- College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
- Department of Pathology and Laboratory Medicine, King Abdulaziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia
- Department of Neurosurgery, King Abdulaziz Medical City, National Guard Health Affairs, Jeddah, Saudi Arabia.
Correspondence Address:
Abdulaziz M. Alghamdi, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_646_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Abdulaziz M. Alghamdi1,2, Abdulkarim M. Alghamdi1,2, Alaa Samkari1,2,3, Afnan Samman2,4, Ahmed Lary1,2,4. Xanthogranuloma of the suprasellar region mimicking cystic craniopharyngioma: A case report. 15-Sep-2023;14:331
How to cite this URL: Abdulaziz M. Alghamdi1,2, Abdulkarim M. Alghamdi1,2, Alaa Samkari1,2,3, Afnan Samman2,4, Ahmed Lary1,2,4. Xanthogranuloma of the suprasellar region mimicking cystic craniopharyngioma: A case report. 15-Sep-2023;14:331. Available from: https://surgicalneurologyint.com/surgicalint-articles/12556/
Abstract
Background: Xanthogranuloma of the sellar region is an extremely rare benign entity with only case reports and series documented in the literature. We aim to describe in this report a case of a suprasellar xanthogranuloma that was diagnosed initially as a cystic craniopharyngioma.
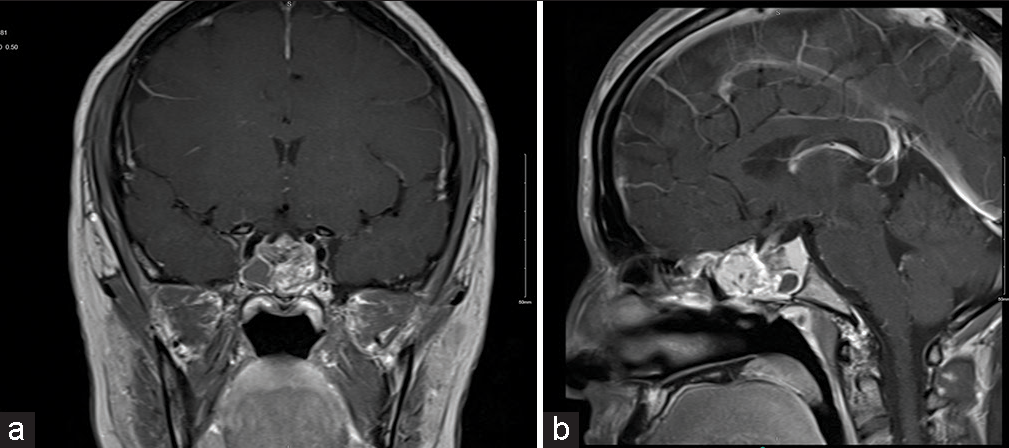
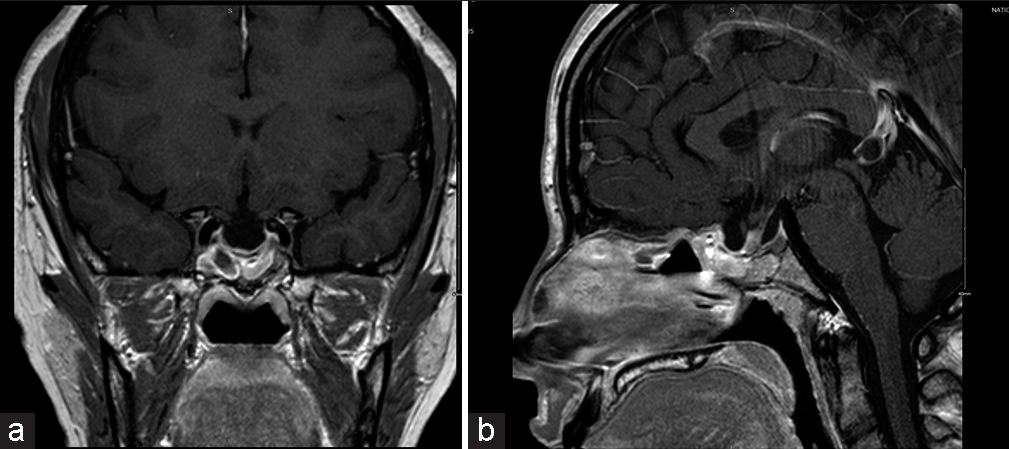
Case Description: A 28-year-old woman presented to the clinic with a 2-week history of headaches, blurred vision, nausea, and vomiting. She had no medical or surgical history, no signs of hormonal disturbances, and no family history of brain tumors or endocrine diseases. Her neurological examination was unremarkable except for bitemporal hemianopia on visual field testing. A magnetic resonance imaging of the brain showed a cystic mass in the sellar region that was compressing the optic chiasm with radiological features representing cystic craniopharyngioma. She underwent endoscopic transnasal transsphenoidal surgery to excise the mass, and only subtotal excision was achieved to preserve the pituitary function. The histopathology confirmed the diagnosis of a xanthogranuloma of the sellar region. The postoperative course was unremarkable, and she did not receive any adjuvant therapy. There was no recurrence of the clinical symptoms or the mass during the 18-month follow-up period.
Conclusion: Although xanthogranuloma is uncommon, it should be included in the differential diagnosis of sellar/suprasellar lesions. Due to its wide range of radiological features that sometimes can mimic other lesions, a definitive diagnosis can only be made postoperatively. Surgical excision is the most accepted treatment with a favorable prognosis and low rates of recurrence.
Keywords: Case report, Craniopharyngioma, Sellar region, Suprasellar region, Xanthogranuloma
INTRODUCTION
Sellar masses can present with a wide range of clinical and radiological features. Their presentations can range from asymptomatic incidental and hormonal effects to compressive local mass effects with presenting symptoms related to the specific anatomical landmarks of the sella turcica and the surrounding parasellar region.[
CASE DESCRIPTION
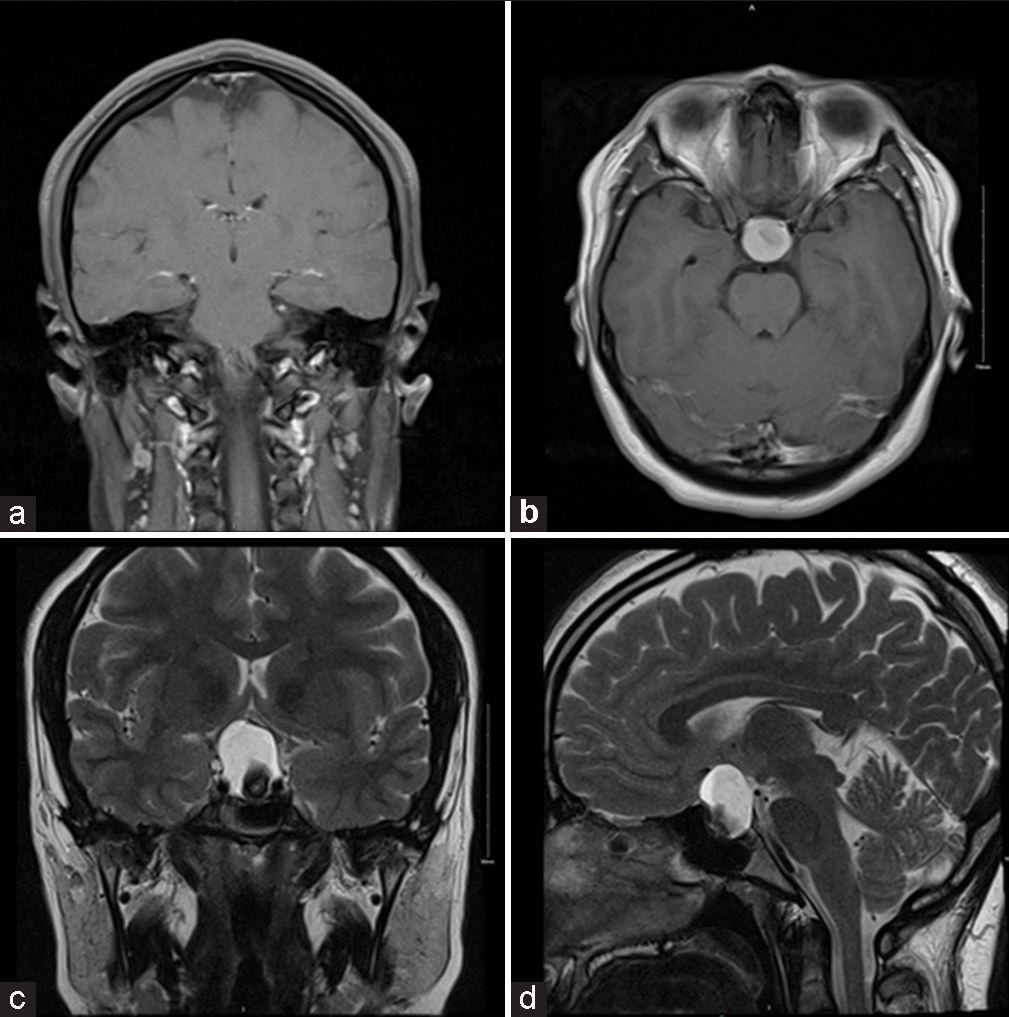
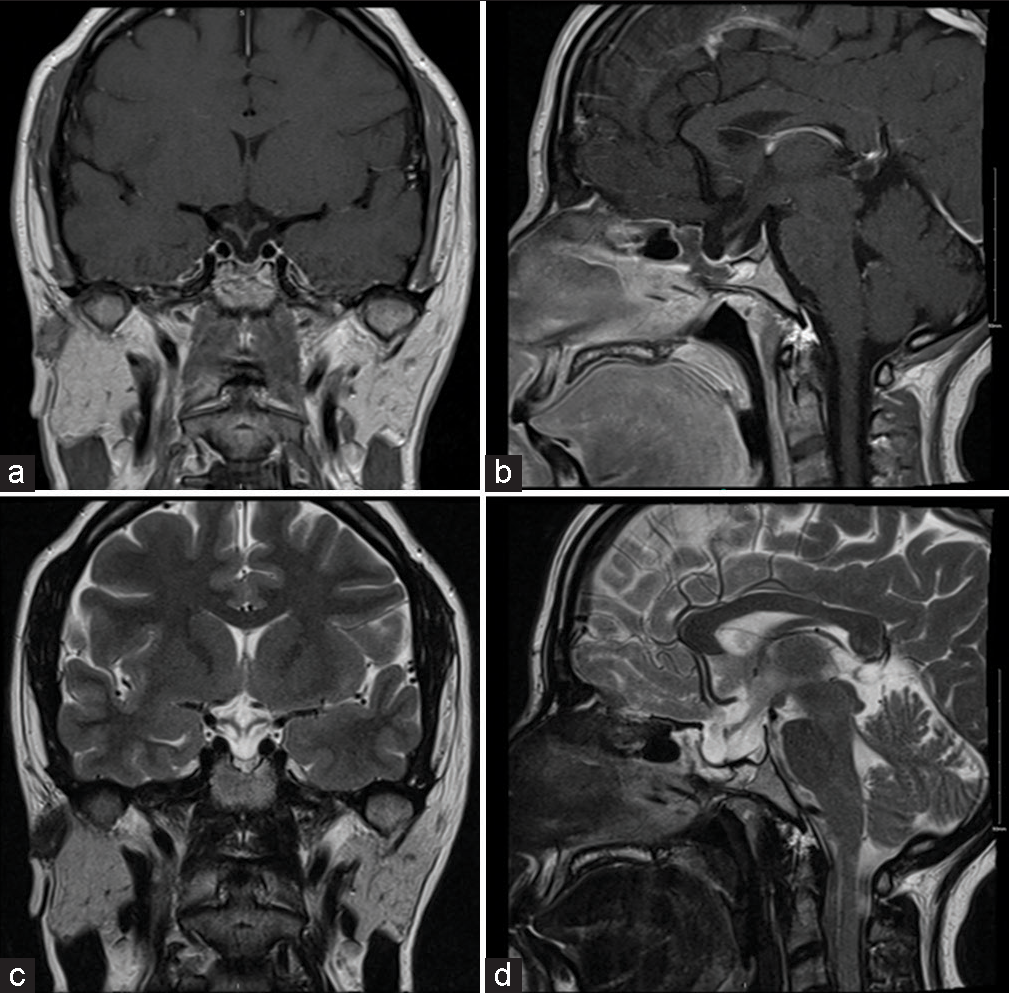
A 28-year-old Saudi right-handed woman, who is not known to have any medical or surgical history, presented to the clinic with a history of right-sided headaches associated with blurred vision for the past 2 weeks. The headache was severe, sudden, tension-like, associated with nausea and infrequent vomiting, and partially relieved by acetaminophen tablets. She had no history of trauma, loss of consciousness, or seizure. She had a history of irregular menses since puberty for which she was not investigated before. She had no symptoms of thyroid dysfunction or other hormonal disorders. She had no family history of brain tumors or endocrine diseases, and she was not taking any regular medications. Other systemic reviews were unremarkable. On examination, she was vitally stable, conscious, alert, and oriented. She had bitemporal hemianopia on visual field testing. Other cranial nerves, motor, sensory, and cerebellar functions were all intact. Her hormonal profile and laboratory tests were unremarkable. She underwent a brain MRI which demonstrated a clear intrasellar and suprasellar mass measuring 2.5 cm in its largest axis that was compressing the optic chiasm and displacing the anterior communicating artery [
DISCUSSION
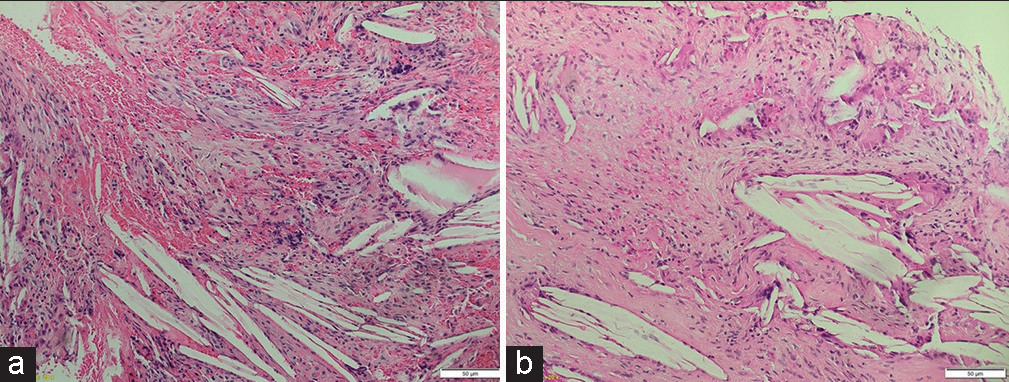
Xanthogranuloma is a benign histological entity characterized by a persistent chronic inflammatory reaction to the presence of cholesterol crystals in an enclosed space, secondary to either hemorrhage, infarction, inflammation, or necrosis. Inflammatory reaction markers of this entity include granulomatous tissue with cholesterol clefts, hemosiderin deposits, macrophages containing lipid-rich foam cells (also known as xanthoma cells), multinucleated giant cells, and lymphocytes.[
The clinical presentation of sellar xanthogranuloma is nonspecific with no selective gender or age distribution. It can range from completely asymptomatic presentations to mass-effect symptoms such as headaches, visual disturbances, and endocrine disturbances, which are similar to other sellar lesions.[
Preoperative diagnosis of sellar xanthogranuloma can be challenging as its radiological features are variant and can resemble other sellar lesions as a reflective measure of the complexity of its histologic components.[
Surgical gross total resection is the most acceptable treatment approach in symptomatic patients, with permanent panhypopituitarism reported as one of the most common surgical complications.[
Limitations
This study has some limitations as it only included one case report of sellar xanthogranuloma. However, considering how rare this condition is, we aim to contribute to the literature to help in understanding these lesions more. Further studies with more cases of sellar xanthogranuloma to help understand the underlying causes and predict the prognosis are recommended.
CONCLUSION
Sellar xanthogranuloma is an extremely rare lesion. Nevertheless, it should be included in the differential diagnosis of sellar/suprasellar lesions. It exhibits a wide range of radiological features, making diagnosing preoperatively difficult. This makes histopathological examination the definitive way of diagnosis. Surgical excision is the main treatment. It has a favorable prognosis with low rates of recurrence, only reported in subtotal gross resected cases. However, the benefits and harms of gross total surgical resection should be considered as it can cause permanent complications to the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmetgjekaj I, Harizi E, Rahman A, Hyseni F, Nasir F, Decka A. Giant cholesterol granuloma of petrous apex. Radiol Case Rep. 2022. 17: 1220-4
2. Famini P, Maya MM, Melmed S. Pituitary magnetic resonance imaging for sellar and parasellar masses: Ten-year experience in 2598 patients. J Clin Endocrinol Metab. 2011. 96: 1633-41
3. Guerrero-Pérez F, Marengo AP, Vilarrasa N, Vidal N, RuizRoig N, Sánchez-Fernández JJ. Xanthogranuloma of the sellar region: A systematic review. Hormones (Athens). 2023. 22: 199-210
4. La Rocca G, Rigante M, Gessi M, D’Alessandris QG, Auricchio AM, Chiloiro S. Xanthogranuloma of the sellar region: A rare tumor. Case illustration and literature review. J Clin Neurosci. 2019. 59: 318-24
5. Pilonieta M, Martin M, Revuelta Barbero JM, Hardesty DA, Carrau RL, Otto BA. Sellar cholesterol granuloma mimicking cystic sellar lesions: A report of three cases and literature review. World Neurosurg. 2020. 144: 250-5
6. Shirataki K, Okada S, Matsumoto S. Histopathological study of the “cholesterol granuloma reaction” in the sellar and juxtasellar tumors. No To Shinkei. 1988. 40: 133-9
7. WHO Classification of Tumours Editorial Boa, editors. Central Nervous System Tumours. Lyon: International Agency for Research on Cancer; 2021. 6:
8. Yang B, Yang C, Fang J, Li G, Wang J, Jia G. Clinicoradiologic features and surgical outcomes of sellar xanthogranulomas: A single-center 10-year experience. World Neurosurg. 2017. 99: 439-47