- Department of Neurosurgery, Japan Community Health Care Organization, Chukyo Hospital, Nagoya, Japan.
- Department of Neurosurgery, Nagoya University Graduate School of Medicine, Nagoya, Japan.
Correspondence Address:
Jungsu Choo, Department of Neurosurgery, JCHO Chukyo Hospital, Nagoya, Japan.
DOI:10.25259/SNI_749_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jungsu Choo1, Kenko Maeda1, Masaya Takemoto1, Yusuke Sakamoto1, Yoshitaka Nagashima2. Widespread spontaneous spinal epidural hematoma treated with a combined technique using a flexible neuroendoscope after hemilaminectomy: A case report. 13-Oct-2023;14:361
How to cite this URL: Jungsu Choo1, Kenko Maeda1, Masaya Takemoto1, Yusuke Sakamoto1, Yoshitaka Nagashima2. Widespread spontaneous spinal epidural hematoma treated with a combined technique using a flexible neuroendoscope after hemilaminectomy: A case report. 13-Oct-2023;14:361. Available from: https://surgicalneurologyint.com/surgicalint-articles/12596/
Abstract
Background: One-third of spinal epidural hematomas occur spontaneously, and these may be associated with the acute onset of severe paralysis. Here, we present a case of T4-L4 symptomatic spontaneous spinal epidural hematoma which was successfully removed using a flexible neuroendoscope after hemilaminectomy.
Case Description: Using flexible neuroendoscopy, we successfully treated a T4-L4 spinal epidural hematoma in an 89-year-old Japanese female who spontaneously developed back pain and paraparesis. The hematoma was removed utilizing a hemilaminectomy at three vertebral levels (T11, T12, and L1), while the remaining hematoma debris was completely evacuated with flexible neuroendoscopy. Neurological improvement was observed immediately postsurgery.
Conclusion: Flexible neuroendoscopy provided a less extensive surgical method for removing a T4-L4 spontaneous epidural hematoma.
Keywords: Flexible neuroendoscopy, Hemilaminectomy, Spinal epidural hematoma, Spinal surgery
INTRODUCTION
The incidence of spinal epidural hematomas is 0.1/100,000.[
CASE DESCRIPTION
History and diagnosis
An 89-year-old Japanese female developed the spontaneous onset of back pain and paraparesis (i.e., motor weakness, hyperreflexia, and sensory loss). Magnetic resonance imaging (MRI) revealed a dorsal epidural hematoma from T4 to L4 [
Figure 1:
T2-weighted magnetic resonance imaging of the thoracolumbar spine with epidural hematoma from T4 to L4 vertebrae. The hematoma was the thickest at the T12 level (12 mm). Contrast-enhanced computed tomography detected no source of bleeding. This was a symptomatic multi-vertebral spinal epidural hematoma requiring emergency surgery. This was explained to the patient who provided informed consent for surgery.
Surgical strategy and treatment
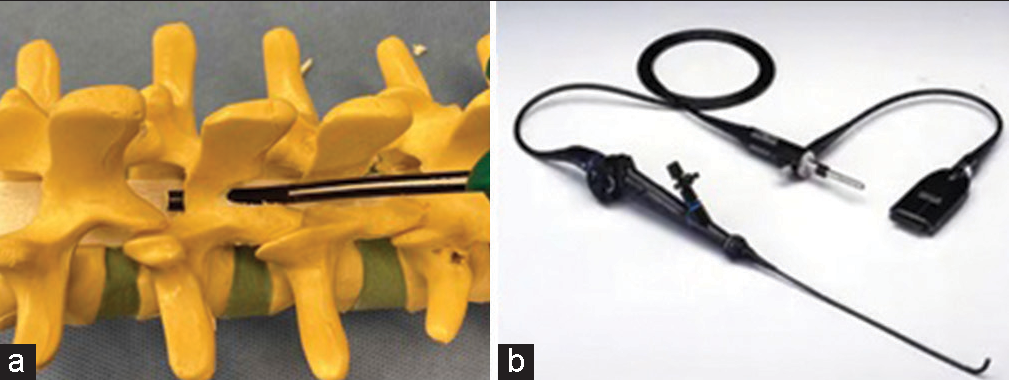
We performed a hemilaminectomy at the T11, T12, and L1 levels and removed/debrided additional intervening hematoma using a flexible neuroendoscope. The flexible neuroendoscope had an outer diameter of 5 mm [
Figure 2:
Intraoperative views (a) After left hemilaminectomy, the epidural hematoma is suctioned, and the dura mater is located. (b) A flexible neuroendoscope is inserted from the hematoma removal cavity. (c) A hematoma is present in front of the neuroendoscope. (d) After removal of the hematoma, the hematoma is cleared, the dura mater (asterisk) is visible on the lower side of the scope’s screen, and the epidural fat (black arrow) is visible on the upper side.
Postoperative course
Immediately after surgery, the patient exhibited some neurological recovery. The postoperative MRI showed no residual hematoma [
DISCUSSION
Typically, patients with SSEH require rapid decompression to treat significant spinal cord/cauda equina compression and avert permanent neurological deficits.[
A Few Hemilaminectomies and a flexible neuroendoscope to remove extensive SSEH
Here, we performed hemilaminectomies at three spinal levels through which we introduced a flexible neuroendoscope to remove/debride/suction epidural clots [
This approach could reduce surgical invasiveness compared to conventional procedures, proving particularly useful for widespread hematoma. Given that a flexible endoscope can reach narrow areas and allow continuous irrigation from its tip, it could allow effective cleaning and removal of both epidural abscesses and epidural hematomas.
CONCLUSION
We describe the successful removal of a spontaneous T4-L4 epidural hematoma utilizing a three-level hemilaminectomy (T11, T12, and L1), through which we could introduce a flexible neuroendoscope.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ali Y, Roux FX, Meder JF, Pallud J. Symptomatic extensive thoracolumbar epidural hematoma following lumbar disc surgery treated by single level laminectomy. Asian Spine J. 2012. 6: 152-5
2. Bakker NA, Veeger NJ, Vergeer RA, Groen RJ. Prognosis after spinal cord and cauda compression in spontaneous spinal epidural hematomas. Neurology. 2015. 84: 1894-903
3. Cheng YP, Lee KW, Lin PY, Huang AP, Cheng CY, Ma HI. Full-endoscopic interlaminar removal of chronic lumbar epidural hematoma after spinal manipulation. Surg Neurol Int. 2014. 5: 55
4. Di Rienzo A, Brunozzi D, Dobran M, Iacoangeli M, Colasanti R, Trivedi R. Skip hemilaminectomy for large, multilevel spinal epidural hematomas: Report of a series of 11 patients. World Neurosurg. 2018. 111: e933-40
5. Holtås S, Heiling M, Lönntoft M. Spontaneous spinal epidural hematoma: Findings at MR imaging and clinical correlation. Radiology. 1996. 199: 409-13
6. Kim N, Jung SB. Biportal endoscopic spine surgery in the treatment of multi-level spontaneous lumbar epidural hematoma: Case report. J Orthop Sci. 2022. 27: 288-91
7. Lo CC, Chen JY, Lo YK, Lai PH, Lin YT. Spontaneous spinal epidural hematoma: A case report and review of the literatures. Acta Neurol Taiwan. 2012. 21: 31-4
8. Peng D, Yan M, Liu T, Yang K, Ma Y, Hu X. Prognostic factors and treatments efficacy in spontaneous spinal epidural hematoma: A multicenter retrospective study. Neurology. 2022. 99: e843-50
9. Sarubbo S, Garofano F, Maida G, Fainardi E, Granieri E, Cavallo MA. Spontaneous and idiopathic chronic spinal epidural hematoma: Two case reports and review of the literature. Eur Spine J. 2009. 18: 1055-61
10. Shin JJ, Kuh SU, Cho YE. Surgical management of spontaneous spinal epidural hematoma. Eur Spine J. 2006. 15: 998-1004
11. Wu ZY, Zhu YJ, Chu L, Cheng CY, Chen CM, Hui-Ting H. Full-endoscopic transforaminal approach for removal of a spontaneous spinal epidural hematoma. World Neurosurg. 2017. 98: 883.e13-20