- Department of Neurosurgery, Ehime University School of Medicine, Toon, Ehime, Japan.
Correspondence Address:
Akihiro Inoue, Department of Neurosurgery, Ehime University School of Medicine, Toon, Ehime, Japan.
DOI:10.25259/SNI_503_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masahiko Tagawa, Akihiro Inoue, Kentaro Murayama, Shirabe Matsumoto, Saya Ozaki, Masahiro Nishikawa, Seiji Shigekawa, Hideaki Watanabe, Takeharu Kunieda. Utility of targeted balloon protection of the venous sinus for endovascular treatment of dural arteriovenous fistula by transarterial embolization with Onyx: A case report and literature review. 12-Jul-2021;12:340
How to cite this URL: Masahiko Tagawa, Akihiro Inoue, Kentaro Murayama, Shirabe Matsumoto, Saya Ozaki, Masahiro Nishikawa, Seiji Shigekawa, Hideaki Watanabe, Takeharu Kunieda. Utility of targeted balloon protection of the venous sinus for endovascular treatment of dural arteriovenous fistula by transarterial embolization with Onyx: A case report and literature review. 12-Jul-2021;12:340. Available from: https://surgicalneurologyint.com/surgicalint-articles/10968/
Abstract
Background: Onyx has already been reported as an effective and safe agent in transarterial embolization of cranial dural arteriovenous fistula (d-AVF). However, successful treatment is related to not only complete shunt obliteration but also preservation of a normal route of venous drainage. Here, we present a case of transverse sigmoid d-AVF in which successful treatment was achieved by transarterial Onyx embolization with targeted balloon protection of the venous drainage.
Case Description: A 70-year-old man presented with a 3-month history of tinnitus in the left ear and mild headache. Magnetic resonance imaging (MRI) showed a cluster of abnormal blood vessels in the area of the left transverse sinus (TS)-sigmoid sinus (SS) junction. Cerebral angiography demonstrated a Cognard type IIa d-AVF at the left TS-SS junction, supplied mainly by vessels such as the left middle meningeal artery, left occipital artery, and left meningohypophyseal trunk. In the venous phase, the ipsilateral TS-SS was recognized as a functional sinus and the left vein of Labbe drained into the TS near the drainage channel. Based on these findings, we decided to perform endovascular treatment under a transarterial approach with Onyx using targeted balloon protection of the venous sinus to protect against Onyx migration and preserve antegrade sinus flow. The patient recovered well without sequelae, and follow-up MRI 12 months later showed complete disappearance of the d-AVF.
Conclusion: This treatment strategy using targeted balloon protection may be very useful to preserve antegrade sinus flow in patients with Cognard type IIa d-AVF.
Keywords: Dural arteriovenous fistula, Onyx, Targeted balloon protection of the venous sinus, Transarterial embolization
INTRODUCTION
Intracranial dural arteriovenous fistula (d-AVF) represents 10–15% of all intracranial vascular malformations.[
CASE DESCRIPTION
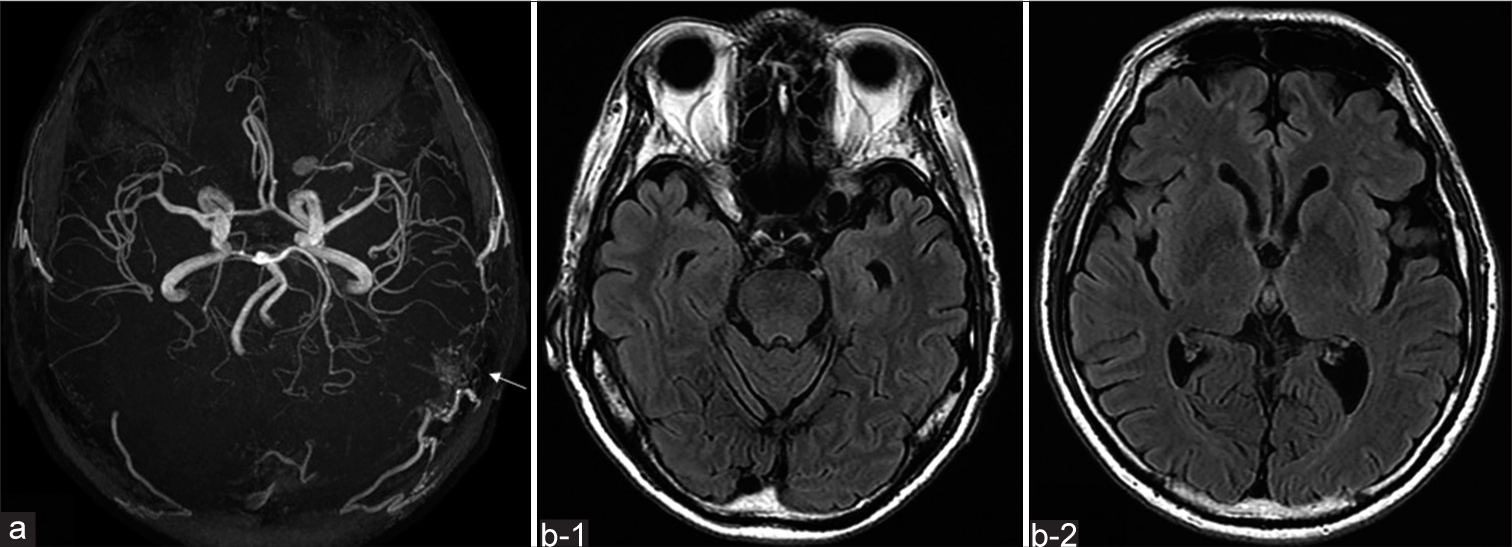
A 70-year-old man with a history of slight hypertension presented with a 3-month history of tinnitus in the left ear and mild headache. Consciousness was clear and no neurological deficits were evident. Magnetic resonance angiography (MRA) on admission showed a cluster of abnormal blood vessels in the area of the left TS-SS junction [
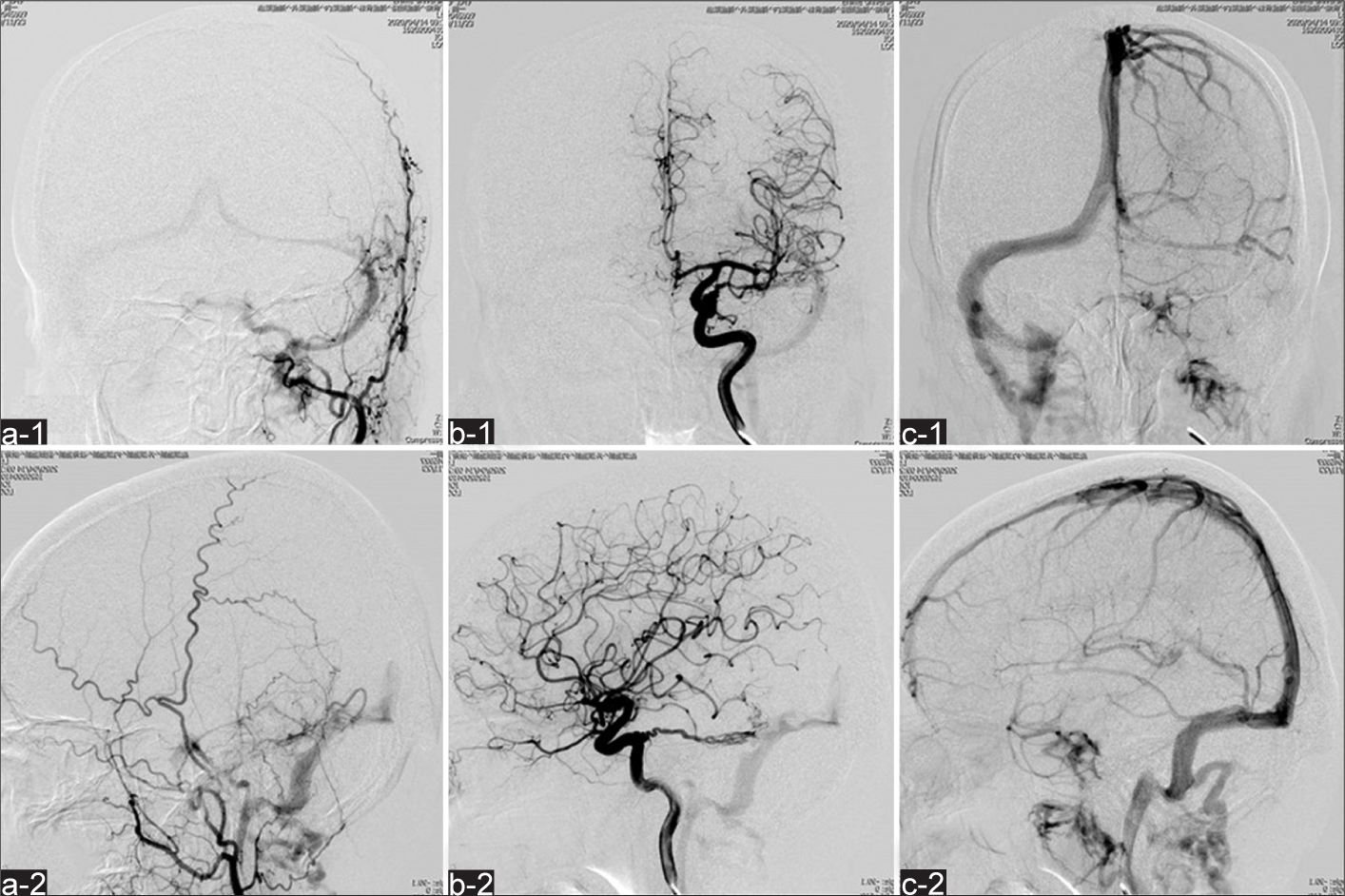
Figure 2:
Preoperative cerebral angiography. (a) Left external carotid angiography (a-1: anterior posterior view, a-2: lateral view) showing shunt flow to the junction of TS-SS via the left middle meningeal artery and left occipital artery. (b) Left internal carotid angiography (b-1: anterior posterior view; b-2: lateral view) revealing fistula to the same area through the left meningohypophyseal trunk in the early phase. In the late venous phase (c-1: anterior posterior view; c-2: lateral view), the draining venous flows mainly into the right TS, but the left SS is partially used for normal venous perfusion. Retrograde flow in the ectatic cortical vein is not recognized. TS: Transverse sinus, SS: Sigmoid sinus.
Figure 3:
Preoperative cerebral angiography. (a) Left vertebral artery angiography (a-1: anterior posterior view; a-2: lateral view) showing the shunt flow to the same portion through left posterior meningeal artery and the meningeal branch of the left superior cerebellar artery in the early arterial phase. In the late venous phase (b-1: anterior posterior view; b-2: lateral view), venous flow drains mainly into the right TS, but the left SS is partially used for normal venous perfusion. Retrograde flow is not apparent in the ectatic cortical vein. TS: Transverse sinus, SS: Sigmoid sinus.
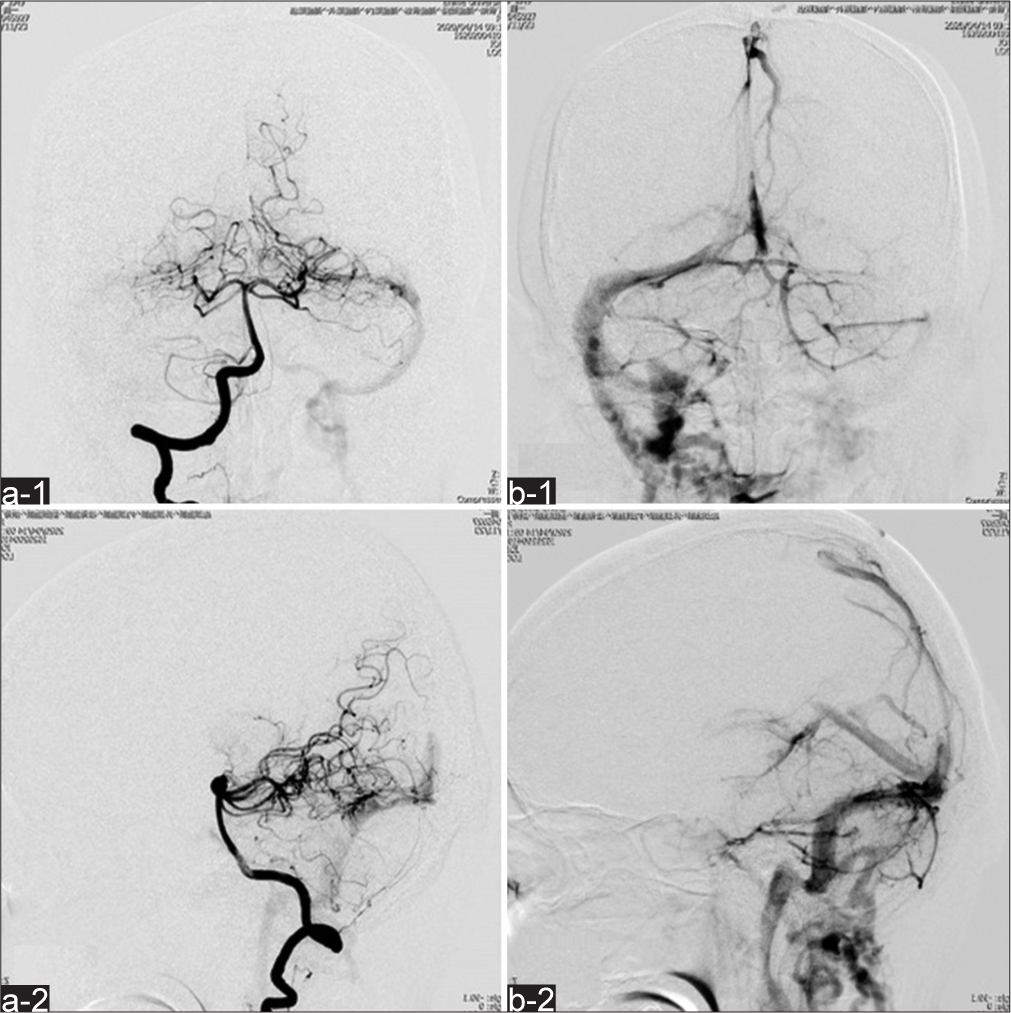
Figure 4:
Endovascular surgery by transarterial embolization. (a and b) Cerebral angiography shows a Headway DUO microcatheter navigated to the near shunt point at the junction of the TS and SS (white arrow: Headway DUO; black dashed arrow: 4.2-Fr FUBUKI). (c) SHOURYU is placed and inflated in the left TSSS junction near the shunt point. (d) Embolization using Onyx 18 is performed while preventing embolic material from straying into the TS-SS (d-1, d-2: Digital subtraction angiography; d-3: Conventional angiography). TS: Transverse sinus, SS: Sigmoid sinus.
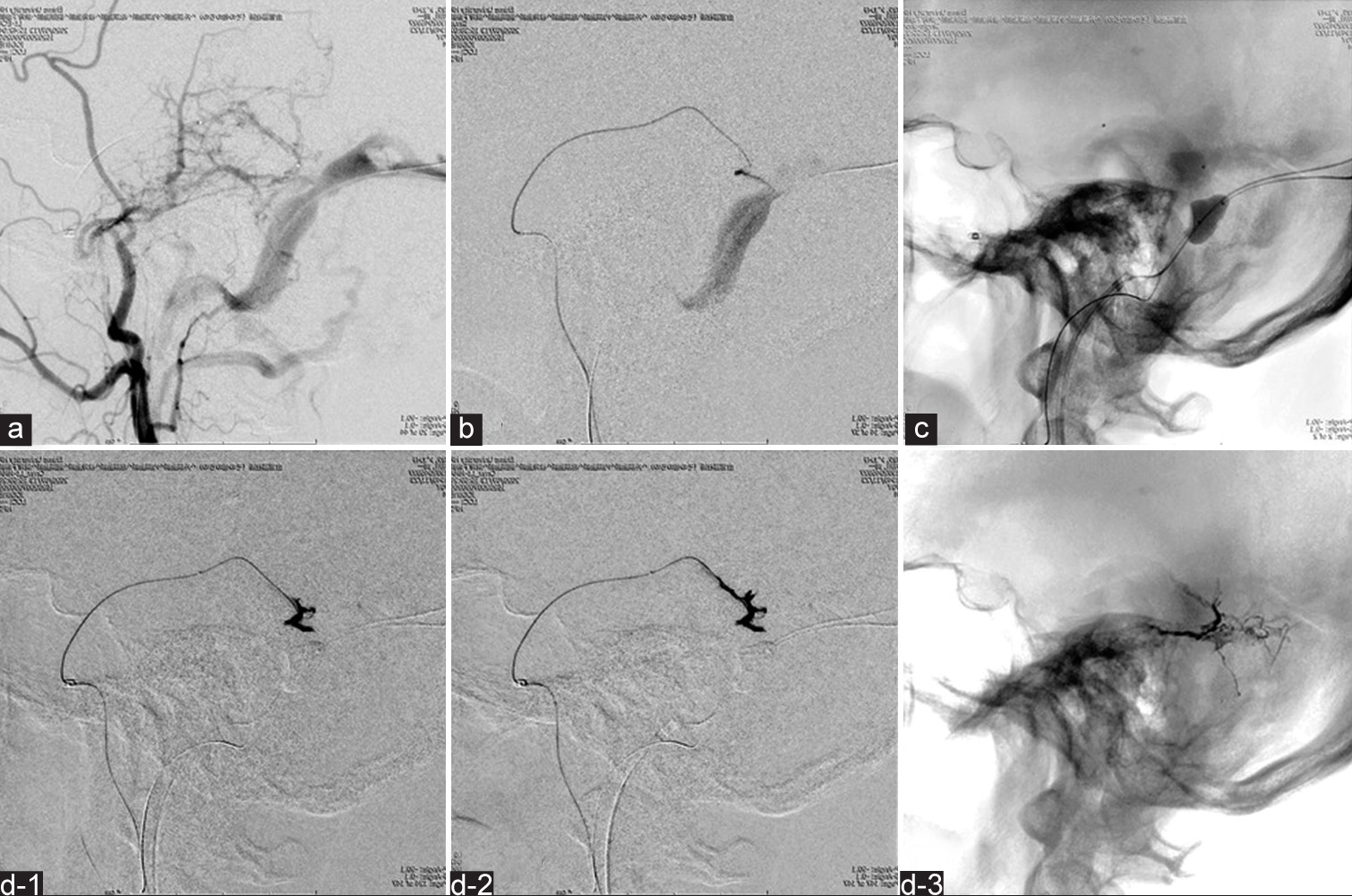
Figure 5:
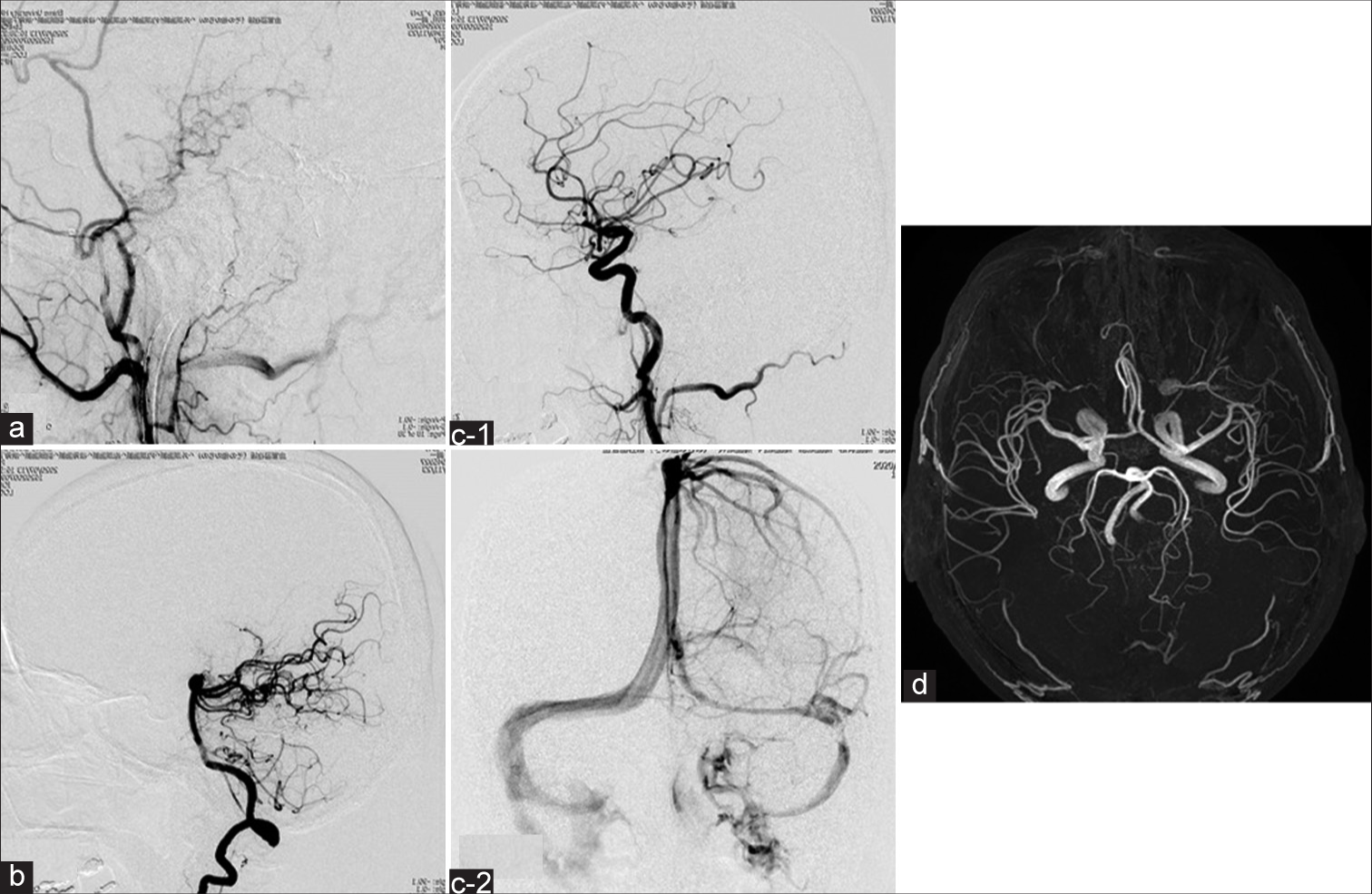
Postoperative cerebral angiography and MRA findings. (a-c) Digital subtraction angiography (a: left ECAG; b: left VAG; c-1: left ICAG) (lateral view) in the early arterial phase confirms complete disappearance of shunt flow. In the late venous phase, good antegrade venous perfusion of the left TS and SS to the left internal carotid vein is identified (c-2) left ICAG) (anterior-posterior view). (d) Follow-up MRA 12 months later shows left TS-SS venous flow has been well reconstructed and that the d-AVF has completely disappeared. MRA: Magnetic resonance angiography, ECAG: External carotid angiography, VAG: Vertebral artery angiography, ICAG: Internal carotid angiography, TS: Transverse sinus, SS: Sigmoid sinus, d-AVF: Dural arteriovenous fistula.
DISCUSSION
Cranial d-AVFs are a general term for lesions that occur in the meninges.[
The main object of d-AVF treatment is to prevent retrograde high flow shunt of the dural arteriovenous system into the cortical veins of the brain parenchyma.[
Compared to other embolic materials including n-butyl-2-cyanoacrylate, Onyx can be delivered more slowly, so embolization from the artery to the dural vein of d-AVF can be controlled more effectively with Onyx.[
Sinus protection by a transvenous balloon has been reported as another useful adjunct to endovascular treatment of d-AVF.[
CONCLUSION
We have described a case of d-AVF at the junction of the TS-SS, in which successful treatment was achieved by TAE combining application of Onyx with targeted balloon protection of the venous sinus to preserve a normal route of venous drainage. This unique technique using a sinus protection balloon not only provided complete occlusion of the d-AVF but also avoided venous compromise and reduced the risk of Onyx migration into the patent sinus. This novel assistive technique may represent an effective, innovative, and less-invasive treatment for d-AVF by TAE with Onyx.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ayad M, Eskioglu E, Mericle RA. Onyx: A unique neuroembolic agent. Expert Rev Med Devices. 2006. 3: 705-15
2. Brzozowski K, Narloch J, Piasecki P, Zięcina P, Koziarski A. Are Type I dural arteriovenous fistulas safe? Single-centre experience of endovascular treatment of dural arteriovenous fistulas. Pol J Radiol. 2019. 84: e179-84
3. Choi BJ, Lee TH, Kim CW, Choi CH. Reconstructive treatment using a stent graft for a dural arteriovenous fistula of the transverse sinus in the case of hypoplasia of the contralateral venous sinuses: Technical case report. Neurosurgery. 2009. 65: E994-6
4. Cognard C, Januel AC, Silva NA, Tall P. Endovascular treatment of intracranial dural arteriovenous fistulas with cortical venous drainage: New management using Onyx. AJNR Am J Neuroradiol. 2008. 29: 235-41
5. Davies MA, Ter Brugge K, Willinsky R, Wallace MC. The natural history and management of intracranial dural arteriovenous fistulae. Part. 2: Aggressive lesions. Interv Neuroradiol. 1997. 3: 303-11
6. Gross BA, Albuquerque FC, Moon K, McDougall CG. Evolution of treatment and a detailed analysis of occlusion, recurrence, and clinical outcomes in an endovascular library of 260 dural arteriovenous fistulas. J Neurosurg. 2017. 126: 1884-93
7. Jittapiromsak P, Ikka L, Benachour N, Spelle L, Moret J. Transvenous balloon assisted transarterial Onyx embolization of transverse-sigmoid dural arteriovenous malformation. Neuroradiology. 2013. 55: 345-50
8. Matsuo K, Fujita A, Kohta M, Kohmura E. Transarterial Onyx embolization with targeted balloon-assisted sinus protection for treatment of dural arteriovenous fistula of the lateral tentorial sinus. Radiol Case Rep. 2020. 15: 405-10
9. Mounayer C, Hammami N, Piotin M, Spelle L, Benndorf G, Kessler I. Nidal embolization of brain arteriovenous malformations using Onyx in 94 patients. AJNR Am J Neuroradiol. 2007. 28: 518-23
10. Newton TH, Cronqvist S. Involvement of Dural arteries in intracranial arteriovenous malformations. Radiology. 1969. 93: 1071-8
11. Nogueira RG, Dabus G, Rabinov JD, Eskey CJ, Ogilvy CS, Hirsch JA. Preliminary experience with onyx embolization for the treatment of intracranial dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2008. 29: 91-7
12. Piechowiak E, Zibold F, Dobrocky T, Mosimann PJ, Bervini D, Raabe A. Endovascular treatment of dural arteriovenous fistulas of the transverse and sigmoid sinuses using transarterial balloon-assisted embolization combined with transvenous balloon protection of the venous sinus. AJNR Am J Neuroradiol. 2017. 38: 1984-9
13. Rabinov JD, Yoo AJ, Ogilvy CS, Carter BS, Hirsch JA. ONYX versus n-BCA for embolization of cranial dural arteriovenous fistulas. J Neurointerv Surg. 2013. 5: 306-10
14. Wanke I, Rufenacht DA. The dural AV-fistula (DAVF), the most frequent acquired vascular malformation of the central nervous system (CNS). Clin Neuroradiol. 2015. 25: 325-32
15. Zhang Y, Li Q, Huang QH. Embolization of a superior sagittal sinus dural arteriovenous fistula under intrasinus balloon protection: A case report. Interv Neuroradiol. 2015. 21: 94-100