- Department of Neurosurgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States.
DOI:10.25259/SNI_75_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Paul Samuel Page, Stewart Paige, Amgad Hanna. Vascular entrapment neuropathy of the tibial nerve within the gastrocnemius muscle. 17-May-2021;12:224
How to cite this URL: Paul Samuel Page, Stewart Paige, Amgad Hanna. Vascular entrapment neuropathy of the tibial nerve within the gastrocnemius muscle. 17-May-2021;12:224. Available from: https://surgicalneurologyint.com/surgicalint-articles/10815/
Abstract
Background: Vascular compression is an extremely rare cause of mononeuropathy and compression of selective tibial nerve branches is an additionally a rare finding and makes diagnosis difficult.
Case Description: Here within, we describe the case of a 41-year-old male who presented with isolated mononeuropathy of the medial gastrocnemius (MG) branch of the tibial nerve presented as persistent fasciculations and atrophy. After electromyography and clinical evaluation, surgical exploration was recommended. A vascular bundle was found to be compressing the MG branch of the tibial nerve and thus was ligated to decompress the nerve. Postoperatively, all fasciculations improved and muscle atrophied improved.
Conclusion: Vascular compression resulting in mononeuropathy of the peripheral nerves is a rare clinical entity. Clinicians should include these etiologies on their differential when considering surgical exploration of mononeuropathies.
Keywords: Punched nerve syndrome, Tibial neuropathy, Vascular compression
INTRODUCTION
Tibial neuropathy is a common clinical entity that has been described as a result of compression. The most common location occurs under the soleal arch or in the tarsal tunnel. In addition to these sites, other sites of compression have been identified as well as localized injury and compression of individual branches. While most causes of tibial neuropathy remain idiopathic, other causes include trauma, mechanical irritation, and tumors.
More recently, ultrasonographic literature describes the “punched-nerve-syndrome” as a rare condition where direct vicinity to a vascular structure leads to chronic neural damage due to repetitive pulsatile compression.[
CASE REPORT
A 41-year-old male presented to clinic with a 2.5-year history of painful right MG atrophy and fasciculations following a previous gastrocnemius tear after a fall from a treadmill. He was initially seen by neurology where his right MG appeared significantly wasted compared to his right lateral gastrocnemius. On examination, fasciculations were present and limited to his right gastrocnemius with no reliable inciting triggers. On motor examination, his strength was MRC Grade 5/5 in all muscle groups, including plantar flexion and inversions, and deep tendon reflexes were 2+ and symmetric. Further workup with electromyography (EMG) revealed a possible focal neuropathy of the right tibial nerve branch supplying the MG, as evidenced by increased insertional activity, 3+ fasciculations, and 1+ spike and wave activity in the MG. All other EMGs on muscle group testing were normal. There was no evidence of radiculopathy, plexopathy, or proximal sciatic neuropathy. Subsequent MRI illustrated his tibial and common peroneal nerve had normal morphology without any structural evidence or injury to explain his EMG findings. Ultimately, the decision was made for a right tibial nerve exploration at the level of the popliteal fossa with decompression and possible grafting of the MG branch.
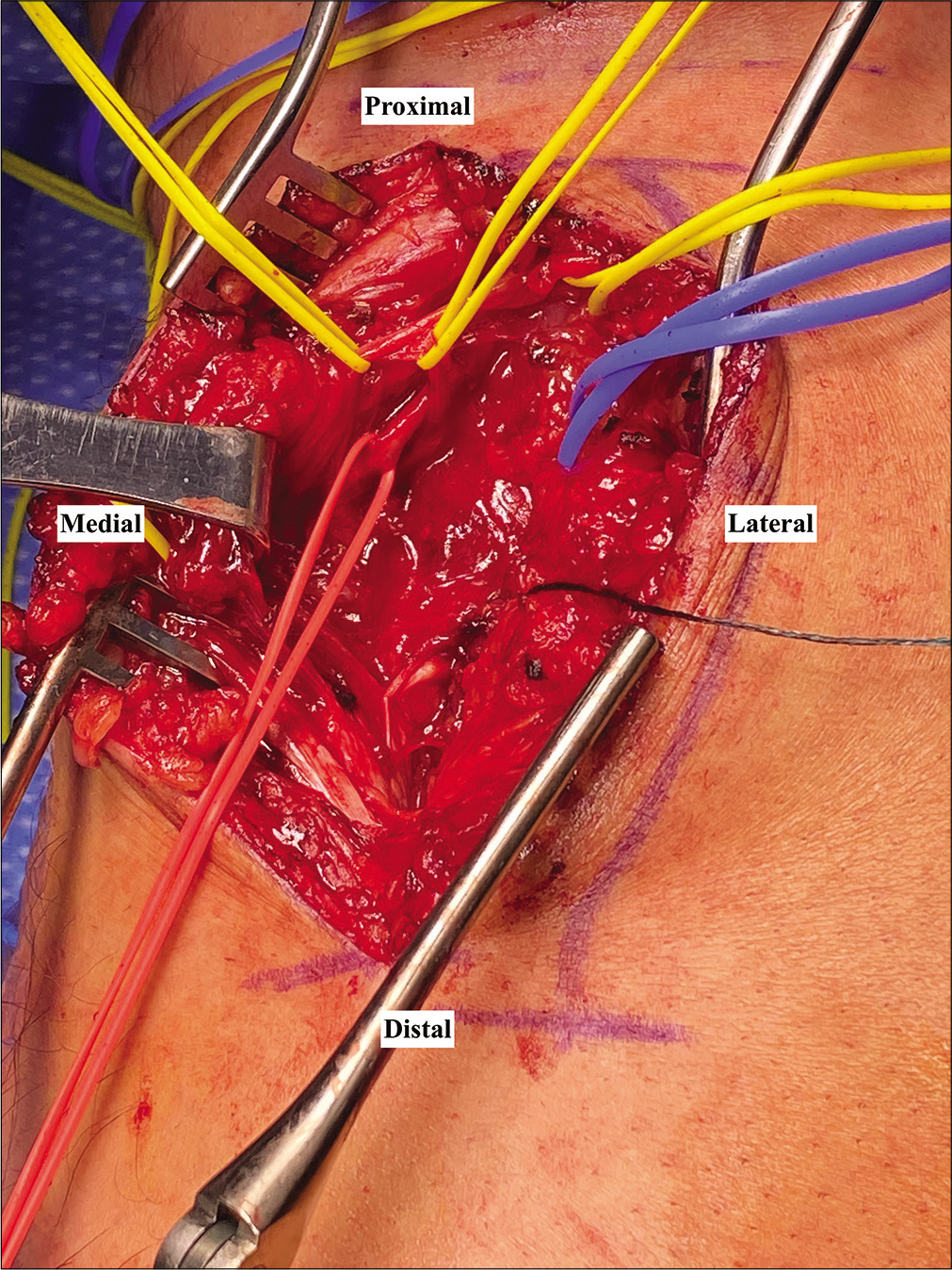
On exploration, both the medial and lateral gastrocnemius muscles were easily identified along with the sciatic nerve and associated tibial and common fibular nerve branch points. Of interest, there were three distinct muscle head contributions to the MG. It was unclear, however, whether this anomaly was congenital or secondary to his previous injury. Nerve identifications were confirmed with intraoperative checkpoint nerve stimulator under direct visualization. Three MG branches were identified arising from the tibial nerve. Unexpectedly, we found large vasculature including, 1 artery and 2 veins, directly abutting deep to the MG branches [
Figure 1:
Intraoperative dissection of the right tibial nerve between the two heads of the gastrocnemius as it provides branches to the medial gastrocnemius (yellow loops). A large vascular bundle was identified directly abutting the medial tibial nerve branches (red loop). Blue loop surrounds the main tibial nerve.
On follow-up at 3 months, his incision had healed without complication, he regained more strength, and his muscle fasciculations had decreased.
DISCUSSION
Mononeuropathies are nerve dysfunctions commonly secondary to local injury such as impingement, mechanical impact, tearing, and/or other constant pressure sources. Tibial neuropathies, in particular, are typically heavily attributed to both impingement and/or injury such as with tarsal tunnel syndrome and entrapment deep to the flexor retinaculum.[
In the presented case, given the significant improvement in fasciculations following the vasculature ligation, the most likely diagnosis following exploration was due to vascular compression of his right MG branches. Contrary to cranial nerves, his presentation was unusual considering the ample space in the popliteal fossa and planes between gastrocnemius heads and underlying soleus muscle. In addition, the normal anatomic variant includes only one MG head and its nerve supply. Yet, our patient not only had multiple MG heads but also a total of three small nerve contributions branching off the tibial nerve. Therefore, there may have been more surface area of nerve to cause abutment and compression to. His previously torn gastrocnemius was likely to cause decreased space between adjacent structures in accommodation for increased swelling as well as adhesions. While the etiology of his anatomic variation remains unclear, it remains feasible that the combination of his anatomy in conjunction with his injury provide a rational mechanism of vascular compression of his MG branch.
Overall, while punched nerve syndrome has been described in the setting of vascular compression of peripheral nerves, this syndrome has largely been described in the setting of ultrasonography. This syndrome was first described in 2012 by Loizides et al. in nine cases of isolated mononeuropathy.[
CONCLUSION
A high level of suspicion is required to identify vascular compression in the setting of a mononeuropathy. With an understanding of the uncommon presentation and location within the popliteal fossa, clinicians should consider the possibility of vascular compression in individuals with a history of localized trauma and lasting associated mononeuropathy. Surgical exploration is worthwhile when the clinical context and EMG findings are compelling, even when the imaging is negative.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Faissner S, Lukas C, Chan A, Gold R, Krogias C. Punched nerve syndrome as contributing factor for Saturday night palsy. J Neurol Sci. 2016. 368: 173-4
2. Falovic R, Nambiar M, Boekel P, Lenaghan J. Varicose veins causing tibial nerve compression in the tarsal tunnel. BMJ Case Rep. 2019. 12: e230072
3. Gruber L, Gruber H, Bauer T, Loizides A. A rare case of a punched nerve syndrome of the deep motor branch of the ulnar nerve. Arch Orthop Trauma Surg. 2015. 135: 891-3
4. Hong CH, Lee YK, Won SH, Lee DW, Moon SI, Kim WJ. Tarsal tunnel syndrome caused by an uncommon ossicle of the talus: A case report. Medicine (Baltimore). 2018. 97: e11008
5. Loizides A, Peer S, Plaikner M, Djurdjevic T, Gruber H. Punched nerve syndrome: Ultrasonographic appearance of functional vascular nerve impairment. Ultraschall Med. 2012. 33: 352-6
6. Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia-diagnosis and treatment. Cephalalgia. 2017. 37: 648-57
7. Tang P, He Q, Chen C, Liu X, Zhang L. Earthquake generated proximal tibial nerve compression treated by surgery. Int Orthop. 2013. 37: 1561-6
8. Yadav YR, Nishtha Y, Sonjjay P, Vijay P, Shailendra R, Yatin K. Trigeminal neuralgia. Asian J Neurosurg. 2017. 12: 585-97