- Department of Surgery, Medical college, King Faisal University, Al-Ahsa, Saudi Arabia
- Department of Surgery, King Fahad University, Al-Ahsa, Saudi Arabia
- Research Center, Almoosa Health Group, Al-Ahsa, Saudi Arabia
Correspondence Address:
Abdulsalam Mohammed Aleid, Department of Surgery, King Faisal University, Al-Ahsa, Saudi Arabia.
DOI:10.25259/SNI_652_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulsalam Mohammed Aleid1, Saud Nayef Aldanyowi1, Ayat J. Aleid1, Awn Abdulmohsen Alessa2, Abdulmonem Ali Alhussain2, Loai Saleh Albinsaad1, Abbas Saleh Al Mutair3. Which is better in the management of chronic subdural hematoma: Irrigation, or no irrigation? A systematic review and meta-analysis of randomized controlled trials. 29-Nov-2024;15:435
How to cite this URL: Abdulsalam Mohammed Aleid1, Saud Nayef Aldanyowi1, Ayat J. Aleid1, Awn Abdulmohsen Alessa2, Abdulmonem Ali Alhussain2, Loai Saleh Albinsaad1, Abbas Saleh Al Mutair3. Which is better in the management of chronic subdural hematoma: Irrigation, or no irrigation? A systematic review and meta-analysis of randomized controlled trials. 29-Nov-2024;15:435. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13263
Abstract
Background: Chronic subdural hematoma (CSDH) is a prevalent neurological disorder, especially among the elderly, where blood accumulates between the brain and its outer covering. The primary treatment for CSDH involves surgical intervention, such as burr-hole craniotomy, with or without irrigation of the subdural space. The efficacy of irrigation versus no irrigation in reducing recurrence, mortality, and postoperative complications remains debated. The study aimed to compare the effectiveness and safety of irrigation versus no irrigation in the surgical management of CSDH through a systematic review and meta-analysis of randomized controlled trials (RCTs).
Methods: A systematic review and meta-analysis were conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Databases searched included PubMed, Scopus, Web of Science, and Cochrane Library, targeting RCTs published in English comparing irrigation with no irrigation in CSDH management. Four RCTs with a total of 843 patients met the inclusion criteria. Two reviewers extracted data independently, and the risk of bias 2 tool was used for quality assessment. The primary outcome was recurrence; secondary outcomes included mortality and postoperative complications. Statistical analyses were performed using RevMan 5.3.
Results: The meta-analysis included four RCTs with 843 patients, revealing that irrigation significantly reduces the recurrence of CSDH compared to no irrigation (odds ratios [OR] = 0.66, 95% confidence interval [CI]: 0.44–0.98, P = 0.04), with no observed heterogeneity (I2 = 0%). Mortality rates showed no significant difference between the irrigation and no irrigation groups (OR = 1.10, 95% CI: 0.59–2.06, P = 0.77), also with no heterogeneity (I2 = 0%). Postoperative complications initially showed no significant difference (OR = 0.39, 95% CI: 0.09–1.69, P = 0.21) and moderate heterogeneity (I2 = 52%). However, sensitivity analysis resolving the heterogeneity indicated a significant reduction in complications favoring the irrigation group (P = 0.03).
Conclusion: This meta-analysis suggests that irrigation during burr-hole drainage significantly reduces CSDH recurrence without increasing mortality or postoperative complications, supporting its use in clinical practice. Further, high-quality RCTs are necessary to confirm these findings and assess long-term outcomes.
Keywords: Burr-hole craniotomy, Chronic subdural hematoma, Irrigation, Meta-analysis, Recurrence
INTRODUCTION
Chronic subdural hematoma (CSDH) is a common neurological condition where blood products build up in the gap between the brain’s outer layer and its protective covering.[
The primary focus of CSDH management is surgical intervention, which involves removing the hematoma and preventing its reoccurrence.[
Irrigation entails the introduction of salt water or other irritants into the subdural space, either during or after the removal of a hematoma, to facilitate the removal of any remaining blood products and potentially decrease the likelihood of a recurrence.[
The ideal management strategy for CSDH, whether to use irrigation or not, is still uncertain due to conflicting evidence and inconsistent clinical practices despite the high occurrence of CSDH and the frequent use of surgical procedures.[
This meta-analysis aimed to synthesize current evidence and offer valuable insights into improving surgical techniques for managing CSDH. Our exclusive focus on RCTs is intended to increase the dependability and relevance of our findings.
MATERIALS AND METHODS
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we conducted a systematic review and meta-analysis of clinical randomized trials (RCTs) to compare the effectiveness and safety of irrigation versus no irrigation in the treatment of CSDH. By employing this method, we were able to methodically gather and examine available information, providing significant observations regarding the possible advantages of these interventions in the management of CSDH.[
Literature search
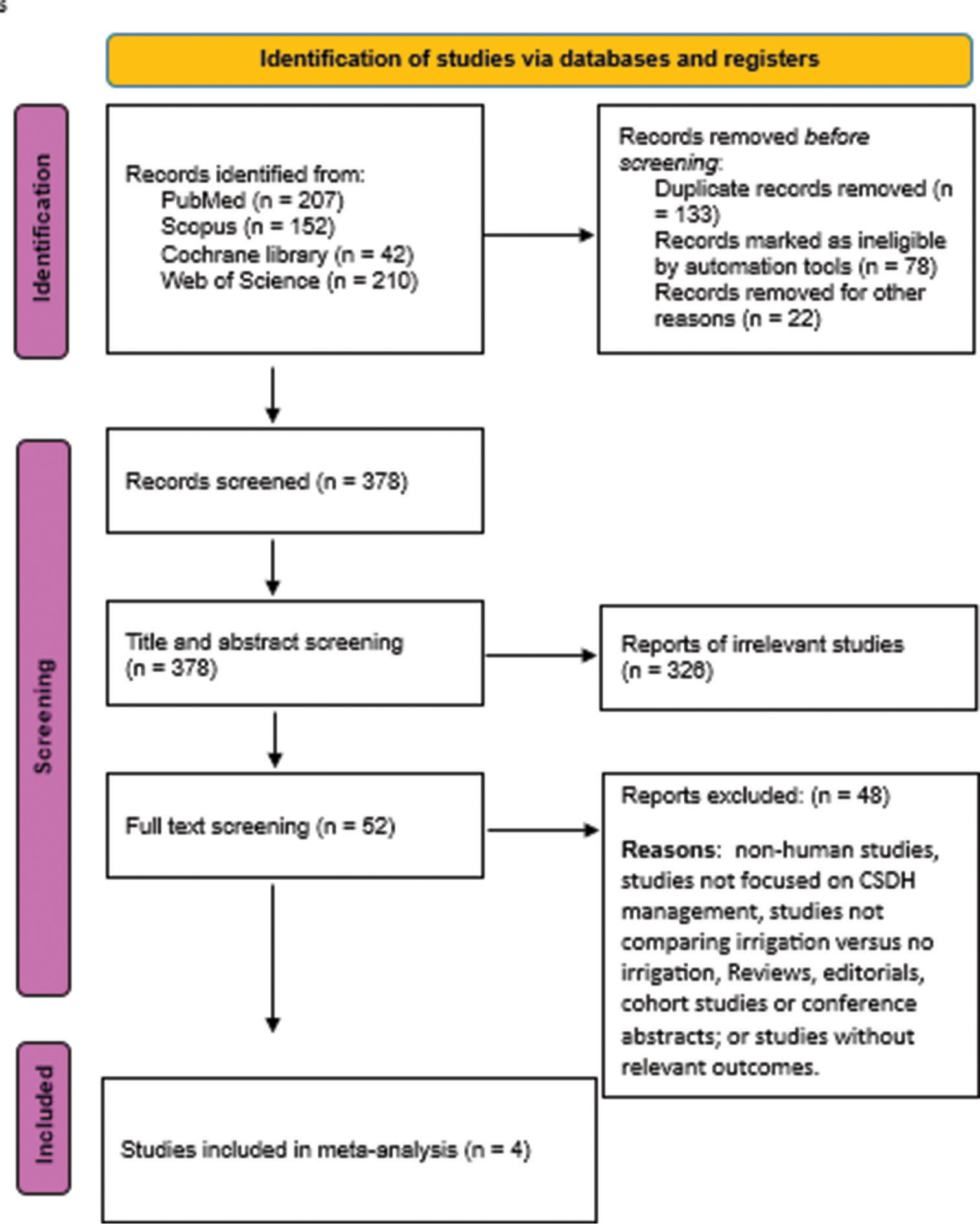
We performed a comprehensive literature search using PubMed, Scopus, Web of Science, and Cochrane Library databases. Our search specifically targeted RCTs published in English that evaluated the effectiveness of irrigation versus no irrigation in the management of CSDH. The search utilized keywords for irrigation, no irrigation, and CSDH. The initial search results were evaluated for relevancy by assessing the titles and abstracts. After reviewing the whole texts of papers that could be relevant, four RCTs were included in the meta-analysis.
Words such as “irrigation,” “no irrigation,” and “CSDH” were connected by the operator to ensure that all aspects of research containing these key terms were captured during search information To make the search more systematic and inclusive, the two search terms, “irrigation” and “CSDH,” were searched for in their synonyms and variants using the operator OR.
Study selection
The procedure of selecting studies was undertaken separately by two writers. Both individuals conducted a comprehensive assessment of the complete papers, addressing any inconsistencies or differences of opinion through mutual agreement. The selection procedure is outlined in the PRISMA diagram flowchart [
Initial screening
An initial search of the databases provided 611 records, which were reduced to 223 after identifying the duplicates, and 378 records were considered for screening. After identifying the titles and abstracts, both reviewers screened the studies; 326 studies were removed for not being eligible (for instance, non-RCTs or unrelated subjects).
Full-text review
Of the 52 studies, the full text was further searched to determine its suitability according to the following inclusion criteria: a randomized clinical trial that compared irrigation to no irrigation in CSDH. Of these, 48 studies were excluded on account of factors that included different interventions, study design, or lack of adequate data. Inter-observer bias was handled through conversation, or if required, the disparities were settled with a third reviewer.
Final inclusion
Out of 1264 patients, four RCTs were encompassed by inclusion criteria and applied in meta-analysis. These studies are presented in
PRISMA flow diagram
PRISMA flow chart of study selection is presented below in
Criteria for inclusion and exclusion
Inclusion criteria
Study design: RCTs compare the effectiveness and safety of irrigation with no irrigation in the treatment of CSDH Participants: patients with CSDH who perform surgical drainage Interventions: burr-hole drainage with irrigation Comparator: no irrigation Outcomes: Studies that reveal recurrence, mortality, and postoperative complications.
Exclusion criteria
Non-RCTs: Studies that are not RCTs, including observational studies, case reports, reviews, or meta-analyses Additional treatments: Research investigating the comparison of different irrigation solutions or studies investigating other approaches Non-English studies: Exclude articles that are not available in English to prevent potential translation bias Insufficient data: Research studies that lack complete outcome data or essential information that was unattainable from the authors.
Data extraction
We collected pertinent data from the chosen research and arranged it systematically in a specialized spreadsheet. The provided material encompassed crucial details, including the study’s design, the nation in which it was conducted, the sample size for each group, the age of participants (represented by the mean and standard deviation), the sex of each group, follow-up duration, and main findings. The data extraction was undertaken by two independent reviewers, who resolved any inconsistencies by discussion or third-party assessment.
Evaluating quality using risk of bias 2 (ROB2) tool
The ROB2 tool, a verified instrument for evaluating the propensity for bias in RCTs, was utilized. The evaluation encompasses bias arising from the randomization process, variations from intended interventions, missing outcome data, outcome assessment, and selection of the reported result [
Measured outcomes
The primary outcome assessed in this study was the recurrence. The secondary outcomes examined were mortality and postoperative complications.
Statistical analysis and heterogeneity
The statistical analysis was conducted using the RevMan 5.3 software. The Mantel–Haenszel method was used to combine dichotomous variables (recurrence, mortality, and postoperative complications) into odds ratios (OR). The study employed a fixed effects model, which is characterized by a larger standard error, higher weighting of smaller studies, and broader confidence intervals.
Heterogeneity in the forest plots was determined through visual inspection, while the I2 and Chi-square (χ2) tests were employed to quantify it. The χ2 test was used to examine the presence of significant heterogeneity, and if heterogeneity was detected, it was measured using the I2 test. The interpretation of the I2 test follows the standards outlined in the Cochrane Handbook for meta-analysis. According to these guidelines, an I2 value of 0–40% may not be considered significant, 30–60% may indicate moderate heterogeneity, 50–90% may suggest substantial heterogeneity, and 75–100% may indicate significant heterogeneity.
RESULTS
Literature search
Characteristics of the included studies
The 4 studies that were included in the analysis involved a combined total of 843 patients. These studies were conducted in various countries indicating the generalizability of our results. The interventions in these studies differed, comparing the use of irrigation versus no irrigation in the management of CSDH. A summary of characteristics can be found in
Quality assessment evaluation
The methodological quality of each trial was thoroughly evaluated using the Cochrane ROB Tool for Randomized Trials.[
The ROB2 tool evaluates the ROB across several subdomains, including
Bias arising from the randomization process: Guarantees that participants were correctly assigned into the groups they participated in, thus controlling for selection bias Bias due to deviations from intended interventions: Assessing the role of the performance bias by comparing the participants’ and investigators’ adherence to the intended intervention strategies Bias due to missing outcome data: Encourages the understanding of how missing data reduces the accuracy of the study’s findings Bias in the measurement of the outcome: Reviews the measures employed in determining the outcome in regard to both consistency and objectivity Bias in the selection of the reported result: This helped in making sure that all pre-specified outcomes were reported hence reducing reporting bias.
Data analysis
Recurrence
The analysis included data from four RCTs involving a total of 843 patients to assess the recurrence of CSDH following irrigation versus no irrigation treatments. The pooled (OR) for recurrence favored irrigation, with an OR of 0.66 (95% CI: 0.44–0.98), indicating a statistically significant difference in favor of irrigation (P = 0.04). There was no heterogeneity among the studies (I2 = 0%) [
Mortality
Mortality outcomes were analyzed across the same 3 RCTs with 763 patients. The pooled OR for mortality was 1.10 (95% CI: 0.59–2.06), indicating no significant difference between irrigation and no irrigation groups in terms of mortality risk (P = 0.77). There was no heterogeneity among the studies (I2 = 0%) [
Postoperative complications
The analysis of postoperative complications included data from the 3 RCTs with 763 patients. The pooled OR was 0.39 (95% CI: 0.09–1.69), suggesting no significant difference in the risk of postoperative complications between irrigation and no irrigation groups (P = 0.21). Heterogeneity among the studies was moderate (I2 = 52%) [
Figure 5:
Comparison of surgical complications between irrigation and no irrigation groups. This figure presents a forest plot of the odds ratio with 95% confidence intervals (CI) for various studies, indicating the overall effect size and heterogeneity among the included studies. M-H: Mantel-Haenszel
Figure 6:
Comparison of postoperative infection rates between irrigation and no irrigation groups. This figure presents a forest plot of the odds ratio with 95% confidence intervals (CI) for various studies, indicating the overall effect size and heterogeneity among the included studies. M-H: Mantel-Haenszel
DISCUSSION
In this systematic review and meta-analysis, four RCTs involving 843 patients were included, comparing irrigation versus no irrigation techniques in CSDH management. These trials, conducted globally, presented consistent surgical approaches but varied in irrigation use. Using the Cochrane ROB Tool, three studies demonstrated robust methodologies, while one showed minor concerns. The meta-analysis indicated a significant benefit of irrigation in reducing recurrence rates (P = 0.04), with no heterogeneity observed. Mortality outcomes did not significantly differ between groups and initial moderate heterogeneity in postoperative complications was resolved post-sensitivity analysis, suggesting potential advantages with irrigation (P = 0.03).
Aljabali et al.[
In our systematic review and meta-analysis of four RCTs involving 843 patients, irrigation significantly reduced the recurrence of CSDH compared to no irrigation (OR = 0.66, 95% CI: 0.44–0.98, P = 0.04), with no observed heterogeneity (I2 = 0%). This underscores irrigation’s potential benefit in reducing recurrence rates, supporting its clinical utility. Conversely, Zhu et al.’s comprehensive meta-analysis of 402 studies found no significant association between irrigation and recurrence (P = 0.81), suggesting variability in findings across broader study contexts.[
Our findings contrast with the findings of Yuan et al.,[
The recurrence of CSDH following surgery may be attributed to multiple factors, including the pathophysiology of CSDH, advanced age, reduced brain re-expansion, bilateral CSDH, and large hematoma size. This may be attributed to a multitude of variables that contribute to the development of CSDH, including the specific pathophysiology of CSDH, advanced age, decreased brain re-expansion following surgery, bilateral CSDH, and the presence of a big hematoma.[
The FINISH trial, conducted by Raj et al., was a Finnish, nationwide, multicenter, randomized, controlled, non-inferiority trial comparing burr-hole drainage with and without irrigation for the treatment of CSDH. Enrolling 589 patients from five neurosurgical units, the study aimed to determine if non-inferiority of the no-irrigation approach could be established. The primary outcome was the reoperation rate within 6 months, with a non-inferiority margin set at 7.5%. The trial found that 18.3% of participants in the no-irrigation group required reoperation compared to 12.6% in the irrigation group, with a difference of 6.0 percentage points (95% CI 0.2–11.7; P = 0.30), indicating higher reoperation rates without irrigation. There were no significant differences in functional outcomes or mortality rates between the groups, nor in the number of adverse events. These findings suggest that while functional outcomes and mortality are similar, burr-hole drainage with irrigation reduces the need for reoperation, thereby favoring the use of subdural irrigation.[
Limitations
This meta-analysis has several limitations that should be acknowledged. First, the relatively small number of included RCTs (four) and the total sample size (843 patients) may limit the generalizability of the findings. In addition, the studies varied in terms of their methodologies, patient populations, and definitions of outcomes, which could introduce heterogeneity and affect the results. The potential for publication bias is another concern, as studies with non-significant results might be underreported. Furthermore, the included trials did not consistently report on all secondary outcomes, such as detailed postoperative complications, which may lead to an incomplete assessment of the safety profile of the interventions.
CONCLUSION
This systematic review and meta-analysis of four RCTs indicate that burr-hole drainage with irrigation significantly reduces the recurrence rate of CSDH compared to burr-hole drainage without irrigation. Our findings support the use of irrigation during CSDH surgery as it may lower the need for reoperations without significantly impacting mortality or increasing postoperative complications. Despite the limitations, this analysis provides valuable evidence favoring the incorporation of irrigation into surgical protocols for CSDH management. Further, large-scale, high-quality RCTs are warranted to confirm these results and to explore the long-term outcomes and safety of irrigation in diverse patient populations.
Author’s contributions
Conceptualization, Writing – original draft, Writing – review and editing: All authors.
Data availability statement
All data are available on the internet.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
“This work was supported by the Deanship of Scientific Research, Vice Presidency for Graduate Studies and Scientific Research, King Faisal University, Saudi Arabia (KFU241828)”
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
The authors acknowledge the Deanship of Scientific Research at King Faisal University for obtaining financial support for research, authorship, and the publication of research under Research Proposal Number (KFU241828).
References
1. Abdelhady MA, Aljabali A, Al-Jafari M, Serag I, Elrosasy A, Atia A. Local anesthesia with sedation and general anesthesia for the treatment of chronic subdural hematoma: A systematic review and meta-analysis. Neurosurg Rev. 2024. 47: 162
2. Adhiyaman V, Chattopadhyay I, Irshad F, Curran D, Abraham S. Increasing incidence of chronic subdural haematoma in the elderly. QJM. 2017. 110: 375-8
3. Aljabali A, Sharkawy AM, Jaradat B, Serag I, Al-Dardery NM, Abdelhady M. Drainage versus no drainage after burr-hole evacuation of chronic subdural hematoma: A systematic review and meta-analysis of 1961 patients. Neurosurg Rev. 2023. 46: 251
4. Aljabali A, Serag I, Diab S, Alhadeethi AZ, Abdelhady M, Alkhawaldeh IM. Irrigation versus no irrigation in the treatment of chronic subdural hematoma: An updated systematic review and meta-analysis of 1581 patients. Neurosurg Rev. 2024. 47: 130
5. Aljabali A, Serag I, Abouzid M, Abdelhady M, Alkhawaldeh IM, Diab S. Irrigation versus no irrigation in the treatment of chronic subdural hematoma: An updated systematic review and meta-analysis of 1581 patients (P7-11.019). Neurology. 2024. 102: 3223
6. Alkhawaldeh IA, Serag I, Abouzid M, Hamdallah A, AlJafari M, Abdelhady M. Comparison of subperiosteal or subgaleal drainage with subdural drainage on the outcome of chronic subdural hematoma surgery (P7-11.012). Neurology. 2024. 102: 3247
7. Belkhair S, Pickett G. One versus double burr holes for treating chronic subdural hematoma meta-analysis. Can J Neurol Sci. 2013. 40: 56-60
8. Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN. The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012. 35: 155-69
9. Erol FS, Topsakal C, Faik Ozveren M, Kaplan M, Tiftikci MT. Irrigation vs. closed drainage in the treatment of chronic subdural hematoma. J Clin Neurosci. 2005. 12: 261-3
10. Gurelik M, Aslan A, Gurelik B, Ozum U, Karadag O, Kars HZ. A safe and effective method for treatment of chronic subdural haematoma. Can J Neurol Sci. 2007. 34: 84-7
11. Ishibashi A, Yokokura Y, Adachi H. A comparative study of treatments for chronic subdural hematoma: Burr hole drainage versus burr hole drainage with irrigation. Kurume Med J. 2011. 58: 35-9
12. Kim SS, Won JC, Kwon HS, Kim CH, Lee JH, Park TS. Prevalence and clinical implications of painful diabetic peripheral neuropathy in type 2 diabetes: results from a nationwide hospital-based study of diabetic neuropathy in Korea. Diabetes Res Clin Pract. 2014. 103: 522-9
13. Markwalder TM. Chronic subdural hematomas: A review. J Neurosurg. 1981. 54: 637-45
14. Miranda LB, Braxton E, Hobbs J, Quigley MR. Chronic subdural hematoma in the elderly: Not a benign disease. J Neurosurg. 2011. 114: 72-6
15. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001. 95: 256-62
16. Nouri A, Gondar R, Schaller K, Meling T. Chronic subdural hematoma (cSDH): A review of the current state of the art. Brain Spine. 2021. 1: 100300
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021. 372: n71
18. Raj R, Tommiska P, Koivisto T, Leinonen V, Danner N, Posti JP. Burr-hole drainage with or without irrigation for chronic subdural haematoma (FINISH): A Finnish, nationwide, parallel-group, multicentre, randomised, controlled, non-inferiority trial. Lancet. 2024. 403: 2798-806
19. Serag I, Abdelhady M, Awad AA, Wageeh A, Shaboub A, Elhalag RH. Postoperative elevated bed header position versus supine in the management of chronic subdural hematoma: A systematic review and meta-analysis. Acta Neurol Belg. 2024. 124: 1177-87
20. Shim YS, Park CO, Hyun DK, Park HC, Yoon SH. What are the causative factors for a slow, progressive enlargement of a chronic subdural hematoma?. Yonsei Med J. 2007. 48: 210-7
21. Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019. 366: l4898
22. Wang QP, Yuan Y, Guan JW, Jiang XB. A comparative study of irrigation versus no irrigation during burr hole craniostomy to treat chronic subdural hematoma. BMC Surg. 2017. 17: 99
23. Yang W, Huang J. Chronic subdural hematoma: Epidemiology and natural history. Neurosurg Clin N Am. 2017. 28: 205-10
24. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: Results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003. 98: 1217-21
25. Yuan Y, Wang QP, Cao YL, Zhang H, Burkutally MS, Budryte K. Burr hole drainage and burr hole drainage with irrigation to treat chronic subdural hematoma: A systematic review and meta-analysis. Medicine (Baltimore). 2018. 97: e11827
26. Zakaraia AM, Adnan JS, Haspani MS, Naing NN, Abdullah JM. Outcome of 2 different types of operative techniques practiced for chronic subdural hematoma in Malaysia: An analysis. Surg Neurol. 2008. 69: 608-15
27. Zhu F, Wang H, Li W, Han S, Yuan J, Zhang C. Factors correlated with the postoperative recurrence of chronic subdural hematoma: An umbrella study of systematic reviews and meta-analyses. EClinicalMedicine. 2022. 43: 101234