- Department of Neurosurgery, Klinikum Bayreuth GmbH, Betriebsstätte Hohe Warte, Bayreuth, Germany.
Correspondence Address:
Thomas Reithmeier, Department of Neurosurgery, Klinikum Bayreuth GmbH, Betriebsstätte Hohe Warte, Bayreuth, Germany.
DOI:10.25259/SNI_503_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Dounia Hmimidi, Shafie Ariai, Thomas Reithmeier. Ventriculoperitoneal shunt failure due to raised intra-abdominal pressure: A case report and review of the literature. 30-Sep-2022;13:440
How to cite this URL: Dounia Hmimidi, Shafie Ariai, Thomas Reithmeier. Ventriculoperitoneal shunt failure due to raised intra-abdominal pressure: A case report and review of the literature. 30-Sep-2022;13:440. Available from: https://surgicalneurologyint.com/surgicalint-articles/11911/
Abstract
Background: Ventriculoperitoneal (VP) shunt implantation is the standard neurosurgical procedure to treat hydrocephalus for various reasons. Its function depends on the differential pressure between the ventricular space and the peritoneal cavity. Correct functioning of cerebrospinal fluid (CSF) valves requires a gradient of pressure between the ventricular and the abdominal cavity. Any reason that disrupts this balance can result in dysfunction of the system. Increased intra-abdominal pressure (IAP) may be a reason to induce shunt failure by decreasing CSF drainage from the ventricular system to the peritoneal cavity.
Case Description: We report a case of repeated VP shunt failure because of constipation and successful conservative management by lowering IAP without surgical revision of the VP shunt system and reviewed the relevant literature.
Conclusion: Increased IAP for a variety of reason should always be considered as a possible reason for shunt failure that can often be treated conservatively and therefore can reduce unnecessary shunt revision surgery.
Keywords: Abdominal surgery, Constipation, Intra-abdominal pressure, Ventriculoperitoneal shunt dysfunction
INTRODUCTION
A malfunctioning ventriculoperitoneal (VP) shunt was always a challenging for neurosurgeons and mostly resulting from obstruction, infection, or disconnection. In this article, we discussed a case of repeated VP shunt (VPS) failure because of constipation as uncommon etiology of VPS failure and reviewed the relevant literature.
CASE REPORT
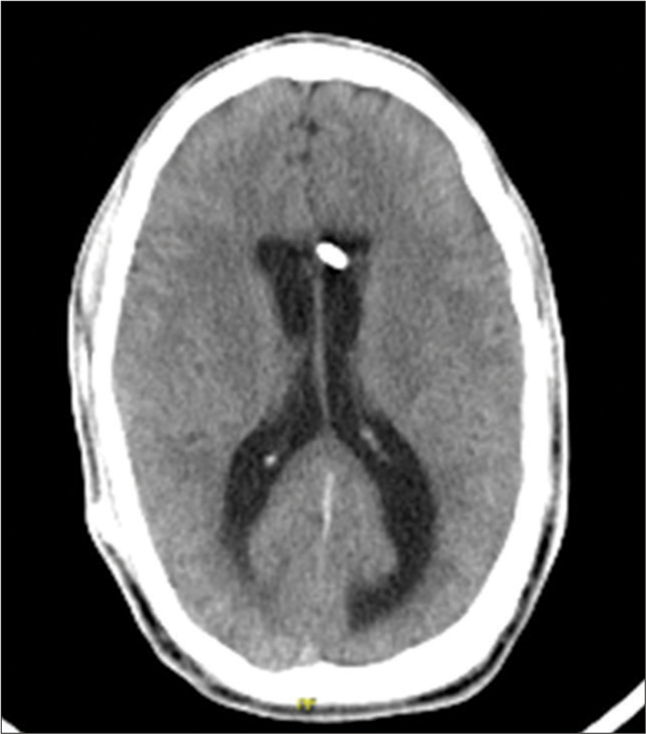
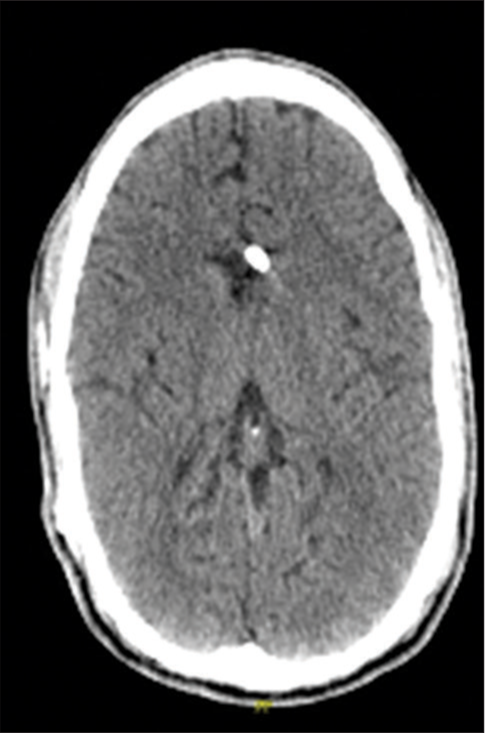
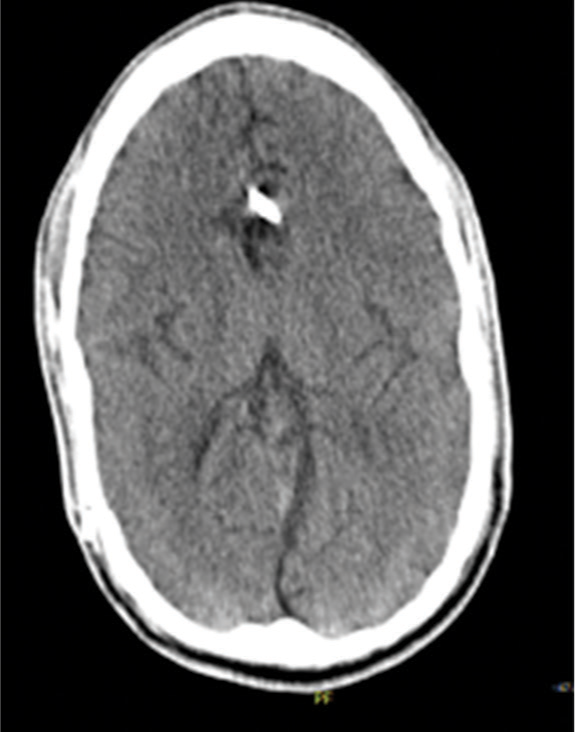
A 29-year-old man, in whom a VPS had been inserted at the age of 4 months to treat congenital hydrocephalus, presented in our clinic with altered state of consciousness and gait apraxia. The patient did not report other symptoms typical for raised intracranial pressure or shunt infection such as nausea, vomiting, meningism, or fever. His routine laboratory investigation was normal. Emergency computerized tomography (CT) of the head revealed a hydrocephalic ventricular system, suggesting a functional VPS failure [
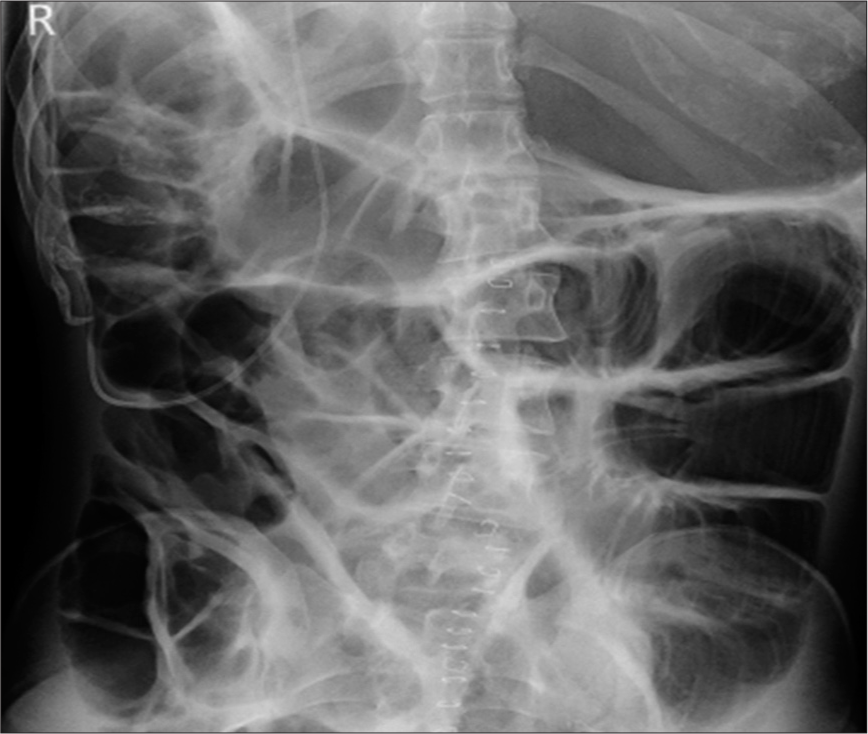
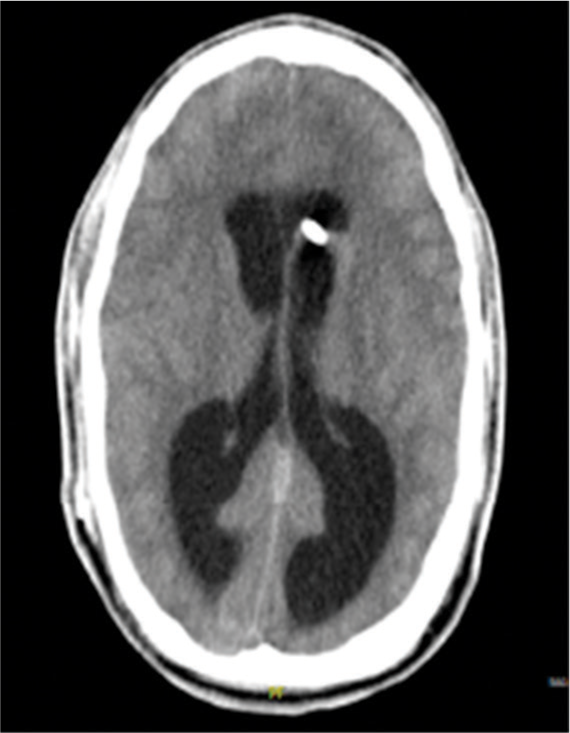
Further evaluation of the medical history of the patient revealed a similar situation in 2017. The patient underwent ileus surgery and was admitted to our hospital with suspected meningitis because of fever and alteration of consciousness 2 days after. The patient was immediately transferred to the intensive care unit and endotracheal intubation was required. A spinal tap was ensued, thereby excluding meningitis. A CT of the head showed an advanced hydrocephalus [
DISCUSSION
At present, the treatment of choice for most patients with hydrocephalus is a VPS placement. Unfortunately, the rate of complications after VPS surgery is high. The most common causes of shunt failure in both pediatric and adult populations are shunt obstruction followed by infection.[
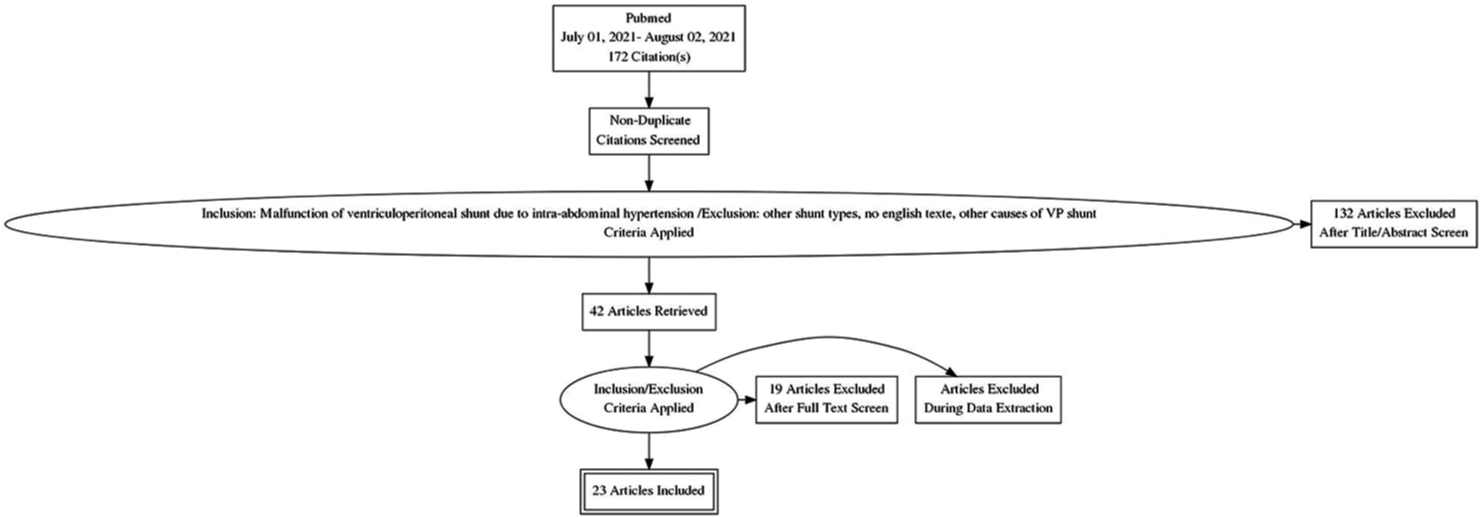
Therefore, we performed a systematically literature review for case reports and reasons of increased IAP leading to VPS dysfunction according to the PRISMA framework [
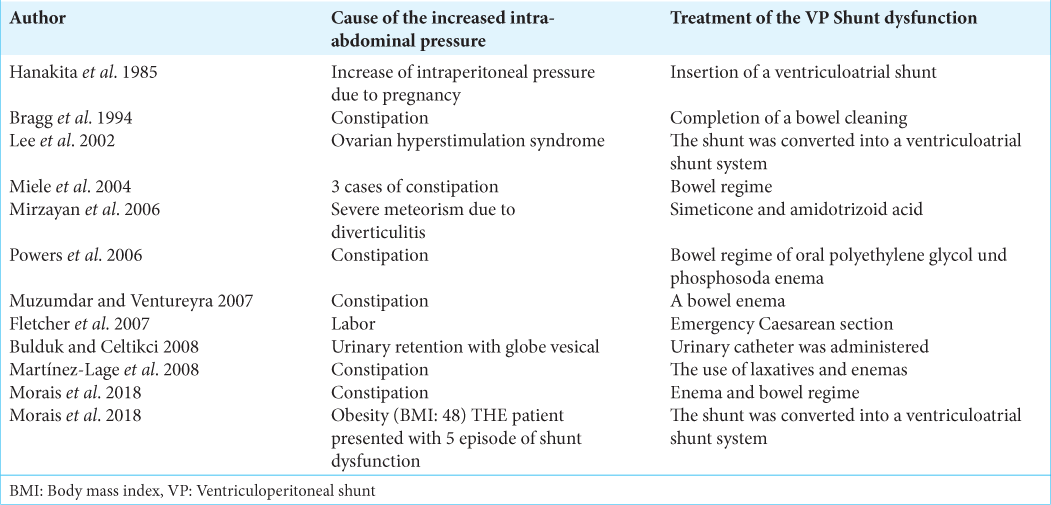
Actually, constipation is an unusual cause of VPS failure and was first described by Bragg in 1994.[
However, our literature research revealed several additional reasons of raised IAP, leading to VPS failure.
Already in 1985, Hanakita et al. described a malfunction of a VPS in a 25-year-old woman at 32 weeks of gestation induced by increase of intra-peritoneal pressure due to pregnancy and the VPS system had to be converted into a ventriculoatrial shunt system.[
In 2006, Mirzayan et al. described a patient with exacerbation of a previously shunted hydrocephalus due to meteorism which was conservatively treated by simethicone and amidotrizoic acid for meteorism and constipation.[
In an obstetrical case report, published by Fletcher et al. in 2007, labor was identified as the cause of VPS malfunction. A shunted parturient had an uneventful pregnancy until the 36th week when she presented to the labor ward with drowsiness and decreasing consciousness. The reason was acute shunt malfunction due to increased IAP and the patient recovered after emergency caesarean section.[
Another rare case of VPS dysfunction in a pediatric patient caused by urinary retention was reported by Bulduk and Celtikci. in 2008.[
Moreover, obesity is considered an important factor of an inadequate function of VPSs. In obese individuals, the IAP reaches values between 8 and 12 mmHg. Morais et al. reported in 2018 repeated VPS malfunction in a 16-year-old girl with a body mass index of 48. Revision operations did not show any evidence of malfunction. Ultimately, the VPS was converted into a ventriculoatrial shunt system.[
Besides this physical aspect of VPS dysfunction focusing on changes in the differential pressure, various other factors are described in the literature how intra-abdominal pathologies can influence shunt function. Hypothetically, a stool or a huge bowel loop could mechanically occlude the peritoneal end of the VPS. In addition, increasing intra-peritoneal and IAP decreases the resorptive ability of the peritoneum for CSF.[
CONCLUSION
While evaluating a shunt dysfunction, not only shunt dependent factors but also abdominal related problems must be considered with the goal to minimize unnecessary shunt revisions. We, therefore, recommend that patients with a VPS and the need for an abdominal surgery should be treated in a hospital with an additional neurosurgical department.
STATEMENT OF ETHICS
Study approval statement
Ethical approval was not required for this study according to paragraph 15 of the code of the professional conduct for Bavarian doctors: Mrs Sanja Fricke, head of the office, Ethics committee (Bayerische Landesärztekammer, Munich).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bragg CL, Edwards-Beckett J, Eckle N, Principe K, Terry D. Ventriculoperitoneal shunt dysfunction and constipation: A chart review. J Neurosci Nurs. 1994. 26: 265-9
2. Bulduk EB, Celtikci E. Intraabdominal pressure: Is it a cause of shunt dysfunction? A pediatric case reports. GMJ. 2018. 29: 69-71
3. Burks JD, Conner AK, Briggs RG, Glenn CA, Bonney PA, Cheema AA. Risk of failure in pediatric ventriculoperitoneal shunts placed after abdominal surgery. J Neurosurg Pediatr. 2017. 19: 571-7
4. Fletcher H, Crandon IW, Webster D. Maternal hydrocephalus in pregnancy and delivery: A report of two cases. West Indian Med J. 2007. 56: 558-9
5. Hanakita J, Suzuki T, Yamamoto Y, Linuta Y, Nishihara K. Ventriculoperitoneal shunt malfunction during pregnancy. J Neurosurg. 1985. 63: 459-60
6. Lee GY, Daniel RT, Jones NR. Ventriculoperitoneal shunt failure as a secondary complication of ovarian hyperstimulation syndrome. J Neurosurg. 2002. 97: 992-4
7. Martínez-Lage JF, Martos-Tello JM, Ros-de-San Pedro J, Almagro MJ. Severe constipation: An under-appreciated cause of VP shunt malfunction: A case-based update. Childs Nerv Syst. 2008. 24: 431-5
8. Miele VJ, Bendok B, Bloomfield SM, Ondra SL, Bailes JE. Ventriculoperitoneal shunt dysfunction in adults secondary to conditions causing a transient increase in intra-abdominal pressure: Report of three cases. Neurosurgery. 2004. 55: E444-8
9. Mirzayan MJ, Koenig K, Bastuerk M, Krauss JK. Coma due to meteorism and increased intra-abdominal pressure subsequent to ventriculoperitoneal shunt dysfunction. Lancet. 2006. 368: 2032
10. Morais BA, Cardeal DD, Andrade FG, Paiva WS, Matushita H, Teixeira MJ. Reversible ventriculoperitoneal shunt dysfunction and chronic constipation: Case report. J Neurosurg Pediatr. 2018. 22: 147-50
11. Morais BA, Yamaki VN, Cardeal DD, Andrade FG, Paiva WS, Matushita H. High intra-abdominal pressure secondary to obesity as a determining factor for ventriculoperitoneal shunt malfunction. Arq Bras Neurocir. 2018. 37: 50-3
12. Muzumdar D, Ventureyra EC. Transient ventriculoperitoneal shunt malfunction after chronic constipation: Case report and review of literature. Childs Nerv Syst. 2007. 23: 455-8
13. Paff M, Alexandru-Abrams D, Muhonen M, Loudon W. Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg. 2018. 13: 66-70
14. Powers CJ, George T, Fuchs HE. Constipation as a reversible cause of ventriculoperitoneal shunt failure. Report of two cases. J Neurosurg. 2006. 105: 227-30