- Department of Neurosurgery, Miami University, Miami, United States
- Hacettepe University School of Medicine, Ankara, Turkey
- Department of Neurosurgery, School of Medicine, Ankara University, Ankara, Turkey
Correspondence Address:
Muhammet Enes Gurses, Department of Neurosurgery, Miami University, Miami, United States.
DOI:10.25259/SNI_231_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammet Enes Gurses1, Victor M. Lu1, Neslihan Nisa Gecici2, Khushi Hemendra Shah1, Elif Gökalp3, Malek Bashti1, Sameah Haider1, Ricardo J. Komotar1. Utilizing tubular retractors in colloid cyst resection: A single surgeon experience. 31-May-2024;15:179
How to cite this URL: Muhammet Enes Gurses1, Victor M. Lu1, Neslihan Nisa Gecici2, Khushi Hemendra Shah1, Elif Gökalp3, Malek Bashti1, Sameah Haider1, Ricardo J. Komotar1. Utilizing tubular retractors in colloid cyst resection: A single surgeon experience. 31-May-2024;15:179. Available from: https://surgicalneurologyint.com/surgicalint-articles/12920/
Abstract
Background: Colloid cysts are intracranial lesions originating from abnormalities in the primitive neuroepithelium folding of the third ventricle. Various surgical approaches have been explored for the management of colloid cysts, each carrying its own set of advantages and limitations. Tubular retractors developed recently alleviate retraction pressure through radial distribution, potentially offering benefits for colloid cyst resection. This study aims to introduce and assess a modified microsurgical method utilizing the tubular retractor for addressing colloid cysts.
Methods: The study included a retrospective assessment of patients who had colloid cysts and who were treated between 2015 and 2023 by one experienced surgeon. The demographic, clinical, radiological, histological, and surgical data regarding these patients were evaluated. The patients were assessed using the colloid cyst risk score, indicating a risk for obstructive hydrocephalus.
Results: The minimally invasive microsurgical approach was successfully applied to all 22 identified patients. No postoperative surgical complications were reported. Gross total resection was achieved in 21 (95.5%) patients. The early complication rate was 22.7% (n = 5). There were no postoperative seizures, permanent neurological deficits, or venous injuries. The average hospital stay was 3 days. There was no evidence of recurrence at an average follow-up length of 25.9 months.
Conclusion: The transtubular approach is an effective, safe method for treating colloid cysts. It achieves complete cyst removal with minimal complications, offering the benefits of less invasiveness, improved visualization, and reduced tissue disruption, strengthening its role in colloid cyst surgery.
Keywords: Colloid cyst, Microsurgical approach, Minimally invasive surgery, Outcomes, Tubular retractor
INTRODUCTION
Colloid cysts in the third ventricle are rare, making up only about 1% of all intracranial tumors. [
There are several standard surgical options for removing colloid cysts in the third ventricle. These include transcortical trans ventricular, interhemispheric transcallosal, and endoscopic approaches.[
Traditional systems such as the Greenberg or Leyla retractors, though effective, often present issues due to their bulky nature and the potential for causing significant cortical and vascular damage during aggressive retraction, as demonstrated in animal studies.[
MATERIALS AND METHODS
Patient selection
This retrospective study received approval from the Institutional Review Board, with the consent process waived. All patients who underwent colloid cyst resection with the use of tubular retractors by the senior neurosurgeon (R.J.K.) at our institution between 2015 and 2023 were included in the study. To identify relevant patients, we reviewed the senior neurosurgeon’s clinical database. We collected clinical data from electronic medical records, including demographic information, initial symptoms, surgical data, and postoperative neurological status of the patients. The BrainPath system (NICO Corp, Indianapolis, Indiana) and the ViewSite Brain Access System (VBAS; Vycor Medical Inc, Boca Raton, Florida) were utilized in these procedures. The BrainPath tubular retractor system has a smaller working diameter (13.5 mm) compared to the VBAS system by Vycor Medical (17 mm). Despite this disparity in size, both tubular retractors share a similar technique and approach. The advantage of the BrainPath retractor lies in its narrower working diameter, potentially resulting in less disruption of normal brain tissue during the procedure. On the other hand, the VBAS system’s larger working area presents an advantage in tackling larger lesions, potentially facilitating their resection more effectively.
We assessed the patients using the colloid cyst risk score (CCRS). T1 contrast-enhanced, T2, and fluid-attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) images were evaluated. Preoperative cyst volume was determined using the formula 4/3πr1r2r3. Early complications were defined as complications occurring within the 1st week of post-surgery.
Operative technique
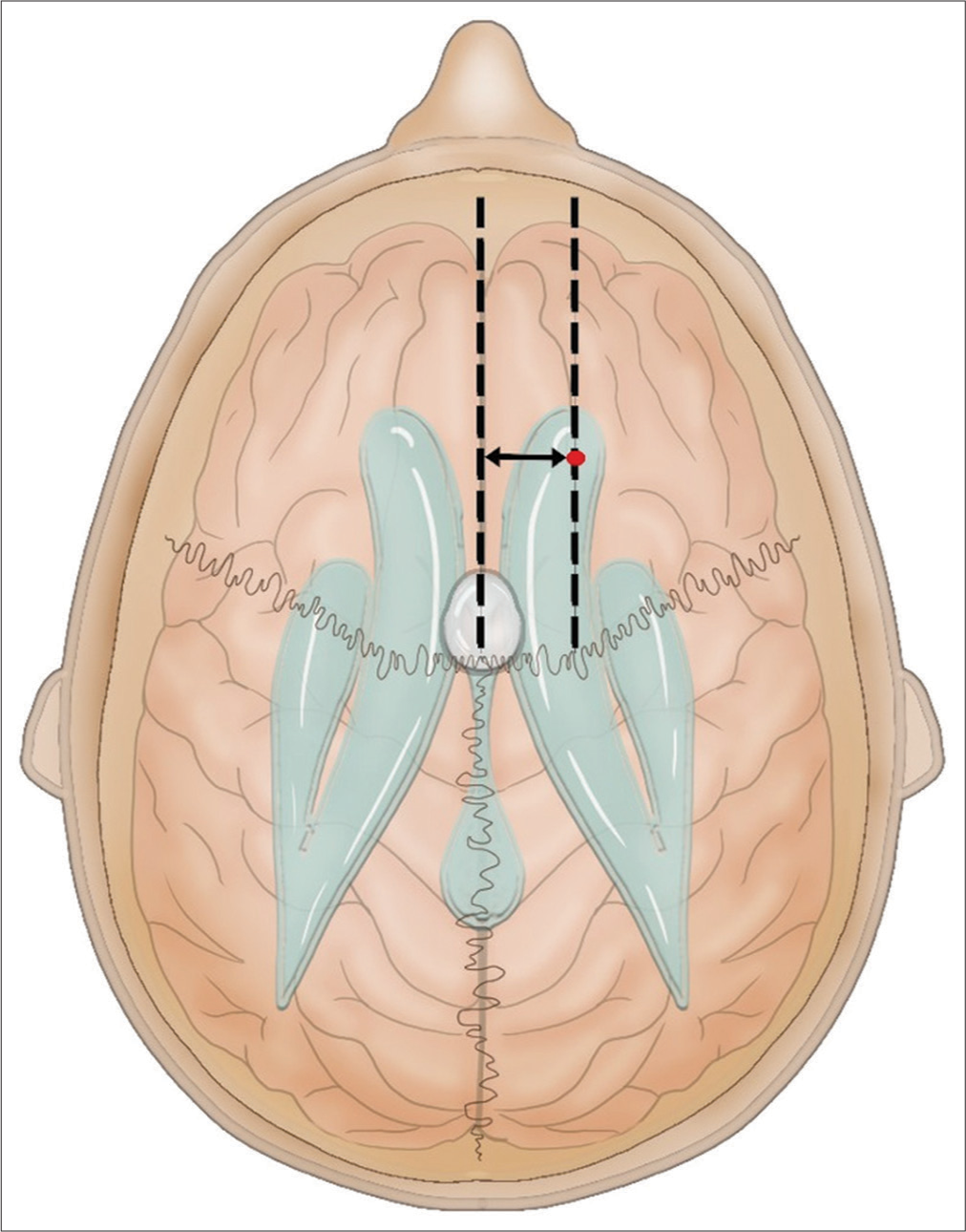
All patients underwent preoperative MRI, encompassing gadolinium-enhanced and fluid-attenuated inversion recovery sequences, with fiducial markers placed for utilization alongside navigation and preoperative trajectory planning. Following intubation and anesthesia induction, patients were immobilized in a Mayfield head holder and registered within the navigation system. The incision and craniotomy were strategically planned according to the lesion’s location, utilizing navigation for precise trajectory and guidance. All surgeries were performed with patients in a supine position. Typically, the entry point is situated approximately at Kocher’s point [
Case example: Patient 14
A 59-year-old male with a past medical history of hypertension, hyperlipidemia, and gout presented in July 2020 with a chief complaint of progressively worsening altered mental status and headaches over the past several weeks. A computed tomography (CT) scan revealed obstructive hydrocephalus, with a notable large lesion identified in the foramen of Monro. Urgent admission was necessitated, and subsequent MRI substantiated the presence of a spherical 2.6 cm × 2.6 cm × 2.3 cm cystic-appearing mass centered at the foramen of Monro in Zone I [
Figure 3:
Patient 14. Preoperative and postoperative magnetic resonance imaging (MRI) of a patient with a colloid cyst with a volume of 70.92 cm3. (a) Preoperative T2-weighted axial fluid-attenuated inversion recovery (FLAIR) MRI. (b) Preoperative T1-weighted sagittal MRI. (c) Postoperative T2-weighted axial FLAIR MRI. (d) Postoperative T2-weighted axial FLAIR MRI showing tubular retractor trajectory.
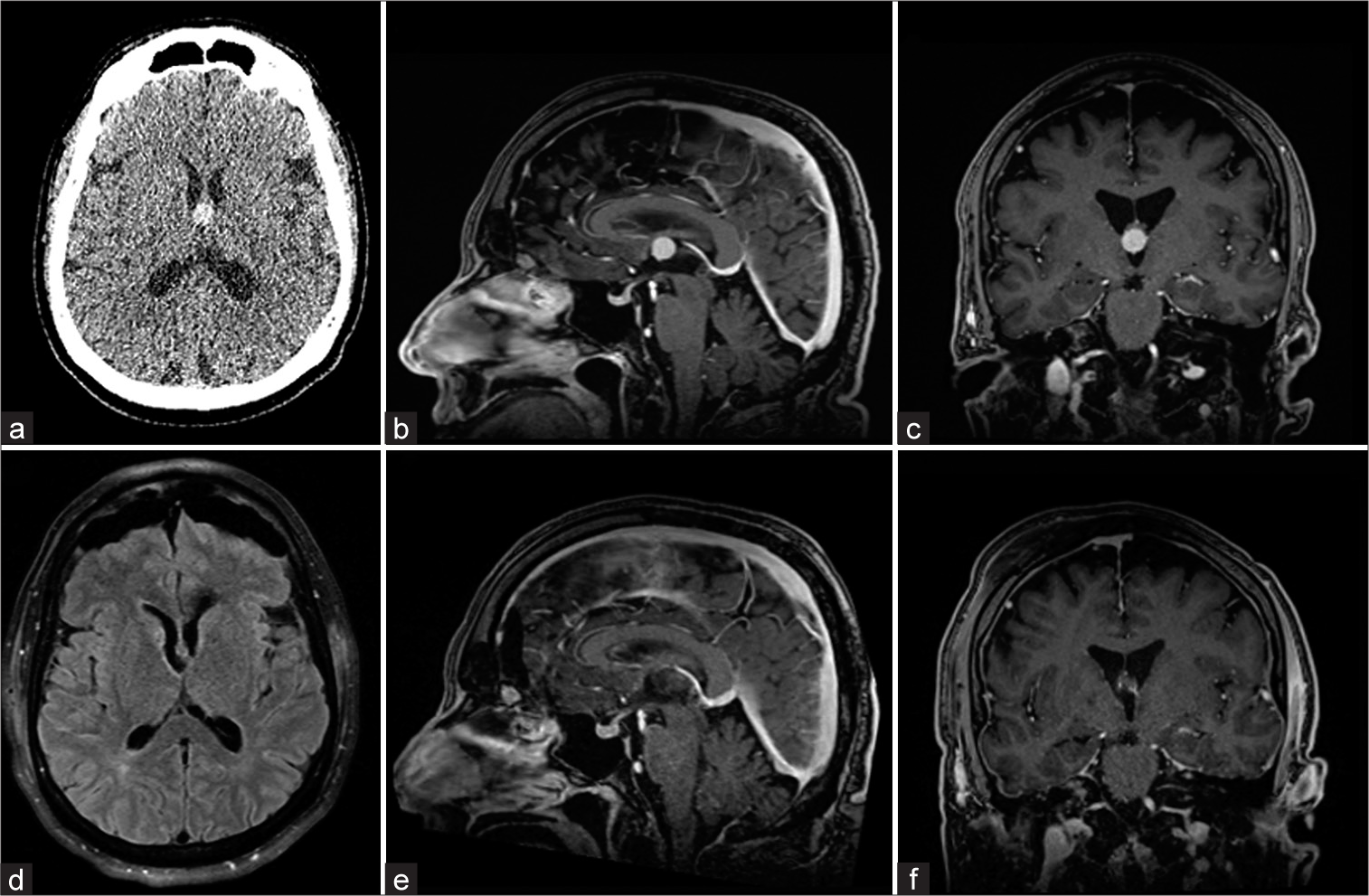
Case example: Patient 22
A 69-year-old male with a past medical history of hypertension and thrombosis presented to the clinic in August 2023 with complaints of headache and a syncope event. A CT scan revealed a third ventricular colloid cyst with no acute hydrocephalus. MRI substantiated a stable spherical 1.15 cm × 1.19 cm × 1.15 cm homogenously high T2 lesion in the anterosuperior aspect of the third ventricle centered at the foramen of Monroe in Zone II suggestive of a colloid cyst [
Figure 5:
Patient 22. Preoperative and postoperative magnetic resonance imaging (MRI) of a patient with a colloid cyst with a volume of 6.59 cm3. (a) Preoperative computed tomography. (b) Preoperative T1-weighted contrast-enhanced sagittal MRI. (c) Preoperative T1-weighted contrast-enhanced coronal MRI. (d) Postoperative T2-weighted axial fluid-attenuated inversion recovery MRI. (e) Postoperative T1-weighted contrast-enhanced sagittal MRI. (f) Postoperative T1-weighted contrast-enhanced coronal MRI.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences 23.0 software (IBM, New York). Categorical variables were presented as numbers and percentages, and continuous variables were presented as means ± Standard deviation. Two-group comparisons for categorical variables were performed using Chi-square and Fisher’s exact tests, while comparisons for continuous variables were conducted using the independent samples t-test. Receiver operating characteristic analysis was performed to evaluate the accuracy of the CCRS score in predicting the risk of obstructive hydrocephalus.
RESULTS
Twenty-two colloid cyst resections were performed at our institution. Patient demographics are shown in
Gross total resection was achieved in 95.5% (n = 21) of cases [
Every patient was discharged to home in good condition with an average hospital stay of 3 ± 1.34 days, with a range of discharge on postoperative day 2–day 7. Five (22.7%) patients had early complications: two with confusion, one with short-term memory difficulties, and one with mild dizziness. One patient had urinary retention post-operatively. All of the early complications resolved within 5 days of surgery. No patients experienced permanent complications. There was no evidence of recurrence or progression during an average follow-up of 25.9 ± 25.02 months.
Our analysis did not reveal a significant association between the size of the colloid cyst, axial and greatest diameter of the cyst, and CCRS of greater or equal to 4 [
DISCUSSION
This is the largest single-surgeon experience in the literature to date using tubular retractors for colloid cyst resection. The channel-based transcortical-transtubular approach appears to be an effective and safe method for treating colloid cysts based on our institutional experience. The procedure demonstrated favorable surgical outcomes, with complete cyst removal and no permanent postoperative complications. Further, prospective data are needed to establish the learning curve to make this an appropriate tool in the surgeon’s armamentarium when presented with a colloid cyst for surgical evaluation.
The utilization of endoscopy in the extraction of third ventricular colloid cysts has garnered favor in various medical institutions. Neuroendoscopy demonstrates efficacy in evacuating cyst contents and coagulating the cyst wall. Nevertheless, the endoscopic approach, mainly due to the significant prevalence of incomplete removal, was documented in previous reports within the medical literature.[
Tubular systems for deep-seated lesions are known for causing less tissue trauma, reducing intrusion into normal tissue, and enabling traditional microsurgical techniques.[
We believe that the results of our study demonstrate the effectiveness and a reasonably safe profile for the use of tubular retractors in colloid cyst resections. We achieved a gross total resection rate of 95.5%, which is consistent with reported rates using this modality and surpasses those of endoscopic approaches.[
We employed the CCRS to assess our patients preoperatively, as outlined by Beaumont et al., which proved instrumental in evaluating preoperative risk.[
Notably, in our study cohort, 21 (95.5%) patients exhibited a CCRS score of 3 or higher [
In our institution, we have observed that employing the transcortical-trans tubular approach for colloid cyst removal proves effective and maintains a reasonably safe profile. However, there is a scarcity of comprehensive comparative data between this approach and established microsurgical and endoscopic methods. Further, extensive studies involving larger series and comparative analyses between various surgical approaches are necessary. Nonetheless, the field of neurosurgical technology is progressing, paving the way for continuous evolution in the treatment of deeply located brain lesions. Anticipated advancements in neuronavigation and surgical robotics are likely to surpass current methodologies. Notably, transcortical-trans tubular approaches to the third ventricle have exhibited both safety and effectiveness, warranting consideration, especially when confronted with challenging deep-seated lesions.
Limitations
A significant limitation of our study is its retrospective nature. Retrospective studies inherently carry the risk of selection bias, incomplete data, and the inability to control or standardize data collection methods. In addition, neuropsychological assessment for long-term memory complaints was not performed. These limitations could impact the overall robustness of our findings and the validity of the conclusions drawn. Our analysis was based on a relatively small number of patients, which may restrict the generalizability of our results. Larger and more diverse datasets would provide a more comprehensive and reliable assessment of the predictive capabilities of this technique.
CONCLUSION
The channel-based transcortical-trans tubular approach is an effective and safe method for treating colloid cysts. The procedure demonstrated favorable surgical outcomes, with complete cyst removal and no permanent postoperative complications. This approach offers the advantages of minimal invasiveness, optimal visualization, and reduced glial tissue incision, further establishing its viability in the management of colloid cysts in the third ventricle.
Ethical approval
The research/study approved by the Institutional Review Board at University of Miami, number 221078, dated October 13, 2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdou MS, Cohen AR. Endoscopic treatment of colloid cysts of the third ventricle. Technical note and review of the literature. J Neurosurg. 1998. 89: 1062-8
2. Beaumont TL, Limbrick DD, Rich KM, Wippold FJ, Dacey RG. Natural history of colloid cysts of the third ventricle. J Neurosurg. 2016. 125: 1420-30
3. Boogaarts HD, Decq P, Grotenhuis JA, Le Guerinel C, Nseir R, Jarraya B. Long-term results of the neuroendoscopic management of colloid cysts of the third ventricle: A series of 90 cases. Neurosurgery. 2011. 68: 179-87
4. Cabbell KL, Ross DA. Stereotactic microsurgical craniotomy for the treatment of third ventricular colloid cysts. Neurosurgery. 1996. 38: 301-7
5. Camacho A, Abernathey CD, Kelly PJ, Laws ER. Colloid cysts: Experience with the management of 84 cases since the introduction of computed tomography. Neurosurgery. 1989. 24: 693-700
6. Connolly ID, Johnson E, Lamsam L, Veeravagu A, Ratliff J, Li G. Microsurgical vs. endoscopic excision of colloid cysts: An analysis of complications and costs using a longitudinal administrative database. Front Neurol. 2017. 8: 259
7. Desai KI, Nadkarni TD, Muzumdar DP, Goel AH. Surgical management of colloid cyst of the third ventricle--a study of 105 cases. Surg Neurol. 2002. 57: 295-302 discussion-302-4
8. Goel A. Can the hype of “endoscope” become a reality for colloid cyst surgery?. World Neurosurg. 2013. 80: 500-1
9. Gokalp HZ, Yuceer N, Arasil E, Erdogan A, Dincer C, Baskaya M. Colloid cyst of the third ventricle. Evaluation of 28 cases of colloid cyst of the third ventricle operated on by transcortical transventricular (25 cases) and transcallosal/transventricular (3 cases) approaches. Acta Neurochir (Wien). 1996. 138: 45-9
10. Greenfield JP, Cobb WS, Tsouris AJ, Schwartz TH. Stereotactic minimally invasive tubular retractor system for deep brain lesions. Neurosurgery. 2008. 63: 334-9 discussion 339-40
11. Hajtovic S, Sun J, Multani JS, Herrmann LL, Britton H, Gautreaux J. Surgical cytoreduction of deep-seated high-grade glioma through tubular retractor. J Neurosurg. 2023. 139: 73-84
12. Harris AE, Hadjipanayis CG, Lunsford LD, Lunsford AK, Kassam AB. Microsurgical removal of intraventricular lesions using endoscopic visualization and stereotactic guidance. Neurosurgery. 2005. 56: 125-32
13. Hellwig D, Bauer BL, Schulte M, Gatscher S, Riegel T, Bertalanffy H. Neuroendoscopic treatment for colloid cysts of the third ventricle: The experience of a decade. Neurosurgery. 2003. 52: 525-33 discussion 532-3
14. Hellwig D, Bauer BL, Schulte M, Gatscher S, Riegel T, Bertalanffy H. Neuroendoscopic treatment for colloid cysts of the third ventricle: The experience of a decade. Neurosurgery. 2008. 62: 1101-9
15. Hernesniemi J, Leivo S. Management outcome in third ventricular colloid cysts in a defined population: A series of 40 patients treated mainly by transcallosal microsurgery. Surg Neurol. 1996. 45: 2-14
16. Horn EM, Feiz-Erfan I, Bristol RE, Lekovic GP, Goslar PW, Smith KA. Treatment options for third ventricular colloid cysts: Comparison of open microsurgical versus endoscopic resection. Neurosurgery. 2007. 60: 613-8 discussion 618-20
17. Jeffree RL, Besser M. Colloid cyst of the third ventricle: A clinical review of 39 cases. J Clin Neurosci. 2001. 8: 328-31
18. Jo KI, Chung SB, Jo KW, Kong DS, Seol HJ, Shin HJ. Microsurgical resection of deep-seated lesions using transparent tubular retractor: Pediatric case series. Childs Nerv Syst. 2011. 27: 1989-94
19. Kashkoush AI, El-Abtah ME, Achey R, Winkelman R, Glauser G, Patterson TE. Prognosticators of functional outcome after supratentorial minimally invasive intracranial hemorrhage evacuation with tubular retractor systems. Oper Neurosurg (Hagerstown). 2023. 25: 408-16
20. Kelly PJ, Goerss SJ, Kall BA. The stereotaxic retractor in computer-assisted stereotaxic microsurgery. Technical note. J Neurosurg. 1988. 69: 301-6
21. Kelly PJ, Kall BA, Goerss SJ. Computer-interactive stereotactic resection of deep-seated and centrally located intraaxial brain lesions. Appl Neurophysiol. 1987. 50: 107-13
22. Li B, Kim MG, Dominguez J, Feldstein E, Kleinman G, Hanft S. Intraventricular choroid plexus cavernoma resection using tubular retractor system and exoscope visualization: A technical case report. Oper Neurosurg (Hagerstown). 2022. 22: e134-7
23. Lin M, Bakhsheshian J, Strickland B, Rennert RC, Chen JW, Van Gompel JJ. Navigable channel-based trans-sulcal resection of third ventricular colloid cysts: A multicenter retrospective case series and review of the literature. World Neurosurgery. 2020. 133: e702-10
24. Mathiesen T, Grane P, Lindgren L, Lindquist C. Third ventricle colloid cysts: A consecutive 12-year series. J Neurosurg. 1997. 86: 5-12
25. Mathiesen T, Grane P, Lindquist C, von Holst H. High recurrence rate following aspiration of colloid cysts in the third ventricle. J Neurosurg. 1993. 78: 748-52
26. Okasha M, Ineson G, Pesic-Smith J, Surash S. Transcortical approach to deep-seated intraventricular and intra-axial tumors using a tubular retractor system: A technical note and review of the literature. J Neurol Surg A Cent Eur Neurosurg. 2021. 82: 270-7
27. Pollock BE, Huston J. Natural history of asymptomatic colloid cysts of the third ventricle. J Neurosurg. 1999. 91: 364-9
28. Rangwala SD, Briggs RG, Ruzevick J, Zada G. Exoscope-assisted, channel-based approach for resection of 3rd ventricular colloid cyst: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2023. 25: e101-2
29. Rosenorn J, Diemer N. The risk of cerebral damage during graded brain retractor pressure in the rat. J Neurosurg. 1985. 63: 608-11
30. Rosenorn J, Diemer NH. Reduction of regional cerebral blood flow during brain retraction pressure in the rat. J Neurosurg. 1982. 56: 826-9
31. Sampath R, Vannemreddy P, Nanda A. Microsurgical excision of colloid cyst with favorable cognitive outcomes and short operative time and hospital stay: Operative techniques and analyses of outcomes with review of previous studies. Neurosurgery. 2010. 66: 368-74 discussion 74-5
32. Sefcikova V, Wong QH, Samandouras G. Practical, stereotactic, low-profile technique for transcortical/transventricular colloid cyst removal independent of ventricular size: Technical note and analysis of approaches. Oper Neurosurg (Hagerstown). 2023. 24: e61-7
33. Sheikh AB, Mendelson ZS, Liu JK. Endoscopic versus microsurgical resection of colloid cysts: A systematic review and meta-analysis of 1,278 patients. World Neurosurg. 2014. 82: 1187-97
34. Stachura K, Grzywna E, Krzyzewski RM, Kwinta BM. Retrospective evaluation of endoscopic treatment in colloid cyst of the third ventricle. Wideochir Inne Tech Maloinwazyjne. 2021. 16: 604-11
35. Zhong J, Dujovny M, Perlin AR, Perez-Arjona E, Park HK, Diaz FG. Brain retraction injury. Neurol Res. 2003. 25: 831-8