- Department of Radiology, Beaumont Hospital, Dublin 9, Ireland
- Department of Neurosurgery, Royal College of Surgeons in Ireland, Dublin 2, Ireland
- Department of Surgery, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Correspondence Address:
Conor Brosnan, Department of Radiology, Beaumont Hospital, Dublin, Ireland.
DOI:10.25259/SNI_293_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Conor Brosnan1, Mohamed Osman Dablouk2,3, Vincent Healy2,3, Daniel Murray2,3, Hamzah A. Soleiman2, Ciaran Bolger2,3. When does too little pressure become too much? A case of spontaneous intracranial hypotension presenting with acute loss of consciousness. 15-Sep-2023;14:338
How to cite this URL: Conor Brosnan1, Mohamed Osman Dablouk2,3, Vincent Healy2,3, Daniel Murray2,3, Hamzah A. Soleiman2, Ciaran Bolger2,3. When does too little pressure become too much? A case of spontaneous intracranial hypotension presenting with acute loss of consciousness. 15-Sep-2023;14:338. Available from: https://surgicalneurologyint.com/surgicalint-articles/12549/
Abstract
Background: We present a unique case of spontaneous intracranial hypotension (SIH) presenting with acute collapse and loss of consciousness.
Case Description: The affected patient suffered an abrupt decline in level of consciousness several weeks after initial diagnosis. The patient was urgently transferred to a specialist neurosurgical unit. Imaging showed bilateral subdural fluid collections with significant associated local mass effect. The treating team faced a clinical conundrum with a lack of clarity as to whether this sudden deterioration was secondary to the local pressure effect on brainstem traction from reduced intracranial pressure. A decision was made to proceed with urgent burr-hole decompression of the bilateral subdural fluid collections.
Conclusion: After a protracted, complex postoperative course, the patient recovered to full functional independence. To the author’s knowledge, this is the first case in literature describing successful surgical management of SIH, with bilateral burr-hole evacuation to relieve the paradoxical mass effect of bilateral subdural fluid collections.
Keywords: Cerebrospinal fluid effusion, Essential intracranial hypotension, Neurosurgery, Spontaneous subdural surgical management
INTRODUCTION
Spontaneous intracranial hypotension (SIH) is characterized by postural headache, often secondary to an underlying idiopathic spinal cerebrospinal fluid (CSF) leak, resulting in reduced intracranial pressure. It has an estimated annual incidence of 5/100,000 of the population.[
Management of SIH is usually conservative, with hydration and bed rest. Further, intervention by means of an epidural blood patch may be pursued following failed conservative management. Surgical intervention is rarely performed. Repair of dural defects or CSF venous fistulae has been described but is exceedingly rare.[
We report a case of SIH presenting with acute collapse and loss of consciousness. There are no published reports of SIH presenting with acute deterioration and coma managed with urgent decompressive surgery. This case presents a unique diagnostic dilemma, with uncertainty as to whether a drop in Glasgow Coma Score (GCS) was due to brainstem herniation through the foramen magnum secondary to low intracranial pressure or a result of the mass effect of subdural fluid collections on the cerebrum. A decision was made to urgently evacuate the fluid collections. The patient made a complete recovery following the intervention.
CASE HISTORY
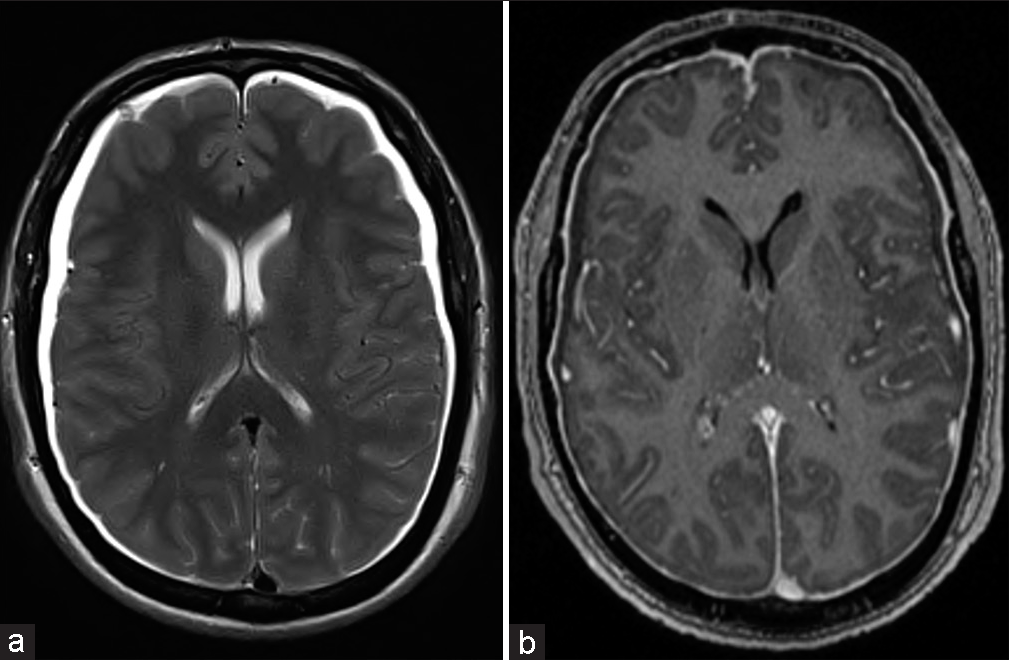
A 48-year-old right-hand dominant male presented to a local emergency department with a 6-week history of headaches and ataxia which began after weightlifting. Headaches were described as intermittent and worse with standing. Background history was unremarkable with no comorbidities, prior surgery, or recent trauma. Following admission, routine hematological tests were unremarkable. Work-up also included computed tomography (CT) brain and magnetic resonance imaging (MRI) of the brain with contrast. Imaging revealed bilateral hypoattenuating subdural collections with associated bifrontal sulcal effacement on CT [
Several weeks later, the patient was found collapsed at home. He was difficult to rouse and was brought by ambulance to a local hospital. A GCS of 14 was recorded on arrival. This subsequently dropped to 10. An urgent CT brain exhibited enlarging subdural fluid collections, particularly on the right [
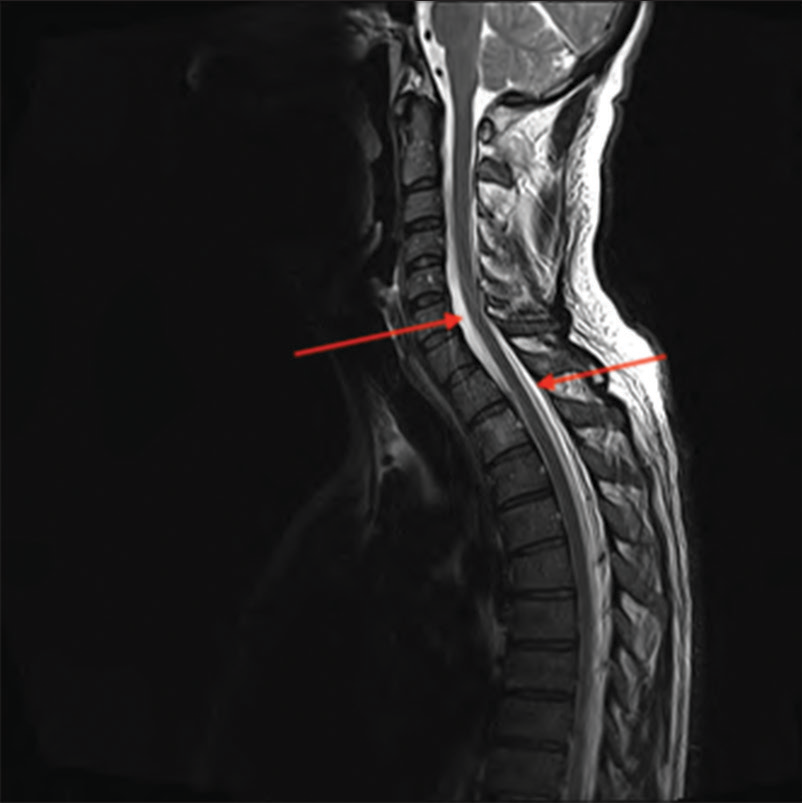
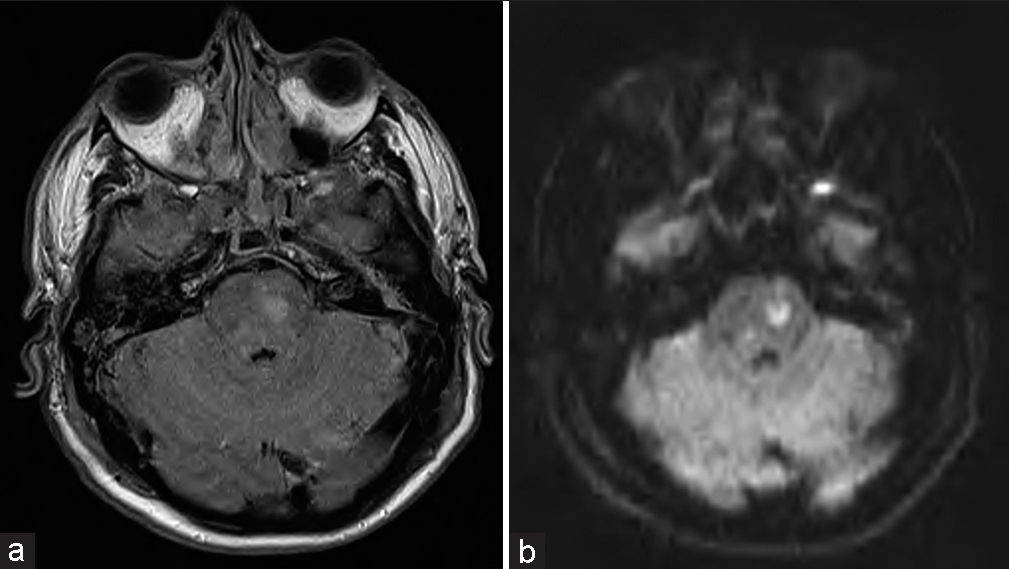
A complex postoperative course followed. The neurosurgical team advocated for the patient to be nursed in the Trendelenburg position. However, the patient was often managed in a head up position for the management of respiratory problems. A blood patch performed to seal a hypothesized leak at the cervicothoracic spine yielded no clinical improvement 4 days after surgery. Spinal epidural fluid collections remained stable on MRI. GCS remained low; however, the patient began flexing in response to pain with severe right-sided weakness. An up-to-date MRI brain [
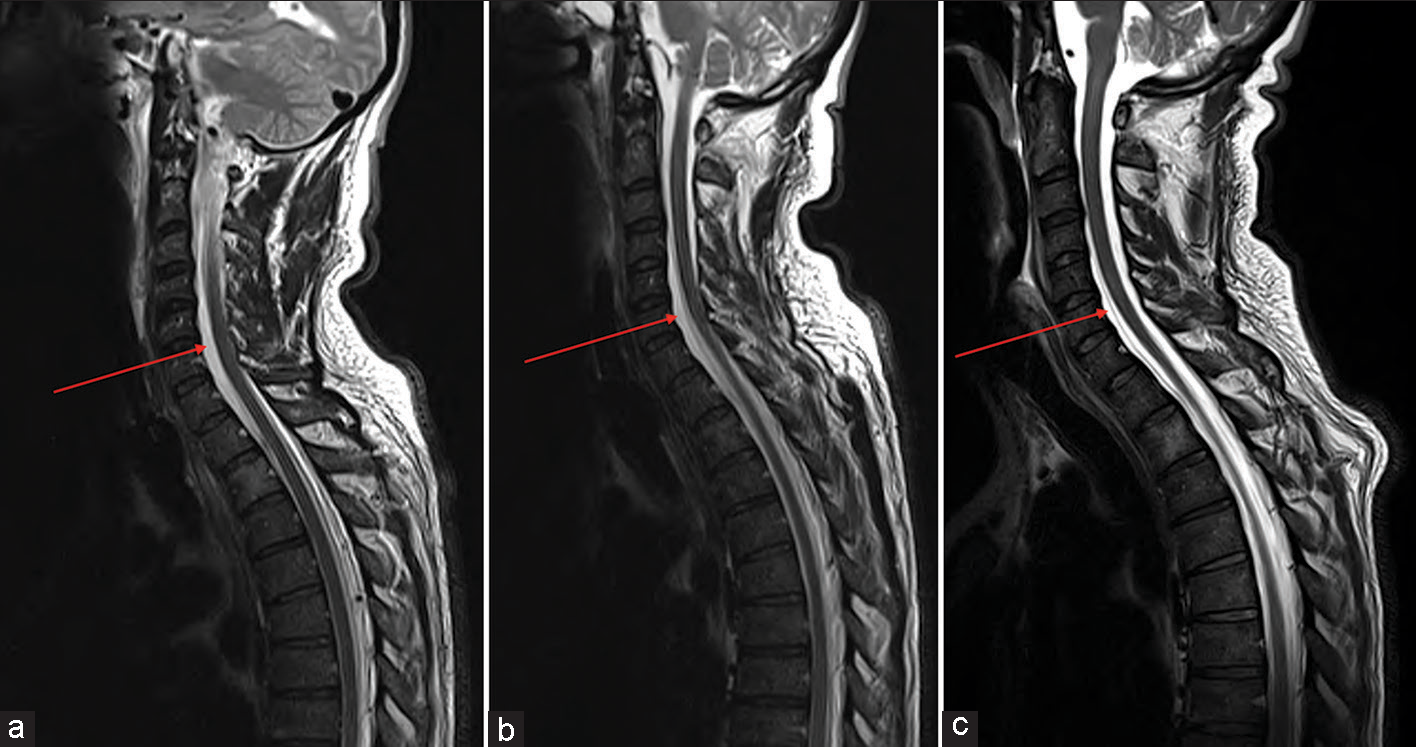
Despite the grim prognosis, a repeat blood patch was performed 2 weeks after the first. The patient was strictly nursed in a continuous Trendelenburg position following this. This yielded encouraging results, and GCS rose to 14 with successful extubation 2 days later. The cervicothoracic epidural fluid collections gradually reduced in volume over serial MRI [
At follow-up 2 months post discharge, the patient was fully independent with only a partial right trochlear nerve palsy and mild right-sided paresthesias, having regained full power on both sides.
DISCUSSION
SIH is uncommonly encountered. It has an estimated annual incidence of 5/100,000.[
Our case has a distinct course. Acute collapse confounded the clinical picture and presented a unique challenge in deciding the most appropriate management. While the patient had known SIH, it was impossible to determine whether the rapid deterioration was secondary to brainstem herniation through the foramen magnum from sagging related to low intracranial pressure or due to the mass effect of subdural fluid collections on the cerebrum and subsequent coning. Given the sudden acute decline and considerable increase in the size of the bifrontal subdural fluid collections, a decision for urgent bilateral burr-hole decompression was made. While several cases of SIH presenting with coma have been described,[
CONCLUSION
After a long, protracted and complex postoperative course, the patient recovered to full functional independence. To the author’s knowledge, this is the first case in literature describing successful surgical management of SIH, with bilateral burr-hole evacuation to relieve the paradoxical mass effect of bilateral subdural fluid collections.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Capizzano AA, Lai L, Kim J, Rizzo M, Gray L, Smoot MK. Atypical presentations of intracranial hypotension: Comparison with classic spontaneous intracranial hypotension. AJNR Am J Neuroradiol. 2016. 37: 1256-61
2. Chen YC, Wang YF, Li JY, Chen SP, Lirng JF, Hseu SS. Treatment and prognosis of subdural hematoma in patients with spontaneous intracranial hypotension. Cephalalgia. 2016. 36: 225-31
3. D’Antona L, Merchan MA, Vassiliou A, Watkins LD, Davagnanam I, Toma AK. Clinical presentation, investigation findings, and treatment outcomes of spontaneous intracranial hypotension syndrome: A systematic review and meta-analysis. JAMA Neurol. 2021. 78: 329-37
4. Ganau L, Prisco L, Ganau M. High altitude induced bilateral non-traumatic subdural hematoma. Aviat Space Environ Med. 2012. 83: 899-901
5. Kwok JM, Mandell DM, Margolin EA. Papilledema in a patient with intracranial hypotension. J Neuroophthalmol. 2021. 41: e708-10
6. Lin WC, Lirng JF, Fuh JL, Wang SJ, Chang FC, Ho CF. MR findings of spontaneous intracranial hypotension. Acta Radiol. 2002. 43: 249-55
7. Liu YF, Lin HL, Cho DY, Chen CC, Lo YC, Chiou SM. Burr hole drainage for complicated spontaneous intracranial hypotension syndrome. Kaohsiung J Med Sci. 2008. 24: 498-502
8. Loya JJ, Mindea SA, Yu H, Venkatasubramanian C, Chang SD, Burns TC. Intracranial hypotension producing reversible coma: A systematic review, including three new cases. J Neurosurg. 2012. 117: 615-28
9. Schievink WI, Maya MM, Louy C, Moser FG, Tourje J. Diagnostic criteria for spontaneous spinal CSF leaks and intracranial hypotension. AJNR Am J Neuroradiol. 2008. 29: 853-6
10. Schievink WI, Maya MM, Moser F, Tourje J, Torbati S. Frequency of spontaneous intracranial hypotension in the emergency department. J Headache Pain. 2007. 8: 325-8