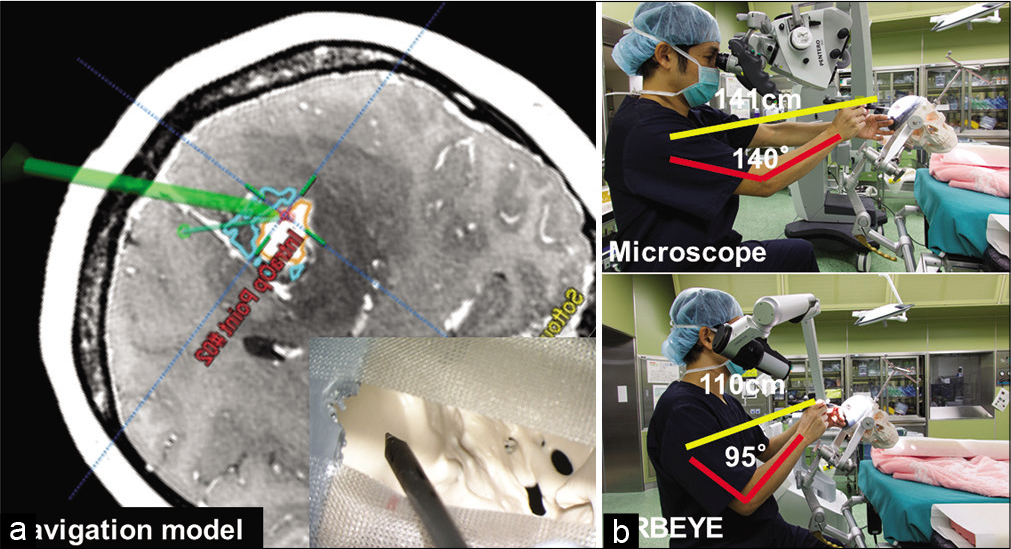
We investigated the ergonomics of gravity-assisted brain retraction surgery of midline brain lesions with craniotomy models. We sought to simulate the contralateral transfalcine approach in a human skull craniotomy model, fabricated with the Form2 3-D printer (Formlabs, MA, USA). We pinned down the skull with a Mayfield skull clamp (Integra LifeSciences Corporation, Ohio, USA) at a 40° vertex up position to achieve an optimal angle for the contralateral transfalcine approach. We entered data from the MRI scan of “patient 1” into the BRAIN LAB Curve-Navigation system (Brainlab Corp., Feldkirchen, Germany). We registered the tumor’s lateral part as the target lesion [
Figure 2:
ORBEYE allows more natural physician positioning. (a) Image from the neuronavigation system of preoperative MRI scan from Patient 1. We set the target in the superolateral part of the tumor. Navigation pointer showing the same target with the microscope and exoscope (ORBEYE). (b) Ergonomic differences between microscope and exoscope use (ORBEYE).
RESULTS
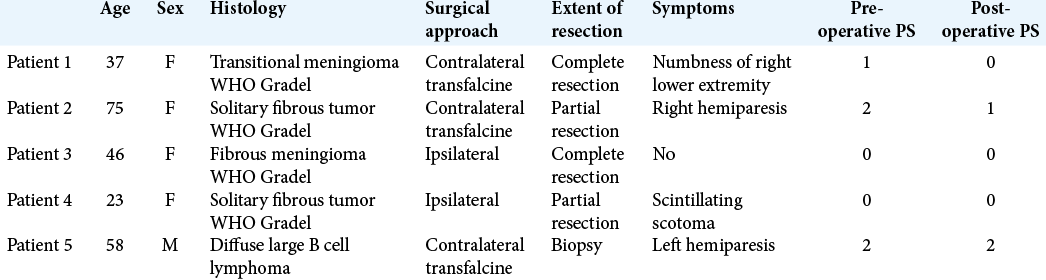
Demographic characteristics of the five patients who underwent gravity-assisted brain retraction surgery.
The demographic characteristics of the five patients are presented in [
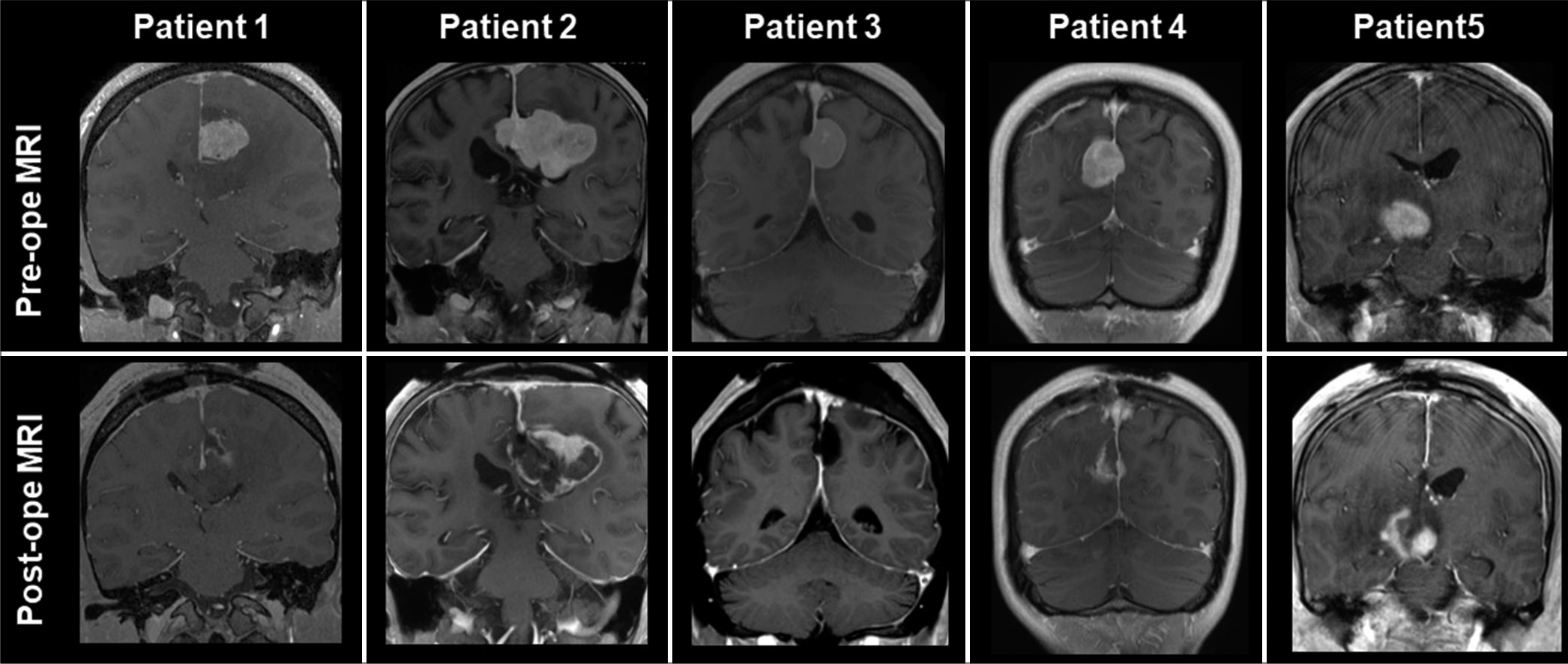
Figure 3:
Preoperative and postoperative MRI scans from each patient. Patient 1 had a tumor with a maximum diameter of 26 mm with peritumoral edema present. A complete resection was made possible using a contralateral transfalcine approach. Patient 2 had a tumor with a maximum diameter of 54 mm with peritumoral edema. Partial resection was carried out using a contralateral transfalcine approach. Patient 3 had a tumor with a maximum diameter of 25 mm with peritumoral edema present. A complete resection was made possible using an ipsilateral approach. Patient 4 had a tumor with a maximum diameter of 25 mm. Partial resection was carried out using an ipsilateral approach. Patient 5 had a tumor with a maximum diameter of 30 mm. Partial resection was carried out using a contralateral approach.
Cases
Patient 1
A 37-year-old woman presented with headache and slight numbness of the upper extremity for 1 month when she visited our outpatient clinic. The MRI scan revealed falx meningioma with peripheral edema at the medial frontal lobe. The maximum tumor diameter was 26 mm. Most of the t4mor was located on the left side of the falx. An ipsilateral approach to the tumor could have damaged the brain during retraction due to significant peripheral edema at the medial frontal lobe. Thus, we decided that a contralateral approach to the tumor was relatively safer. We chose to perform the contralateral transfalcine approach to the tumor using the ORBEYE exoscope. The patient was placed in a lateral position with the tumor side upward. The patient’s head was pinned down with an upward tilt of 40°. We performed right hemicraniotomy, dissected the interhemispheric fissure, and visualized the falx [
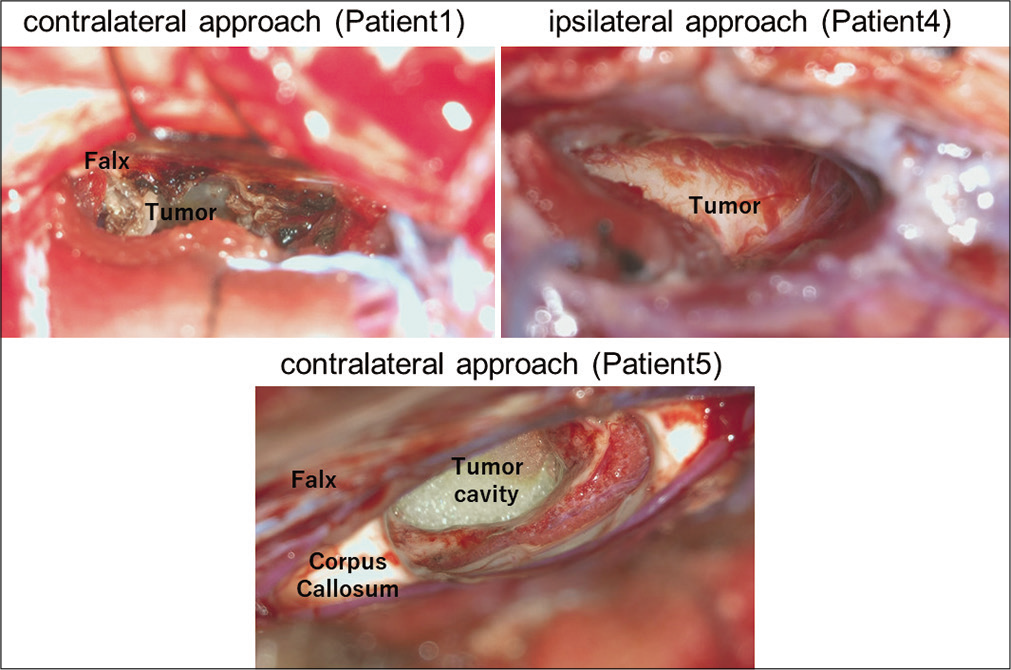
Figure 4:
Intraoperative images from representative cases. Patient 1 underwent tumor resection using contralateral transfalcine approach. Falx and contralateral tumor were easily visualized by ORBEYE with high definition. Patient 4 underwent tumor resection using ipsilateral approach. Falx and tumor were easily visualized by ORBEYE with high definition. Patient 5 underwent tumor resection using contralateral approach. Falx, corpus callosum, and tumor cavity were easily visualized by ORBEYE with high definition.
Patient 2
A 75-year-old woman presented with slight numbness of the right upper and lower extremity. The MRI scan revealed a falx meningioma with peripheral edema in the medial frontal lobe. The maximum tumor diameter was 54 mm. Most of the tumor was located on the left side of the falx. Similar to patient 1, we opted to perform the contralateral transfalcine approach. We performed a bilateral craniotomy crossing the superior sagittal sinus with the right side dominant in case we use the left side interhemispheric fissure. We performed tumor resection; however, the left side tumor, which was located superiorly, could not be visualized. Thus, partial resection was performed. A histopathological diagnosis of a WHO Grade II solitary fibrous tumor was made. The postoperative course was uneventful and the patient’s numbness gradually improved; the postoperative MRI revealed residual lesions [
Patient 3
A 46-year-old woman was asymptomatic when she visited our outpatient clinic. The MRI scan revealed a falx meningioma in the medial parietal lobe. The maximum tumor diameter was 25 mm. We initially decided to keep the patient on observation; however, the follow-up MRI revealed tumor growth. Informed consent was obtained from the patient, and we chose to perform tumor resection. We opted for the ipsilateral approach to the tumor because the tumor mostly was located at the midline and did not extend laterally. The patient was placed in a lateral position with the tumor side downward. The patient’s head was pinned down with an upward tilt of 40°. We performed a left hemicraniotomy, dissected the interhemispheric fissure, and visualized the tumor. We resected the tumor completely; a histopathological diagnosis of a WHO Grade I fibrous meningioma was formulated. The postoperative course was uneventful, and the postoperative MRI revealed no residual tumor [
Patient 4
A 23-year-old woman presented with a scintillating scotoma for 2 months when she visited our outpatient clinic. The MRI scan revealed a falx meningioma in the medial parietal lobe. The maximum tumor diameter was 25 mm. We initially decided to keep the patient on observation; however, the follow-up MRI revealed tumor growth. Informed consent was obtained from the patient and we opted for tumor resection. We chose to perform the ipsilateral approach to the tumor because the tumor was mostly located at the midline and did not extend laterally. The patient was placed in a lateral position with the tumor side downward. The patient’s head was pinned down with an upward tilt of 40°. We performed a right hemicraniotomy, dissected the interhemispheric fissure, and visualized the tumor [
Patient 5
A 58-year-old man presented with the left hemiparesis when he visited our outpatient clinic. The MRI scan revealed a brain tumor in the right thalamus. The maximum tumor diameter was 30 mm. An ipsilateral approach to the tumor could have damaged the brain during retraction; thus, we opted for the contralateral transfalcine approach to the tumor using the ORBEYE exoscope. The patient was placed in a lateral position with the tumor side upward. The patient’s head was pinned down with an upward tilt of 40°. We performed a left hemicraniotomy, dissected the interhemispheric fissure, and visualized the corpus callosum. We dissected the corpus callosum and approached the right lateral ventricle. We visualized the right thalamus and approached the tumor, and performed a partial resection [
Ergonomic analysis during contralateral transfalcine approach by craniotomy model.
We assessed the ergonomic difference in performing the contralateral transfalcine approach with the microscope and the exoscope. In so doing, we sought to simulate the contralateral transfalcine approach in a human skull craniotomy model. As shown in
DISCUSSION
In this study, we reported five cases in which the gravity-assisted brain retraction surgery was successfully performed using the ORBEYE exoscope. The previous studies reported the usefulness of the gravity-assisted brain retraction surgery from either the ipsilateral or the contralateral transfalcine approach for midline brain lesions, such as arteriovenous malformation,[
The operating microscope has remained the gold standard in microneurosurgery since its introduction in this field in the 1960s.[
Previous reports demonstrated the feasibility of the ORBEYE exoscope system compared with that of the operative microscope.[
We had also performed an ergonomic analysis for the contralateral transfalcine approach using a craniotomy model and a neuronavigation system. In this analysis, when we approached the same target within the tumor, the use of ORBEYE was found to be more ergonomically favorable than the microscope because the surgeons could sit in a neutral position during the procedure and were not required to spread their arms while operating. In addition, the working distance from the skull and surgeon is much shorter when we used ORBEYE. Using a chair with armrests while preforming surgery under the microscope is another way to augment surgical stance; however, the shortcoming of a chair with armrests is that it requires more space. When using ORBEYE, the surgeons do not need armrests during the operation.
Thus, the use of ORBEYE has the potential to simplify neurosurgical approaches that were previously considered difficult because of the surgeon’s position, such as in the context of a gravity-assisted brain retraction surgery for midline brain tumors.
CONCLUSION
Gravity-assisted brain retraction surgeries to midline brain lesions using an exoscope are feasible. Exoscopic surgery maintains the same safety profile as that using the operative microscope and is ergonomically favorable for surgeons. Thus, it could be a gold standard for neurosurgical procedures, such as in the context of gravity-assisted brain retraction surgeries.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ahmad FI, Mercicli AF, DeFazio MV, Chang EI, Hanasono MM, Pederson WC. Application of the ORBEYE three-dimensional exoscope for microsurgical procedures. Microsurgery. 2020. 40: 468-72
2. García-García S, Gonzalez-Sanchez J, Gandhi S, Tabani H, Meybodi AT, Kakaizada S. Contralateral transfalcine versus ipsilateral anterior interhemispheric approach for midline arteriovenous malformations: Surgical and anatomical assessment. World Neurosurg. 2018. 119: e1041-51
3. Graffeo CS, Perry A, Rangel-Castilla L. Interhemispheric transfalcine approach to a medial frontal arteriovenous malformation: Operative video with positioning illustrations. Heliyon. 2019. 5: e02041
4. Hafez A, Raygor KP, Lawton MT. Contralateral anterior interhemispheric approach to medial frontal arteriovenous malformations: Surgical technique and results. Oper Neurosurg (Hagerstown). 2017. 13: 413-20
5. Hendricks BK, Spetzler RF. Contralateral interhemispheric approach for resection of a meningioma: 2-Dimensional operative video. Oper Neurosurg (Hagerstown). 2020. 18: E159
6. Isumo T, Ujifuku K, Baba S, Morofuji Y, Horie N, Matsuo T. Initial experience of ORBEYE™ surgical microscope for carotid endarterectomy. Asian J Neurosurg. 2019. 14: 839-42
7. La Rocca G, Sabatina G, Altieri R, Mazzucchi E, Rapisarda A, Ius T. Parietal interhemispheric transfalcine transtentorial approach for posterior incisural space lesions: From the lab to the operative room. Neurosurg Rev. 2020. 44: 1779-88
8. Mooney MA, Sanai N. Contralateral interhemispheric, transfalcine approach with asleep motor mapping for parasagittal lesions near the medial precentral gyrus. Neurosurg Focus. 2018. 45: V6
9. Sack J, Steinberg JA, Rennert RC, Hatefi D, Pannell JS, Levy M. Initial experience using a high-definition 3-dimensional exoscope system for microneurosurgery. Oper Neurosurg (Hagerstown). 2018. 14: 395-401
10. Smith S, Kozin ED, Kanumur VV, Barber SR, Backous D, Flávio Nogueira J. Initial experience with 3-dimensional exoscope-assisted transmastoid and lateral skull base surgery. Otolaryngol Head Neck Surg. 2019. 160: 364-7
11. Takahashi S, Toda M, Nishimoto M, Ishihara E, Miwa T, Akiyama T. Pros and cons of using ORBEYE™ for microneurosurgery. Clin Neurol Neurosurg. 2018. 174: 57-62
12. Yaşargil MG. A legacy of microneurosurgery: Memoirs, lessons, and axioms. Neurosurgery. 1999. 45: 1025-92
13. Yu G, Wang X, Zhang X, Quan K, Hua W, Yang Z. Gravity-assisted ipsilateral paramedian approach for parafalcine meningioma resection. World Neurosurg. 2020. 135: 234-40
14. Zaidi HA, Chowdhry SA, Nakaji P, Abia AA, Spetzler RF. Contralateral interhemispheric approach to deep-seated cavernous malformations: Surgical considerations and clinical outcomes in 31 consecutive cases. Neurosurgery. 2014. 71: 80-6