- Department of Neurosurgery, Hospital Universitario Fundación Santa Fé de Bogotá, Bogotá, Cundinamarca, Colombia.
Correspondence Address:
Andrés Segura-Hernández, Department of Neurosurgery, Hospital Universitario Fundación Santa Fé de Bogotá, Bogotá, Cundinamarca, Colombia.
DOI:10.25259/SNI_613_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andrés Segura-Hernández, Fernando Hakim, Juan F. Ramón, Enrique Jiménez-Hakim, Juan A. Mejía-Cordovez, Diego Quintero-Rueda, Yessid Araque-Puello, Camila Pedraza-Ciro, Juan P. Leal-Isaza, Juliana Mendoza-Mantilla, Vanesa Robles, Martina Gonzalez, Daniel Jaramillo-Velásquez, Diego F. Gómez. Ventriculo-atrial shunt. Comparison of an ultrasound-guided peel-away technique versus conventional technique in the management of normal pressure hydrocephalus: A retrospective cohort. 19-Oct-2021;12:531
How to cite this URL: Andrés Segura-Hernández, Fernando Hakim, Juan F. Ramón, Enrique Jiménez-Hakim, Juan A. Mejía-Cordovez, Diego Quintero-Rueda, Yessid Araque-Puello, Camila Pedraza-Ciro, Juan P. Leal-Isaza, Juliana Mendoza-Mantilla, Vanesa Robles, Martina Gonzalez, Daniel Jaramillo-Velásquez, Diego F. Gómez. Ventriculo-atrial shunt. Comparison of an ultrasound-guided peel-away technique versus conventional technique in the management of normal pressure hydrocephalus: A retrospective cohort. 19-Oct-2021;12:531. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11181
Abstract
Background: Normal pressure hydrocephalus (NPH) is a common neurodegenerative syndrome among the elderly characterized by ventriculomegaly and the classic triad of symmetric gait disturbance, cognitive decline and urinary incontinence. To date, the only effective treatment is a cerebrospinal fluid shunting procedure that can either be ventriculo-atrial, ventriculo-peritoneal, or lumbo-peritoneal shunt. The conventional ventriculo-atrial shunt uses venodissection, whereas the peel-away is a percutaneous ultrasound (US)-guided technique that shows some advantages over conventional technique. We sought to compare perioperative complication rates, mean operating time and clinical outcomes for both techniques in NPH patients at our institution.
Methods: A retrospective cohort-type analytical study was conducted, using clinical record data of patients diagnosed with NPH and treated at our center from January 2009 to September 2019. Parameters to be compared include: Perioperative complication rates, intraoperative bleeding, mortality, and mean operating time. Perioperative complication rates are those device-related such as shunt infection, dysfunction, and those associated with the procedure. Complications are further classified in immediate (occurring during the first inpatient stay), early (within the first 30 days of surgery), and late (after day 30 of surgery).
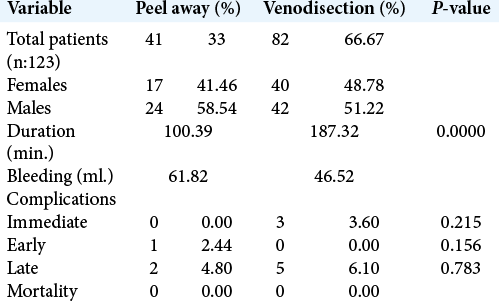
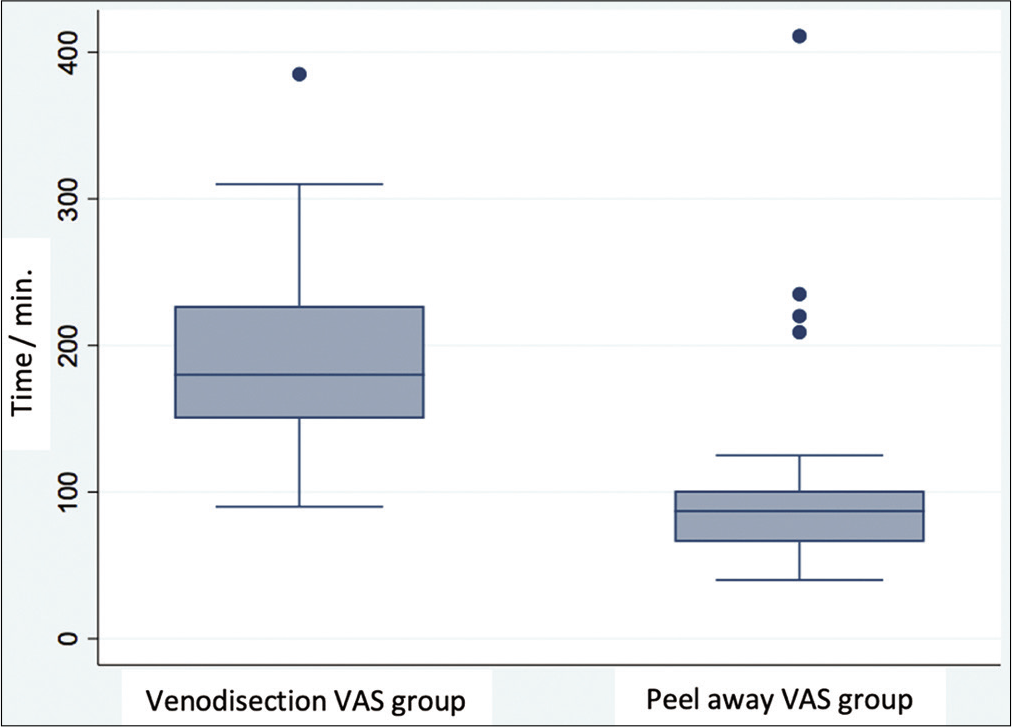
Results: A total of 123 patients underwent ventriculo-atrial shunt. Eighty-two patients (67%) underwent conventional venodissection technique and 41 patients (33%) underwent a peel-away technique. Immediate complications were 3 (3.6%) and 0 for conventional and peel-away groups, respectively. Early complications were 0 and 1 (2.4%) for conventional and peel-away groups, respectively. Late complications were 5 (6.1%) and 2 (4.9%) for conventional and peel-away groups, respectively. Mean operating time was lower in the peel-away group (P = 0.0000) and mortality was 0 for both groups.
Conclusion: Ventriculo-atrial shunt is an effective procedure for patients with NPH. When comparing the conventional venodissection technique with a percutaneous US-guided peel-away technique, the latter offers advantages such as shorter operating time and lower perioperative complication rates.
Keywords: Cerebrospinal fluid, Normal pressure hydrocephalus, Peel-away, Venodissection, Ventriculo-atrial shunt
INTRODUCTION
Normal pressure hydrocephalus syndrome (NPH), first described by Salomón Hakim in 1965, is the most common form of chronic hydrocephalus. NPH is characterized by the paradoxical phenomenon of ventriculomegaly, a classic triad of symmetric gait disturbance, cognitive decline, and urinary incontinence with normal intracranial pressure.[
This peel-away technique has proven to be a precise, rapid, and safe procedure.[
MATERIALS AND METHODS
A retrospective cohort-type analytical study was performed using data from medical records of patients diagnosed with NPH and treated at our institutional NPH center of excellence from January 2009 to September 2019. Patients underwent either conventional VAS or peel-away VAS and perioperative complications, intraoperative bleeding, mean operating time, and mortality were documented to compare outcomes in both groups.
Perioperative complications are classified in immediate (during the first inpatient stay), early (within the first 30 postoperative days), and late (after day 30). Complications are mainly device-related: infection, shunt dysfunction, and surgery-associated mortality.
RESULTS
A total of 123 patients underwent VAS, of these patients, 82 (67%) were operated using a conventional technique and 41 (33%) were operated using a peel-away technique. Immediate complications were reported in three patients (3.6%) and 0 in the conventional and peel-away groups, respectively. Early complications were 0 and 1 (2.4%) for conventional and peel-away groups, respectively. Late complications were 5 (6.1%) and 2 (4.9%) for conventional and peel-away groups, respectively.
Mean operating time was 178.32 and 100.39 min for conventional and peel-away groups, respectively (P = 0.0000). Surgery-associated mortality was 0 for both groups. Regarding intraoperative bleeding, data were not easily obtained because in most records, the term “scant bleeding” was used, possibly representing a potential confounding bias for this parameter. All relevant data are summarized in [
DISCUSSION
Despite the enormous amount of research on NPH, still today the exact etiology of the disorder eludes us. To date, the only effective treatment is a CSF shunting procedure with a success rate ranging from 60% to 80% depending on the series. These differences are mainly due to divergent methodology, diagnostic criteria, selection criteria for shunting procedure, and thresholds for clinical improvement, hence is important diagnose those patients who benefit from a shunt device. CSF shunting has proven to improve at least one of the classic triad components in most patients. Some authors report subjective improvement in 96% of cases with objective improvement in gait tests in 83% of cases.[
VAS was originally described by Nulsen and Spitz in 1952 and later improved by Hakim due to a physiological rationale. VPS was described by Scott in 1955.[
VPS is the most common technique, but incidence of peritoneal cavity complications range from 5% to 47% and VPS is contraindicated in certain patients (infection, neoplasm or recurrent idiopathic ascites, and among others).[
With the advent of Seldinger-type percutaneous techniques, perioperative complications and mean operating time are significantly reduced.[
In 2006, Słowiński et al. reported a series of 169 patients followed during 64 months. Among intraoperative complications, they report: carotid artery puncture (5%) and pneumothorax (3.3%). Complications during the first 6 postoperative months include: surgical site infection (3.3%), distal catheter malposition (5%), and catheter disconnection (1.7%). Late complications included: distal catheter infection (3.3%), occlusion (6.7%), and disconnection (1.7%).[
It is accepted that when choosing VAS, a US-guided peel-away technique with constant cardiac monitoring should be used and distal catheter position should be confirmed with fluoroscopy.[
In our cohort, perioperative complications and operating times were lower in the peel-away group. Only one patient from the peel-away group had an early complication versus 0 in the conventional group. This patient developed bacterial meningitis which was optimally treated without any further complications and has no relation with the type of technique but probably with flawed antisepsis during the procedure. Surgery-associated mortality was 0 for both groups. This cohort proves once again that peel-away technique is a safe method with low complication rates (comparable to that reported previously in the literature) and that is a viable option for patients that cannot undergo a VPS. All the available data warrant a randomized controlled trial to evaluate both procedures and eventually examine superiority or at least non-inferiority. For the time being, VAS remains an excellent treatment of choice for patients with NPH in experienced hands.
CONCLUSION
VAS using a Seldinger-type US-guided technique with a disposable sheathed peel-away vascular catheter under constant electrocardiographic monitoring and confirming distal catheter position with fluoroscopy, is a procedure that offers advantages like shorter operating time and lower perioperative complication rates for patients with NPH.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adams RD, Fisher CM, Hakim S, Ojemann RG, Sweet WH. Symptomatic occult hydrocephalus with normal cerebrospinal-fluid pressure. N Engl J Med. 1965. 273: 117-26
2. Al-Schameri AR, Hamed J, Baltsavias G, Winkler P, Machegger L, Richling B. Ventriculoatrial shunts in adults, incidence of infection, and significant risk factors: A single-center experience. World Neurosurg. 2016. 94: 345-51
3. Ashker K, Fox JL. Percutaneous technique for insertion of an atrial catheter for CSF shunting. J Neurosurg. 1981. 55: 488-90
4. Bates P, Rajderkar D. Common and uncommon causes of ventriculoperitoneal shunt malfunction diagnosed on plain radiographs. Curr Probl Diagn Radiol. 2017. 47: 317-23
5. Carol M, Robinson W, Harris BS. Percutaneous placement of ventriculoatrial shunts: Four-year case experience. Neurosurgery. 1986. 18: 348-9
6. Decq P, Blanquet A, Yepes C. Percutaneous jugular placement of ventriculo-atrial shunts using a split sheath. Acta Neurochir (Wien). 1995. 136: 92-4
7. Della Pepa GM, Sabatino G, Peppucci E, Sturiale CL, Albanese A, Puca A. Electrocardiographic-guided technique for placement of ventriculoatrial shunts: A valid and cost-effective technical simplification. World Neurosurg. 2018. 109: 455-9
8. Ellegaard L, Mogensen S, Juhler M. Ultrasound-guided percutaneous placement of ventriculoatrial shunts. Childs Nerv Syst. 2007. 23: 857-62
9. Gmeiner M, Wagner H, van Ouwerkerk WJ, Sardi G, Thomae W, Senker W. Long-term outcomes in ventriculoatrial shunt surgery in patients with pediatric hydrocephalus: Retrospective single-center study. World Neurosurg. 2020. 138: e112-8
10. Halperin JJ, Kurlan R, Schwalb JM, Cusimano MD, Gronseth G, Gloss D. Practice guideline: Idiopathic normal pressure hydrocephalus: Response to shunting and predictors of response: Report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology. 2015. 85: 2063-71
11. Hung AL, Vivas-Buitrago T, Adam A, Lu J, Robison J, Elder BD. Ventriculoatrial versus ventriculoperitoneal shunt complications in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg. 2017. 157: 1-6
12. Huppert J, Bret P, Fischer G. Percutaneous insertion of the cardiac catheter in ventriculo-atrial shunt. Neurochirurgie. 1984. 30: 135-7
13. Ignelzi RJ, Kirsch WM. Follow-up analysis of ventriculoperitoneal and ventriculoatrial shunts for hydrocephalus. J Neurosurg. 1975. 42: 679-82
14. Keucher TR, Mealey J. Long-term results after ventriculoatrial and ventriculoperitoneal shunting for infantile hydrocephalus. J Neurosurg. 1979. 50: 179-86
15. Kim YH, Lee SW, Kim DH, Lee CH, Kim CH, Sung SK. Case series of ventriculoatrial shunt placement in hybrid room: Reassessment of ventriculoatrial shunt. Korean J Neurotrauma. 2020. 16: 181-9
16. Kock-Jensen C, Clemmensen S, Andersen BB. Percutaneous insertion of CSF ventriculoatrial shunts-a new technique. Acta Neurochir (Wien). 1989. 96: 76-9
17. Lam CH, Villemure JG. Comparison between ventriculoatrial and ventriculoperitoneal shunting in the adult population. Br J Neurosurg. 1997. 11: 43-8
18. Merkler AE, Ch J, Parker WE, Murthy SB, Kamel H. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017. 98: 654-8
19. Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H.editors. Guidelines for management of idiopathic normal pressure hydrocephalus (Third Edition): Endorsed by the Japanese society of normal pressure hydrocephalus. Neurol Med Chir (Tokyo). 2021. 61: 63-97
20. Nowosławska E, Moszura T, Mikołajczyk-Wieczorek W, Zakrzewski K, Krawczyk J, Szymański W. Ahybrid technique for ventriculoatrial shunt implantation-technical note. Childs Nerv Syst. 2014. 30: 1729-32
21. Pascual JM, Prakash UB. Development of pulmonary hypertension after placement of a ventriculoatrial shunt. Mayo Clin Proc. 1993. 68: 1177-82
22. Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2013. 81: 404-10
23. Słowiński J, Stomal M, Skaba T, Pieniazek J, Mrówka M. Percutaneous ventriculoatrial shunt: Experience with 179 cases. Neurol Neurochir Pol. 2006. 40: 198-202
24. Sribnick EA, Sklar FH, Wrubel DM. A novel technique for distal shunt revision: Retrospective analysis of guidewire-assisted distal catheter replacement. Neurosurgery. 2015. 11: 367-70
25. Symss NP, Oi S. Is there an ideal shunt? A panoramic view of 110 years in CSF diversions and shunt systems used for the treatment of hydrocephalus: From historical events to current trends. Childs Nerv Syst. 2015. 31: 191-202