- Department of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan,
- Department of Neurosurgery, Southmead Hospital, North Bristol, United Kingdom,
- Department of Radiology, National Medical Centre, Karachi, Sindh, Pakistan,
- Department of Radiology, The Aga Khan University Hospital, Karachi, Sindh, Pakistan,
- Department of Radiology, Hyperfine, Guilford, Connecticut, United States.
Correspondence Address:
Syed Ather Enam, Department of Neurosurgery, Aga Khan University Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_123_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Altaf1, Muhammad Waqas Saeed Baqai2, Faiza Urooj1, Muhammad Sami Alam3, Hafiza Fatima Aziz1, Fatima Mubarak4, Edmond A. Knopp5, Khan M. Siddiqui5, Syed Ather Enam1. Utilization of an ultra-low-field, portable magnetic resonance imaging for brain tumor assessment in lower middle-income countries. 28-Jul-2023;14:260
How to cite this URL: Ahmed Altaf1, Muhammad Waqas Saeed Baqai2, Faiza Urooj1, Muhammad Sami Alam3, Hafiza Fatima Aziz1, Fatima Mubarak4, Edmond A. Knopp5, Khan M. Siddiqui5, Syed Ather Enam1. Utilization of an ultra-low-field, portable magnetic resonance imaging for brain tumor assessment in lower middle-income countries. 28-Jul-2023;14:260. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12470
Abstract
Background: Access to neuroimaging is limited in low-middle-income countries (LMICs) due to financial and resource constraints. A new, ultra-low-field, low-cost, and portable magnetic resonance imaging (pMRI) device could potentially increase access to imaging in LMICs.
Case Description: We have presented the first brain tumor case scanned using an Ultra-low-field pMRI at Aga Khan University Hospital in Karachi, Pakistan.
Conclusion: The imaging results suggest that the pMRI device can aid in neuroradiological diagnosis in resource-constrained settings. Further, research is needed to assess its compatibility for imaging other neurological disorders and compare its results with conventional MRI results.
Keywords: Brain tumors, Low-middle-income countries, Neuroimaging, Point-of-care, Portable magnetic resonance imaging, Ultra-low-field magnetic resonance imaging
INTRODUCTION
Magnetic resonance imaging (MRI) is essential for diagnosing brain tumors.[
The most significant deficit in neurosurgical care exists in Southeast Asia, where nearly 2.5 million cases go undiagnosed.[
OUR EXPERIENCE
We first employed this ULF pMRI machine for a 31-year-old female who presented to the neurosurgery clinic with a history of new-onset seizures for 1 year. The patient underwent high-field MRI (1.5 T MRI) and ULF pMRI (0.064 T) exams preoperatively and postoperatively, which were evaluated and compared by board-certified neuroradiologists.
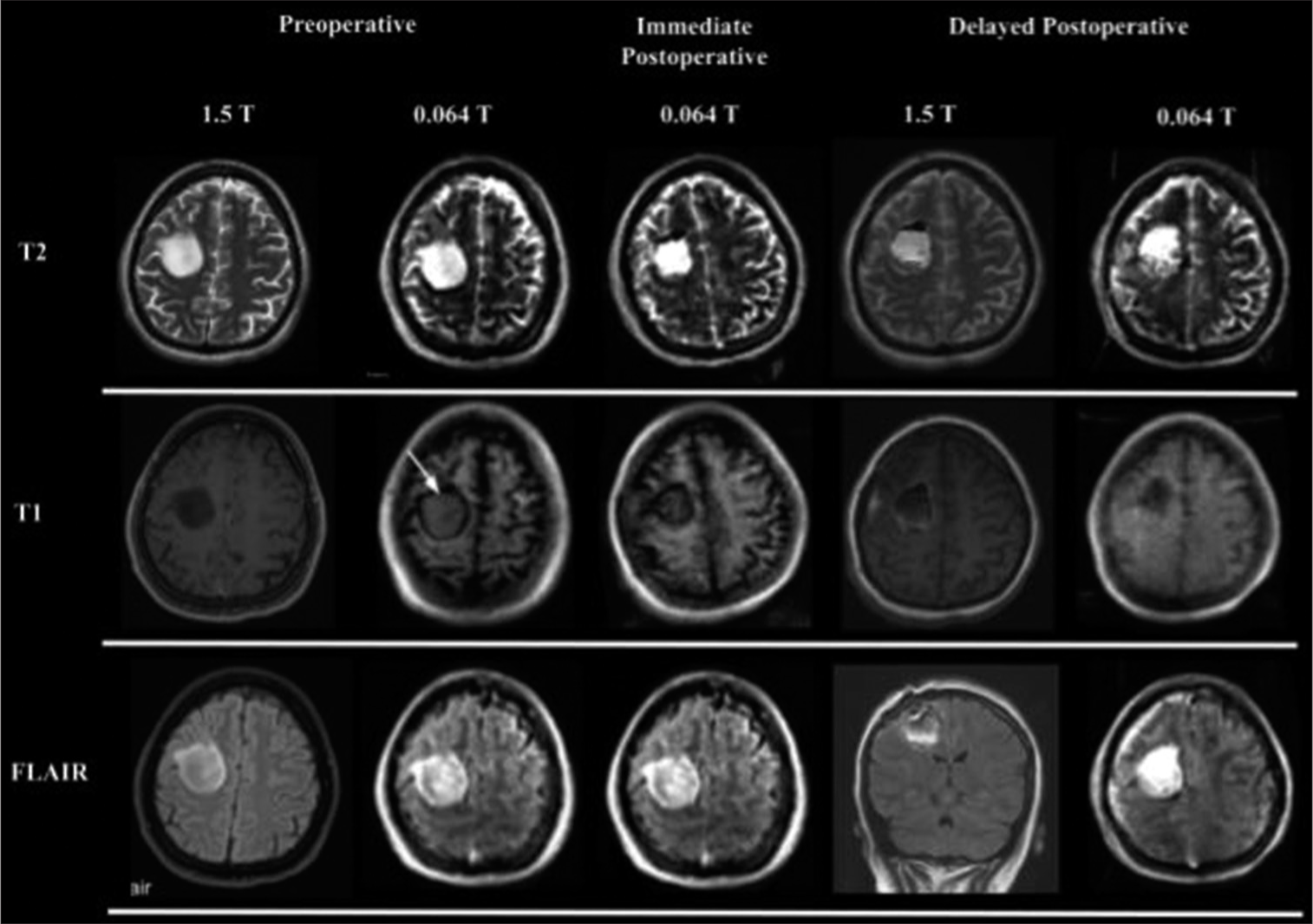
Figure 1:
Comparison of standard 1.5 T magnetic resonance imaging (MRI) and ultra-low-field portable MRI (ULF pMRI) Images of a brain tumor. The figure displays the preoperative MRI images of a patient with a brain tumor both obtained using a standard 1.5 T MRI and an ULF pMRI. Initial preoperative images on standard 1.5 T MRI localize a hyperintense lesion on T2 and fluid-attenuated inversion recovery sequences in the right centrum semiovale, involving deep and subcortical white matter with no surrounding edema. ULF pMRI reveals an isointense lesion with a non-specific hypointense rim (white arrow) on T1. The lesion was well-defined with no surrounding edema, or midline shift, nor any pressure effects. These findings were suggestive of low-grade glioma.
The high-field MRI scan revealed a right frontal intra-axial lesion which was hypointense on T1 with no contrast enhancement, hyperintense on T2, and had hyperintense foci on fluid-attenuated inversion recovery (FLAIR), along with prominent sulci and ventricles [
DISCUSSION
Advantages of pMRI in our experience
With the application of ULF pMRI in our setting, we could scan brain tumor patients at their bedside and in the operating room recovery area. Time is of the essence while identifying neurosurgical pathologies, and the accessibility of a pMRI MRI can expedite emergent medical care. Yuen et al.[
The ULF pMRI device is more cost-effective than the conventional MRI, as it does not require a dedicated MRI suite, and the machine is much cheaper ($3 million vs. $50,000).[
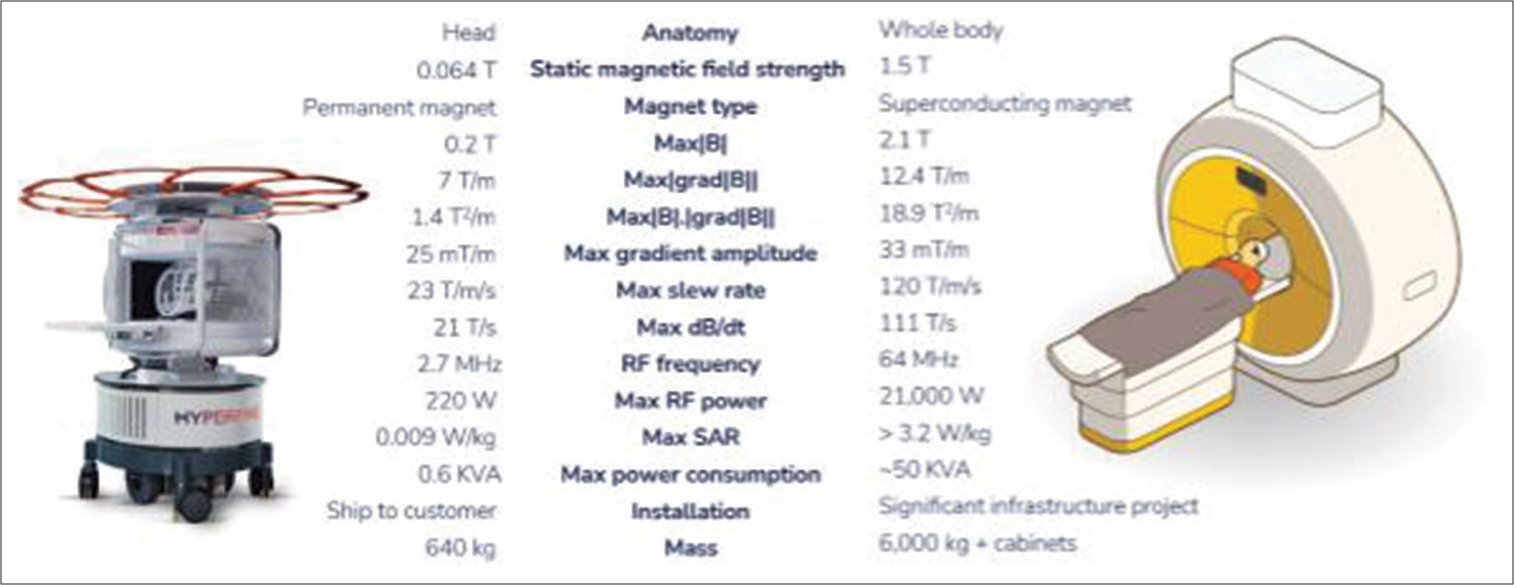
Although it has lower sensitivity, resolution, and signal-to-noise ratio than high-field conventional MRI [
Figure 2:
The comparison highlights the capabilities of the portable, ultra-low-field magnetic resonance imaging in providing comparable imaging quality to its conventional counterpart. Radiofrequency (RF), Specific Absorption Rate (SAR), magnetic field gradient (dB/dt), magnitude of the static magnetic field (Max |B|), maximum value of the magnitude of the gradient of the magnetic field (Max |grad|B||), overall strength of the magnetic field used during an MRI scan (Max |B|.|grad|B||)
Challenges that we faced
In our experience, one difference between ULF pMRI and traditional MRI is that the patient’s head has to be manually positioned inside the head coil before the scan can begin. Patients who have had neurosurgery require extra precautions during the postoperative period. Placing the patient’s head inside the device is a delicate task and requires trained personnel. In addition, since the height of the machine cannot be adjusted; therefore, this requires height-adjustable supports to appropriately place the patient’s head inside the pMRI scanner. Furthermore, due to the smaller frame of the ULF pMRI scanner’s head coil (261 mm x 205 mm) compared to the opening bore of around 500-600 cm in a traditional bore MRI machine, there is limited headroom for patients. This constraint may potentially heighten the chances of claustrophobia among adults undergoing ULF pMRI scans. Moreover, this ULF pMRI scanner can only perform brain MRIs with standard sequences (including T1, T2, Fluid attenuated inversion recovery, diffusion-weighted imaging, and apparent diffusion coefficient).
Recommendations
One of the changes that emerged as a result of the COVID-19 epidemic was a rapid transition to telemedicine. With the advent of modern mobile devices offering high-speed internet connections, coupled with the widespread availability of free, cutting-edge software for remote video communication there is tremendous potential for live, high-quality online consultations and the global exchange of medical knowledge.[
Although only some centers in an LMIC may be able to acquire this machine, incorporating this ULF pMRI scanner into mobile vans that can bring the imaging device directly to the patient would be a game changer. The geographic and logistics barriers to access essential health services in these regions are well-documented. Many patients are required to travel long distances over difficult terrain to reach the nearest clinic or hospital. In Pakistan, for instance, over half of the patients seeking neurosurgical care are required to travel over 50 km, and nearly, one-fifth are forced to travel 500 km to receive neurosurgical care.[
However, we must proceed with caution and conduct large-scale studies to fully understand the potential and limitations of ULF pMRI technology in LMICs. There are also significant challenges for conducting larger studies, such as cost, resource availability, and the need for international collaboration across institutions and countries. Despite these challenges, exploring alternative imaging technologies such as ULF pMRI is crucial to address the significant disparities in healthcare access and outcomes between high and low-income countries. Continued research in this area is essential to understand the full potential of ULF pMRI technology and its impact on global health.
CONCLUSION
The utilization of ULF pMRI shows promise in assessing brain tumors in resource-constrained settings, despite the need for improvements in image quality and resolution. Further research is necessary to explore its sensitivity to various neurological conditions and to conduct large-scale comparative studies with conventional MRI.
Declaration of patient consent
The Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
This research was supported by a grant from Hyperfine Research Inc. to the Pakistan Academy of Neurological Surgery (PANS).
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bajwa MH, Shah MM, Khalid MU, Khan AA, Zahid N, Anis SB. Distance travelled for brain tumour surgery: An low and middle income country’s perspective. J Pak Med Assoc. 2022. 72: S25-33
2. Branco P, Ayres-Basto M, Portugal P, Ramos I, Seixas D. Brain magnetic resonance imaging: Perception and expectations of neurologists, neurosurgeons and psychiatrists. Neuroradiol J. 2014. 27: 261-7
3. Brenner DJ, Hricak H. Radiation exposure from medical imaging: Time to regulate?. JAMA. 2010. 304: 208-9
4. Dewan MC, Rattani A, Fieggen G, Arraez MA, Servadei F, Boop FA. Global neurosurgery: The current capacity and deficit in the provision of essential neurosurgical care. Executive summary of the global neurosurgery initiative at the program in global surgery and social change. J Neurosurg. 2018. 130: 1055-64
5. Enderlin M. The Impact of Patient Acuity and Staffing Shortages on Hospitals and Neurocritical Care. Available from: https://hyperfine.io/resources/blog/the-impact-of-patient-acuity-and-staffing-shortages-on-hospitals-and-neurocritical-care [Last accessed on 2023 May 30].
6. FDA Clears ‘World’s First’ Portable, Low-cost MRI Following Positive Clinical Research. Available from: https://healthimaging.com/topics/healthcare-policy/fda-clear-worlds-first-portable-mri [Last accessed on 2022 Sep 23].
7. Hricak H, Abdel-Wahab M, Atun R, Lette MM, Paez D, Brink JA. Medical imaging and nuclear medicine: A lancet oncology commission. Lancet Oncol. 2021. 22: e136-72
8. Marques JP, Simonis FFJ, Webb AG. Low-field MRI: An MR physics perspective. J Magn Reson Imaging. 2019. 49: 1528-42
9. Mazurek MH, Cahn BA, Yuen MM, Prabhat AM, Chavva IR, Shah JT. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun. 2021. 12: 5119
10. MRI NMR Magnetic Resonance Essentials, Introduction, Basic Principles, Facts, History-the Primer of EMRF/TRTF-Facts and Figures: Organ Distribution of MRI Studies-Number of MRI Machines Worldwide-Field Strength of MRI Machines. Available: https://www.magnetic-resonance.org/ch/21-01.html [Last accessed on 2022 Oct 10].
11. Ogbole GI, Adeyomoye AO, Badu-Peprah A, Mensah Y, Nzeh DA. Survey of magnetic resonance imaging availability in West Africa. Pan Afr Med J. 2018. 30: 240
12. Prabhat AM, Crawford AL, Mazurek MH, Yuen MM, Chavva IR, Ward A. Methodology for low-field, portable magnetic resonance neuroimaging at the bedside. Front Neurol. 2021. 12: 760321
13. Shetewi SG, Mutairi BS, Bafaraj SM. The role of imaging in examining neurological disorders: Assessing brain, stroke, and neurological disorders using CT and MRI imaging. Adv Comput Tomogr. 2020. 9: 1-11
14. Szmuda T, Ali S, Słoniewski P. Telemedicine in neurosurgery during the novel coronavirus (COVID-19) pandemic. Neurol Neurochir Pol. 2020. 54: 207-8
15. Welling RD, Azene EM, Kalia V, Pongpirul K, Starikovsky A, Sydnor R. White paper report of the 2010 RADAID conference on international radiology for developing countries: Identifying sustainable strategies for imaging services in the developing world. J Am Coll Radiol. 2011. 8: 556-62
16. Yuen MM, Prabhat AM, Mazurek MH, Chavva IR, Crawford A, Cahn BA. Portable, low-field magnetic resonance imaging enables highly accessible and dynamic bedside evaluation of ischemic stroke. Sci Adv. 2022. 8: eabm3952