- Department of Neurosurgery, Indiana University School of Medicine, Indianapolis, United States
- Department of Neurosurgery, University of California, Sacramento, California, United States
- Department of Neurosurgery, John A. Burns School of Medicine, University of Hawaii, Honolulu, United States
- Department Otolaryngology-Head and Neck Surgery, University of California, Sacramento, California, United States
Correspondence Address:
Varun Rao, Department of Neurosurgery, Indiana University School of Medicine, Indianapolis, United States.
DOI:10.25259/SNI_461_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Varun Rao1, Clayton H. Gerndt2, Vera Ong3, Edward Bradley Strong4, Kiarash Shahlaie2. Worsening orbital roof “blow-in” fractures following traumatic brain injury: A report of two cases. 06-Sep-2024;15:316
How to cite this URL: Varun Rao1, Clayton H. Gerndt2, Vera Ong3, Edward Bradley Strong4, Kiarash Shahlaie2. Worsening orbital roof “blow-in” fractures following traumatic brain injury: A report of two cases. 06-Sep-2024;15:316. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13086
Abstract
Background: Orbital roof fractures are often the result of high-velocity collisions and are seen in 1–9% of patients with craniofacial trauma. Although the majority of orbital roof fractures are displaced superiorly, a subset results in inferior displacement of fracture fragments, posing a risk for muscle/nerve entrapment and possible blindness. Many of these patients have severe traumatic brain injury (TBI) and, in addition to orbital fractures, also have elevated intracranial pressure (ICP). Management of depressed orbital roof fractures in the setting of severe TBI with elevated ICP represents a management dilemma.
Case Description: Two cases of severe TBI with associated downward displacement of orbital roof fractures were reviewed. Both cases exhibited elevated ICP correlated with the degree of orbital roof fracture depression. Surgical intervention involving elevation and repair of the fractures was undertaken when there was a significant risk of injury to the extraocular muscles and/or the optic nerve due to the extent of the fracture depression.
Conclusion: Depressed orbital roof fractures may migrate in response to changes in ICP. Serial computed tomography scans and eye examinations may aid with determining the need for and timing of surgical intervention.
Keywords: Cerebral spinal fluid, Intracranial pressure, Supraorbital roof fracture, Transpalpebral
INTRODUCTION
Orbital roof fractures are often the result of high-velocity collisions and are seen in 1–9% of patients with craniofacial trauma.[
CASE #1
A 26-year-old male was admitted after a high-speed motor vehicle accident. His Glasgow Coma Scale (GCS) score was 7 on arrival, and he was emergently intubated. His head computed tomography (CT) scan demonstrated multiple comminuted and depressed skull fractures as well as bilateral orbital roof fractures [
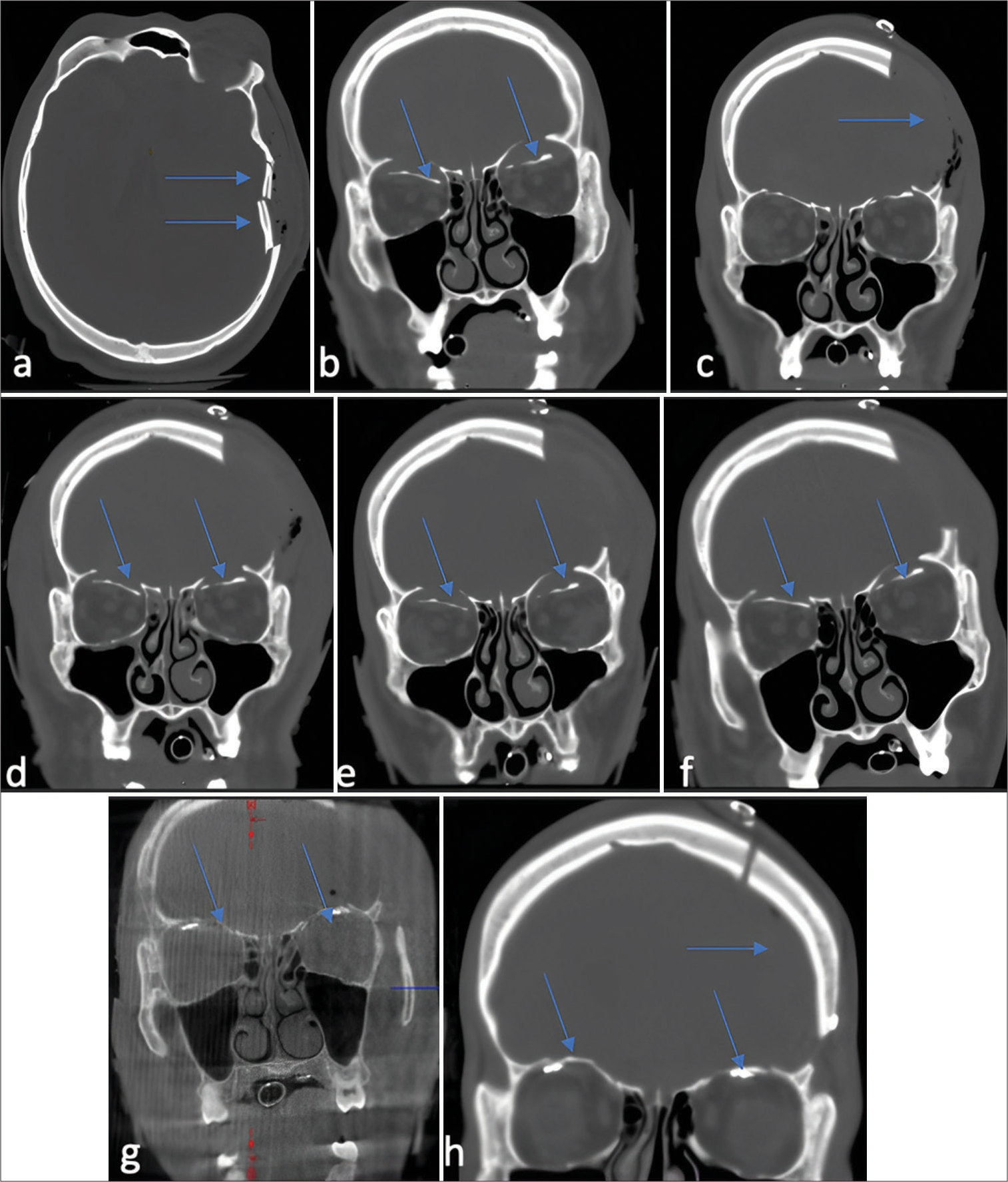
Figure 2:
(a and b) Case 1: Computed tomography (CT) imaging of fracture fragments over time. Axial and coronal bone window CT images from admission demonstrating left calvarial depressed skull fracture fragments and bilateral orbital roof blow in fractures. (c) Coronal CT bone window status post left-sided decompressive craniectomy on postoperative day 0. (d-f) Migration of fragments over time shows 3 mm and 2.9 mm of inferior displacement on the right and left side, respectively. (g) Intraoperative O-arm CT after orbital roof reduction and fixation and (h) post cranioplasty 1 month after orbital roof repairs. *Arrows denote findings described in each image.
The patient underwent left decompressive hemicraniectomy and external ventricular drain placement. ICP was monitored throughout treatment [
ICP was monitored throughout treatment [
A follow-up CT scan on postoperative day (POD) 2 demonstrated an interval increase in the frontal lobe edema and increased inferior displacement of orbital roof fragments to 7.3 mm and 6.0 mm on the right and left side, respectively [
A bilateral upper blepharoplasty approach was used to expose and reduce both orbital roofs, stabilizing them with customized mini-plates bent to a sterile anatomic model. The plates were fixated just behind the superior orbital rim, avoiding screw placement in the mobile bone segments. Intraoperative CT imaging facilitated the repositioning of the left plate for proper reduction. The remainder of the patient’s hospital course was uneventful. The patient was discharged to a skilled nursing facility on post-injury day 81. At 3 months after surgery, the patient was doing well with intact visual fields and no diplopia.
CASE #2
A 40-year-old female was brought in following a motor vehicle accident. Her GCS score was 7, prompting emergent intubation. A post-resuscitation head CT scan demonstrated multifocal intracerebral hemorrhages and bilateral orbital fractures. The right and left orbital roof fragments were inferiorly displaced by 2.6 and 7.0 mm, respectively [
Figure 3:
(a) Case 2: Computed tomography (CT) and Magnetic resonance imaging of fracture fragments over time. Coronal CT bone window image from admission showing inferior displacement of the right and left orbital roofs, now at 3.1 and 9.1 mm, respectively, and (b) 20 h later showing 2.8 and 13.2 mm of inferior displacement of the right and left orbital roof respectively. (c and d) The continued increase in depression over 2 days (e) led to repair and intraop O-arm image after reduction of fracture. (f) T2 coronal image with arrow denoting collagen onlay duraplasty. *Arrows denote findings described in each image.
Ophthalmologic examination demonstrated mild anisocoria, briskly reactive pupils, and no relative afferent pupillary defect. Intraocular pressures were slightly elevated and felt to be secondary to periorbital edema and swelling.
A repeat head CT 20 h after injury demonstrated stable multicompartmental hemorrhages and slight worsening of the inferior displacement of the right and left orbital roofs, now at 3.1 and 9.1 mm, respectively [
Due to concerns about worsening inferior displacement on the left side [
The patient was discharged to a board and care home on post-injury day 57. The patient did not attend follow-up appointments with neurosurgery, ophthalmology, or otolaryngology after discharge.
DISCUSSION
This report highlights the potential for orbital roof fractures to migrate inferiorly in patients experiencing elevated ICP. The dynamic progression of associated injuries, such as hematomas and contusions, demands comprehensive imaging and clinical surveillance. Our observations reveal that all orbital roof fractures, regardless of being non-displaced or minimally displaced, necessitate reassessment, especially in scenarios of elevated ICP.
Indications for surgical management of orbital roof fractures
Management of orbital roof fractures is focused on preserving visual acuity, maintaining normal extraocular movement, and preventing the functional and cosmetic consequences of enophthalmos or exophthalmos. The presence of orbital dystopia, enophthalmos, exophthalmos, extraocular muscle entrapment, high intraocular pressure, and alterations in visual acuity have all been proposed as indications for surgical intervention.[
Surgical approaches for orbital roof fracture management
Most orbital roof fractures can be addressed through a transpalpebral or a bicoronal/frontal craniotomy approach.[
Connon et al. developed a classification and treatment algorithm for orbital roof fractures, advocating for craniotomies in cases with “blow-in” fractures associated with intracranial trauma and functional impairments of extraocular muscles, ocular function, or nerves.[
CONCLUSION
The management of orbital roof “blow-in” fractures involves a multidisciplinary approach to ensure optimal outcomes. It is important to recognize that these fractures can be mobile and may migrate with elevated ICP. Therefore, serial eye examinations and/or CT imaging should be considered in patients with depressed orbital roof fractures and episodes of elevated ICP.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chirico PA, Mirvis SE, Kelman SE, Karesh JW. Orbital “blow-in” fractures: Clinical and CT features. J Comput Assist Tomogr. 1989. 13: 1017-22
2. Connon FV, Austin SJ, Nastri AL. Orbital roof fractures: A clinically based classification and treatment algorithm. Craniomaxillofac Trauma Reconstr. 2015. 8: 198-204
3. Haug RH. Management of the trochlea of the superior oblique muscle in the repair of orbital roof trauma. J Oral Maxillofac Surg. 2000. 58: 602-6
4. Haug RH, Van Sickels JE, Jenkins WS. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 93: 238-46
5. Kim JW, Bae TH, Kim WS, Kim HK. Early reconstruction of orbital roof fractures: Clinical features and treatment outcomes. Arch Plast Surg. 2012. 39: 31-5
6. Locatelli D, Dallan I, Castelnuovo P. Surgery around the orbit: How to select an approach. J Neurol Surg B Skull Base. 2020. 81: 409-21
7. McLachlan DL, Flanagan JC, Shannon GM. Complications of orbital roof fractures. Ophthalmology. 1982. 89: 1274-8
8. Ohjimi H, Taniguchi Y, Tanahashi S, Era K, Fukushima T. Accessing the orbital roof via an eyelid incision: The transpalpebral approach. Skull Base Surg. 2000. 10: 211-6
9. Penfold CN, Lang D, Evans BT. The management of orbital roof fractures. Br J Oral Maxillofac Surg. 1992. 30: 97-103
10. Piotrowski WP, Beck-Mannagetta J. Surgical techniques in orbital roof fractures: Early treatment and results. J Craniomaxillofac Surg. 1995. 23: 6-11
11. Rha EY, Joo HS, Byeon JH. Orbital dystopia due to orbital roof defect. J Craniofac Surg. 2013. 24: e500-4
12. Rountree KM, Blase JJ. Isolated orbital roof blow-in fracture. Trauma Case Rep. 2017. 12: 16-8
13. Sandhu PS, Bucur S, Good C, Cutler M, Rajak S. The management of orbital roof fractures and defects: A review. Ophthalmic Plast Reconstr Surg. 2022. 38: 8-16
14. Stam LH, Wolvius EB, Schubert W, Koudstaal MJ. Natural course of orbital roof fractures. Craniomaxillofac Trauma Reconstr. 2014. 7: 294-7
15. Sullivan WG. Displaced orbital roof fractures: Presentation and treatment. Plast Reconstr Surg. 1991. 87: 657-61
16. Szabo KA, Cheshier SH, Kalani MY, Kim JW, Guzman R. Supraorbital approach for repair of open anterior skull base fracture. J Neurosurg Pediatr. 2008. 2: 420-3
17. Wagle WA, Eames FA, Wood GW. Orbital roof blow-in fractures: CT demonstration. J Comput Assist Tomogr. 1987. 11: 918-9