- Department of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India.
DOI:10.25259/SNI_339_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ravi Sharma, Sachin A. Borkar, Revanth Goda, Shashank S. Kale. Which factors predict the loss of cervical lordosis following cervical laminoplasty? A review of various indices and their clinical implications. 26-Jul-2019;10:147
How to cite this URL: Ravi Sharma, Sachin A. Borkar, Revanth Goda, Shashank S. Kale. Which factors predict the loss of cervical lordosis following cervical laminoplasty? A review of various indices and their clinical implications. 26-Jul-2019;10:147. Available from: http://surgicalneurologyint.com/surgicalint-articles/9530/
Abstract
Background: Many patients undergoing laminoplasty develop postoperative loss of cervical lordosis or kyphotic alignment of cervical spine despite sufficient preoperative lordosis. This results in poor surgical outcomes.
Methods: Here, we reviewed the relationship between multiple radiological parameters of cervical alignment that correlated with postoperative loss of cervical lordosis in patients undergoing laminoplasty.
Results: Patient with a high T1 slope (T1S) has more lordotic alignment of the cervical spine preoperatively and is at increased risk for the loss of cervical lordosis postlaminoplasty. Those with lower values of difference between T1S and Cobb’s angle (T1S-CL) and CL-T1S ratio have higher risks of developing a loss of the cervical lordosis postoperatively. Alternatively, C2-C7 lordosis, neck tilt, cervical range of motion, and thoracic kyphosis had no role in predicting the postlaminoplasty kyphosis.
Conclusion: Among various radiological parameters, the preoperative T1S is the most important factor in predicting the postoperative loss of the cervical lordosis/alignment following laminoplasty.
Keywords: Cervical laminoplasty, Loss of cervical lordosis, T1 slope, C2-C7 lordosis, C2-C7 Cobb’s angle, C2-C7 sagittal vertical axis, C2-C3 disc angle
INTRODUCTION
Although laminectomy has better long-term clinical and radiological outcomes, laminoplasty is still favored for the management of cervical spondylotic myelopathy as it preserves the cervical range of motion (ROM) with a lower risk of postoperative kyphosis.[
METHODS
Measures of cervical alignment
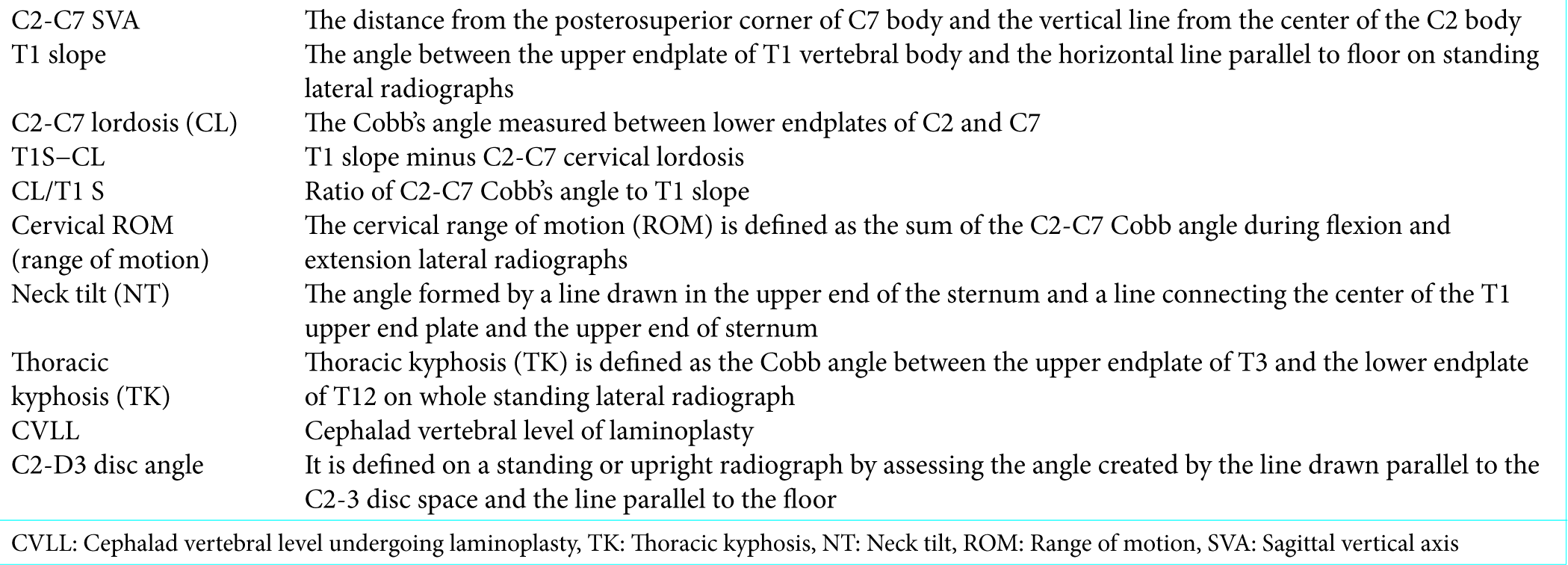
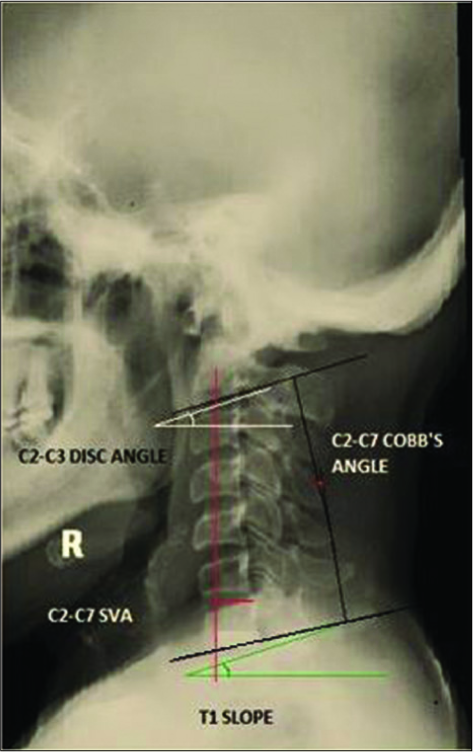
Multiple studies have described various indices that help predict the risk of loss of cervical lordosis in postlaminoplasty patients [
RESULTS
T1S
The T1S is one of the most important indices that can help predict the postlaminoplasty loss of cervical lordosis. Notably, the preoperative cervical lordosis (C2-C7 Cobb’s angle) was greater in patients with higher T1S versus those with lower T1S; these patients have a higher risk of kyphosis postlaminoplasty.[
C2-C7 sagittal vertical axis (SVA)
Several studies have shown that the preoperative C2-C7 SVA had no significant correlation with the postlaminoplasty loss of cervical lordosis.[
Other factors are predictive of postlaminoplasty kyphosis
There are multiple other factors that predict postlaminoplasty kyphosis. Li et al.[
CONCLUSION
A high T1S and C2-C7 SVA are the most predictive factors for postlaminoplasty kyphosis. Those risk factors that do not contribute to this include; (1) the preoperative C2-C7 lordosis, NT, cervical ROM, and TK.
References
1. Baba H, Uchida K, Maezawa Y, Furusawa N, Azuchi M, Imura S. Lordotic alignment and posterior migration of the spinal cord following en bloc open-door laminoplasty for cervical myelopathy: A magnetic resonance imaging study. J Neurol. 1996. 243: 626-32
2. Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty?. Spine (Phila Pa 1976). 2014. 39: E1575-81
3. Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Nakamura H, Kimura T. Minimum 10-year followup after en bloc cervical laminoplasty. Clin Orthop Relat Res. 2003. 411: 129-39
4. Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T. Myoarchitectonic spinolaminoplasty: Efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine. 2007. 7: 293-304
5. Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 2013. 38: E992-7
6. Kim B, Yoon DH, Ha Y, Yi S, Shin DA, Lee CK. Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J. 2016. 16: 219-25
7. Kretzer RM, Hsu W, Hu N, Umekoji H, Jallo GI, McAfee PC. Adjacent-level range of motion and intradiscal pressure after posterior cervical decompression and fixation: An in vitro human cadaveric model. Spine (Phila Pa 1976). 2012. 37: E778-85
8. Lee SH, Son ES, Seo EM, Suk KS, Kim KT. Factors determining cervical spine sagittal balance in asymptomatic adults: Correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015. 15: 705-12
9. Lee SH, Lee JS, Sung SK, Son DW, Lee SW, Song GS. A lower T1 slope as a predictor of subsidence in anterior cervical discectomy and fusion with stand-alone cages. J Korean Neurosurg Soc. 2017. 60: 567-76
10. Lee BS, Walsh KM, Lubelski D, Knusel KD, Steinmetz MP, Mroz TE. The effect of C2-3 disc angle on postoperative adverse events in cervical spondylotic myelopathy. J Neurosurg Spine. 2018. 30: 38-45
11. Li XY, Kong C, Sun XY, Guo MC, Ding JZ, Yang YM. Influence of the ratio of C2-C7 cobb angle to T1 slope on cervical alignment after laminoplasty. World Neurosurg. 2019. 124: e659-66
12. Lin S, Zhou F, Sun Y, Chen Z, Zhang F, Pan S. The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J. 2015. 24: 127-35
13. Lin BJ, Hong KT, Lin C, Chung TT, Tang CT, Hueng DY. Impact of global spine balance and cervical regional alignment on determination of postoperative cervical alignment after laminoplasty. Medicine (Baltimore). 2018. 97: e13111-
14. Matsunaga S, Sakou T, Nakanisi K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord. 1999. 37: 20-4
15. Ratliff JK, Cooper PR. Cervical laminoplasty: A critical review. J Neurosurg. 2003. 98: 230-8
16. Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 2001. 26: 479-87
17. van Geest S, de Vormer AM, Arts MP, Peul WC, Vleggeert-Lankamp CL. Long-term follow-up of clinical and radiological outcome after cervical laminectomy. Eur Spine J. 2015. 24: 229-35
18. Zhang JT, Li JQ, Niu RJ, Liu Z, Tong T, Shen Y. Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J. 2017. 26: 1205-10