- Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY, and Editor-in-Chief of Surgical Neurology International,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA, and 1122 Franklin Avenue Suit 106, Garden City, NY 11530.
Correspondence Address:
Nancy E. Epstein M.D., F.A.C.S., Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and c/o Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA,.
DOI:10.25259/SNI_1172_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Why are spine surgeons sued, and with what outcomes?. 10-Feb-2023;14:46
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Why are spine surgeons sued, and with what outcomes?. 10-Feb-2023;14:46. Available from: https://surgicalneurologyint.com/surgicalint-articles/12152/
Abstract
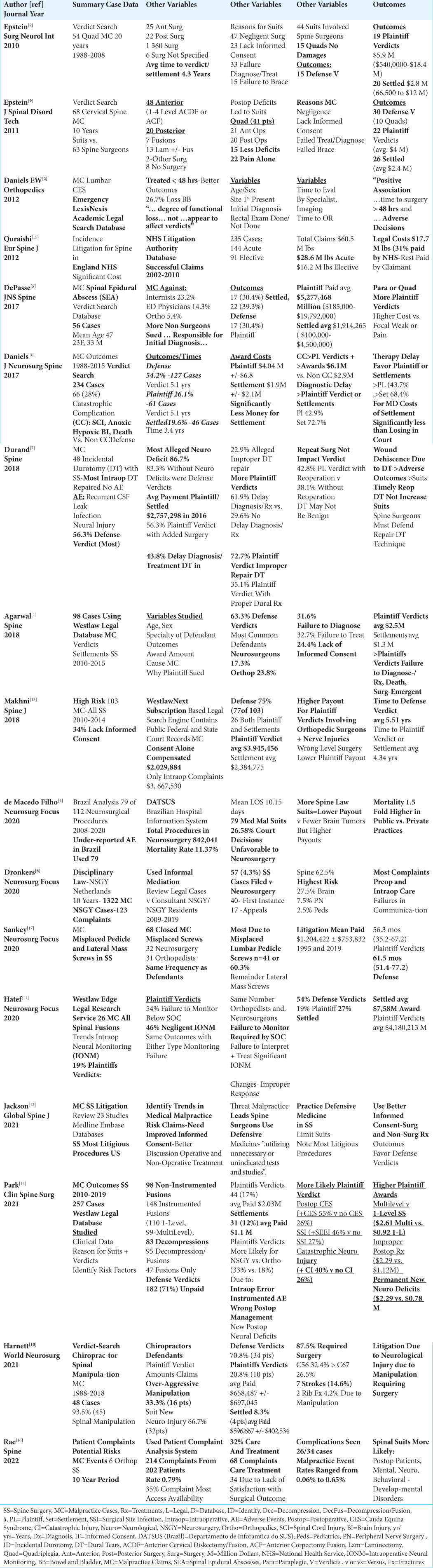
Background: Why are spine surgeons sued, how successfully, and for how much? Typical bases for spinal medicolegal suits have included; the failure to timely diagnose and treat, surgical negligence, (i.e. especially resulting in significant neurological deficits), and the lack of informed consent. We reviewed 17 medicolegal spinal articles looking for additional reasons for suits, along with identifying other factors contributing to defense verdicts, plaintiffs’ verdicts, or settlements.
Methods: After confirming the same three most likely causes of medicolegal suits, other factors leading to such suits included; the lack of patient access to surgeons postoperatively, poor postoperative management (i.e. contributing to new postoperative neurological deficits), failure to communicate between specialists/surgeons perioperatively, and failure to brace.
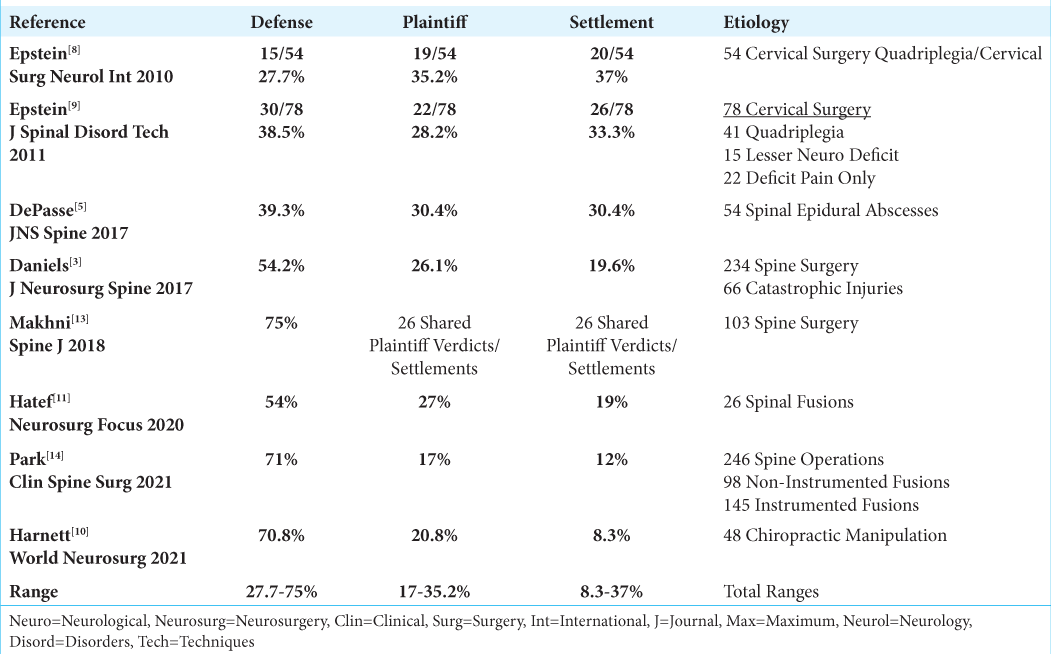
Results: Critical factors leading to more plaintiffs’ verdicts and settlements along with higher payouts for both included new severe and/or catastrophic postoperative neurological deficits. Conversely, defense verdicts were more likely for those with less severe new and/or residual injuries. The total number of plaintiffs’ verdicts ranged from 17-35.2%, settlements, from 8.3-37%, and defense verdicts from 27.7-75%.
Conclusion: The three most frequent bases for spinal medicolegal suits continue to include; failure to timely diagnose/treat, surgical negligence, and lack of informed consent. Here, we identified the following additional causes of such suits; the lack of patient access to surgeons perioperatively, poor postoperative management, lack of specialist/surgeon communication, and failure to brace. Further, more plaintiffs’ verdicts or settlements and greater respective payouts were observed for those with new and/or more severe/catastrophic deficits, while more defense verdicts were typically rendered for patients with lesser new neurological injuries.
Keywords: Malpractice suits, Spine surgery, Orthopedics, Neurosurgery, Negligent surgery, Failure to diagnose/ treat, Lack of Informed consent, Defense and plaintiffs’ verdicts, Settlements, Payouts, Catastrophic neurological injury
INTRODUCTION
In this review of 17 medicolegal spine studies, we confirmed that the three major bases for spinal medicolegal suits still included; the failure to diagnose and treat in a timely fashion, negligent surgery, and the lack of informed consent [
Reasons for Medicolegal Suits in Spine Surgery
Failure to diagnose and treat in a timely fashion
Various studies cite different reasons for medicolegal suits involving spine surgery [
Failure to diagnose/treat lumbar cauda equina syndromes (CES)
Using the LexisNexis Database, Daniels et al. (2012) examined the following multiple variables contributing to CES suits; whether a rectal exam was performed when the patient originally presented (i.e. typically the lack thereof), and the time it took for a specialist to see the patient, obtain imaging, and operate [
Failure to diagnose and treat spinal epidural abscesses (SEA)
DePasse et al. (2017) noted that their 56 suits were mostly against physicians who failed to diagnose a SEA; these predominantly included internists (23.2%), and emergeny room physicians (14.3%), with only 5.4% involving spinal orthopedic surgeons [
Variables contributing to delays in diagnosis and treatment
In 4 studies, multiple variables contributed to delays in diagnosis and treatment [
Surgical negligence
Several studies addressed negligent surgery/technical surgical errors as contributing to plaintiffs’ verdicts and settlements.[
Negligent dural repair
Durand et al. (2018) analyzed 48 cases involving “incidental durotomies using three legal databases; they alleged delays in diagnosis/treatment (43.8%), or cited “improper durotomy repair” (22.9%) [
Negligent placement of spinal screws
In Sankey et al. (2020) 32 neurosurgeons and 31 orthopedists (31) were sued for 68 cases attributed to misplaced spinal screws, (i.e. 41 lumbar pedicle screws, 17 cervical lateral mass screws) [
Negligent surgery and failures of postoperative management contributed to more plaintiffs’ verdicts and settlements
Park et al. (2021) 257 spinal cases resulted in 17% plaintiffs’ verdicts, and 12% settlements largely attributed to: intraoperative errors/negligence in instrumented fusions, failures in postoperative management, and new postoperative neurological deficits [
Negligent failure to use intraoperative neural monitoring or improper intraoperative neural monitoring
Hatef et al. (2020) evaluated 26 medicolegal cases addressing failures to use intraoperative neural monitoring (IONM) (i.e. arguing the Standard of Care required monitoring), and “improper” or negligent monitoring (i.e. failure to appropriately respond/treat significant changes) [
Negligent chiropractic manipulation
Harnett et al., (2021) evaluated 48 spinal medicolegal suits (Verdict Search) against chiropractors; 45 had undergone direct spinal manipulation that resulted in 32 new post-manipulation neurological deficits with 87.5% of these patients requiring surgery [
Lack of informed consent
Multiple studies raised lack of informed consent as a major reason for filing medicolegal suits [
Other reasons for spinal malpractice suits
Other reasons were identified for patients filing spinal malpractice actions. [
It is Not Just the Spine Surgeons Who are Sued
In spine malpractice cases, many suits were brought against treating physicians other than spinal surgeons [
Variable Frequency of Medicolegal Suits Against Neurosurgeons, Orthopedic Surgeons, and Chiropractors
In Agarwal et al. (2018 study) 98 suits, spinal neurosurgeons were defendants in 17.3% of cases, while 23.8% were orthopedists.[
Catastrophic Injuries and More Severe Neurological Deficits Led to More Plaintiffs’ Verdicts and Settlements
In our review of 17 medicolegal studies, greater neurological deficits and/or catastrophic injuries led to more frequent and higher plaintiffs verdicts and settlements, and fewer defense verdicts [
Less Severe Neurological Deficits Correlated with More Defense Verdicts
More defense verdicts were observed in series where patients had less severe neurological deficits.[
Highest Mean, and Highest and Lowest Payouts for Plaintiffs’ Verdicts
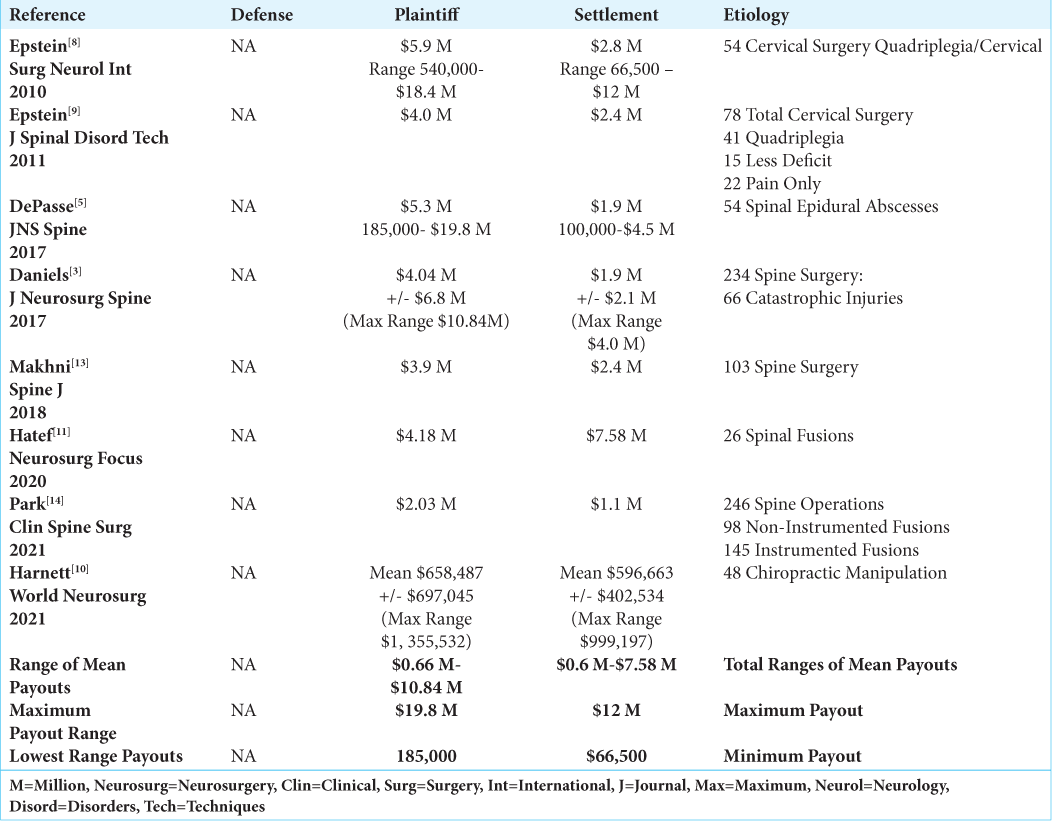
The mean payouts for plaintiffs verdicts ranged from $0.66 Million to $5.9M [
Highest Mean, and Highest and Lowest Payouts for Settlements
The highest mean payouts for settlements ranged from $7.58 M for the 26 patients in Hatef ’s series undergoing spinal fusions, to $2.8 in Epstein’s 2010 and $2.4 M in Epstein’s 2011 studies respectively [
Mean Duration and Range of Times for Verdicts or Settlements to be Rendered
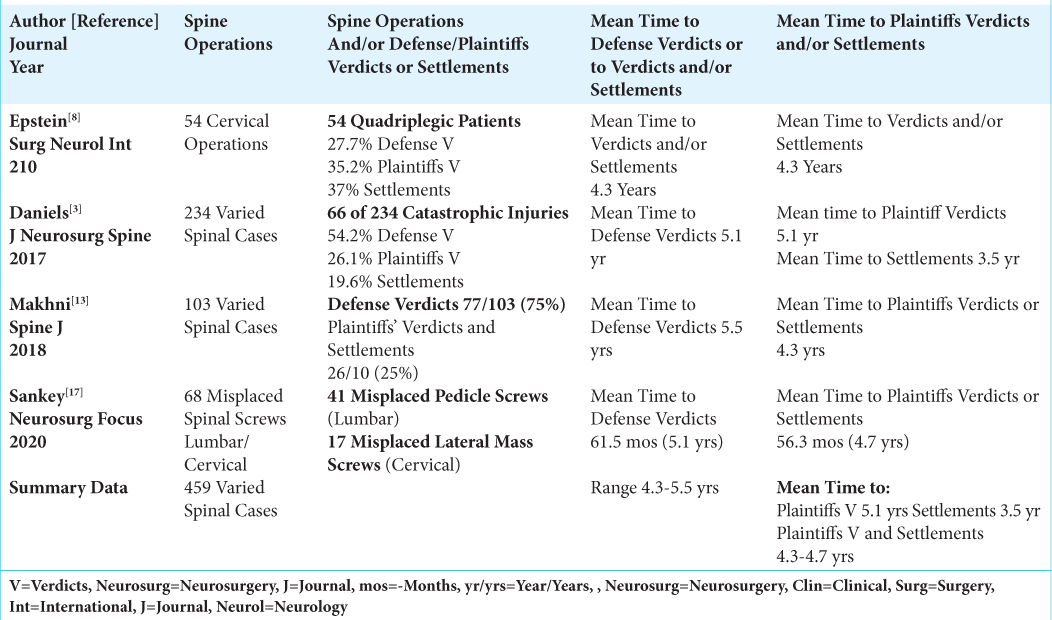
Four studies offered the mean and ranges of times until verdicts or settlements were reached [
Medicolegal Suits Involved Multiple Different Spine Operations
Multiple types of spinal procedures led to medicolegal suits, [
Spinal Litigation in England: A Report from the National Health Service (NHS)
Quraishi et al. (2012) focused on the costs of spinal litigation to the National Health Service in England vs. the costs to claimants within their socialized medical system [
CONCLUSION
Most medicolegal spinal suits arise from the failure to timely diagnosis/treat a spinal problem, negligent surgery, the lack of informed consent, limited access of patients to their surgeons perioperatively, poor postoperative management, and failures of communication between specialists/surgeons [
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agarwal N, Gupta R, Agarwal P, Matthew P Wolferz Jr, Shah A. Descriptive analysis of state and federal spine surgery malpractice litigation in the United States Spine. Phila Pa 1976. 2018. 43: 984-90
2. Daniels EW, Gordon Z, French K, Ahn UM, Ahn NU. Review of medicolegal cases for cauda equina syndrome: What factors lead to an adverse outcome for the provider?. Orthopedics. 2012. 35: e414-9
3. Daniels AH, Ruttiman R, Eltorai AE, DePasse JM, Brea BA, Palumbo MA. Malpractice litigation following spine surgery. J Neurosurg Spine. 2017. 27: 470-5
4. de Macedo Filho LJ, Aragao AC, Moura IA, Olivier LB, Albuquerque LA. Malpractice and socioeconomic aspects in neurosurgery: A developing-country reality. Neurosurg Focus. 2020. 49: E13
5. DePasse JM, Ruttiman R, Eltorai AE, Palumbo MA, Daniels AH. Assessment of malpractice claims due to spinal epidural abscess. J Neurosurg Spine. 2017. 27: 476-80
6. Dronkers WJ, Amelink QJ, Buis DR, Broeckman ML, Spoor JK. Disciplinary law and neurosurgery: A 10-year analysis of cases in the Netherlands. Neurosurg Focus. 2020. 49: E9
7. Durand WM, Eltorai AE, Shantharam G, DePasse JM, Kuris EO, Hersey AE. Medical malpractice claims following incidental durotomy due to spinal surgery spine. Phila Pa 1976. 2018. 43: 940-5
8. Epstein NE. A medico-legal review of cases involving quadriplegia following cervical spine surgery: Is there an argument for a no-fault compensation system?. Surg Neurol Int. 2010. 1: 3
9. Epstein NE. A review of medicolegal malpractice suits involving cervical spine: What can we learn or change?. J Spinal Disord Tech. 2011. 24: 15-9
10. Harnett DA, Milner JD, Kleinhenz Kuris EO, Daniels AH. Malpractice litigation involving chiropractic spinal manipulation. World Neurosurg. 2021. 149: e108-15
11. Hatef J, Katzir M, Toop N, Islam M, Clark T, Roscoe C. Damned if you monitor, damned if you don’t: Medical malpractice and intraoperative neuromonitoring for spinal surgery. Neurosurg Focus. 2020. 49: E19
12. Jackson KL, Rumley J, Griffith M, Linkous T, Abochukwu U, Devine J. Medical malpractice claims and mitigation strategies following spine surgery. Global Spine J. 2021. 11: 782-91
13. Makhni MC, Park PJ, Jimenez J, Saifi C, Caldwell JM, Ha A. The medicolegal landscape of spine surgery: How do surgeons fare?. Spine J. 2018. 18: 209-15
14. Park HY, Hwang R, Sheppard WL, Blumstein G, Shah AA, Medina JA. Predictors of medical malpractice outcomes after spine surgery: A comprehensive analysis from 2010 to 2019. Clin Spine Surg. 2021. 34: 228-35
15. Quraishi NA, Hammett TC, Todd DB, Bhutta MA, Kapoor V. Malpractice litigation and the spine: The NHS perspective on 235 successful claims in England. Eur Spine J. 2012. 21: S196-9
16. Rae M, Rocha DF, Hayes DS, Haak M, Maniar H, Grandizio LC. Formal patient complaints and malpractice events involving orthopedic spine surgeons: A ten-year analysis. Spine (Phila Pa 1976). 2022. 47: E521-6
17. Sankey EW, Mehta VA, Wang TY, Than TT, Goodwin CR, Okarikari I. The medicolegal impact of misplaced pedicle and lateral mass screws on spine surgery in the United States. Neurosurg Focus. 2020. 49: E20