- Department of Orthospine, Sir Ganga Ram Hospital, New Delhi, India
Correspondence Address:
Nitin Maruti Adsul
Department of Orthospine, Sir Ganga Ram Hospital, New Delhi, India
DOI:10.4103/sni.sni_260_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: G. Sudhir, Nitin Maruti Adsul, Shankar Acharya, Rupinder S. Chahal. Compartment syndrome of lumbar paraspinal musculature after percutaneous pedicle screw fixation. 20-Sep-2018;9:190
How to cite this URL: G. Sudhir, Nitin Maruti Adsul, Shankar Acharya, Rupinder S. Chahal. Compartment syndrome of lumbar paraspinal musculature after percutaneous pedicle screw fixation. 20-Sep-2018;9:190. Available from: http://surgicalneurologyint.com/surgicalint-articles/9019/
Abstract
Background:Compartment syndromes have been reported in nearly every anatomical area of the extremities. Similarly, in the lumbar spine, there is a risk of a compartment syndrome following either direct or indirect injury to the paraspinal muscles. In this study, we present a case of lumbar paraspinal compartment syndrome after percutaneous pedicle screw fixation for a spine fracture.
Case Description:A 27-year-old obese female sustained a fall and an L1 fracture. Her neurological examination was normal. She underwent a minimally invasive percutaneous posterior pedicle screw fixation from T12 to L2 to stabilize the L1 fracture. Postoperatively, the patient developed hypoesthesia in the back, and sterile serous wound discharge. Because of the persistent discharge, an open debridement was performed that revealed multiple cavities within the necrotic avascular paraspinal musculature. Once these were completely excised, the wounds healed uneventfully.
Conclusion:Patients undergoing minimally invasive posterior thoracolumbar (TL) pedicle screw fixation can develop a compartment syndrome involving the TL paraspinal musculature. This case highlights the need for early consideration of a compartment syndrome when patients develop persistent sterile discharge after spine surgery. In this case, urgent decompression prevented any long-term sequelae.
Keywords: Compartment syndrome, lumbar paraspinal musculature, percutaneous posterior instrumentation
INTRODUCTION
Multiple studies document that compartment syndromes can involve the thoracolumbar (TL) paraspinal musculature following surgical manipulation.[
Various studies in literature have shown that minimally invasive pedicle screw fixation is a safe and effective surgery.[
CASE REPORT
Clinical presentation and surgery
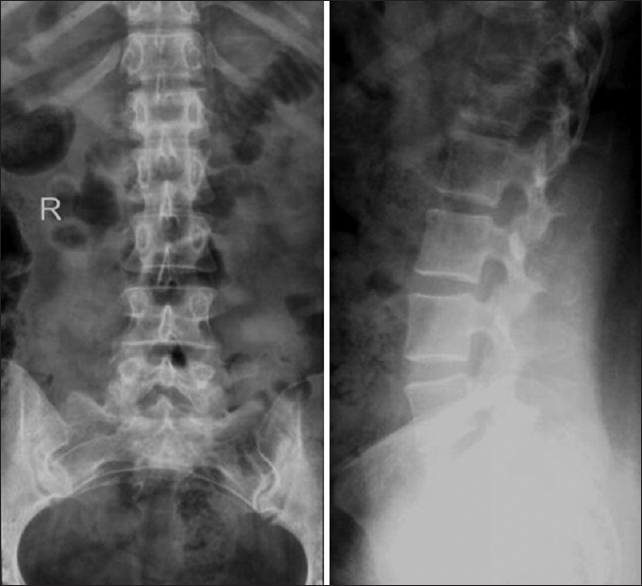
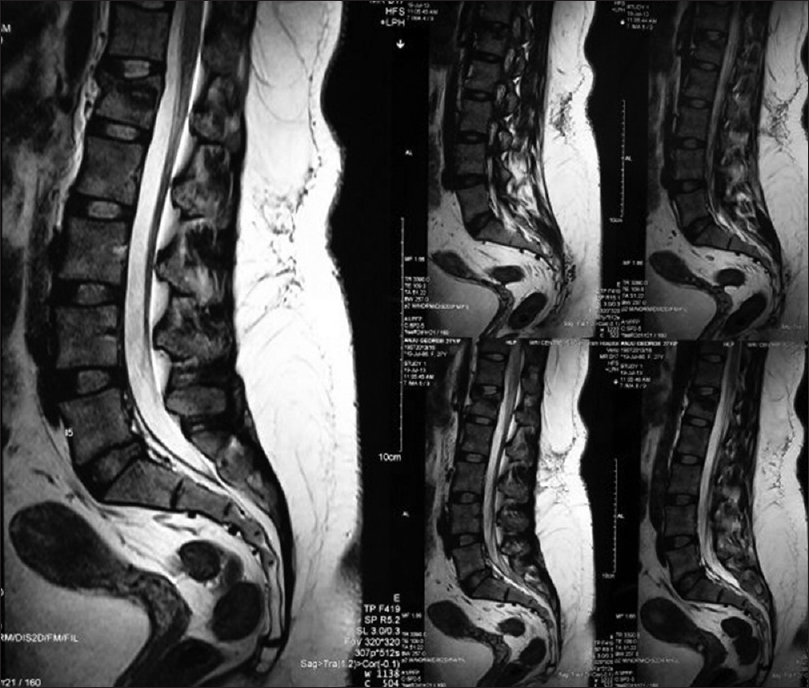
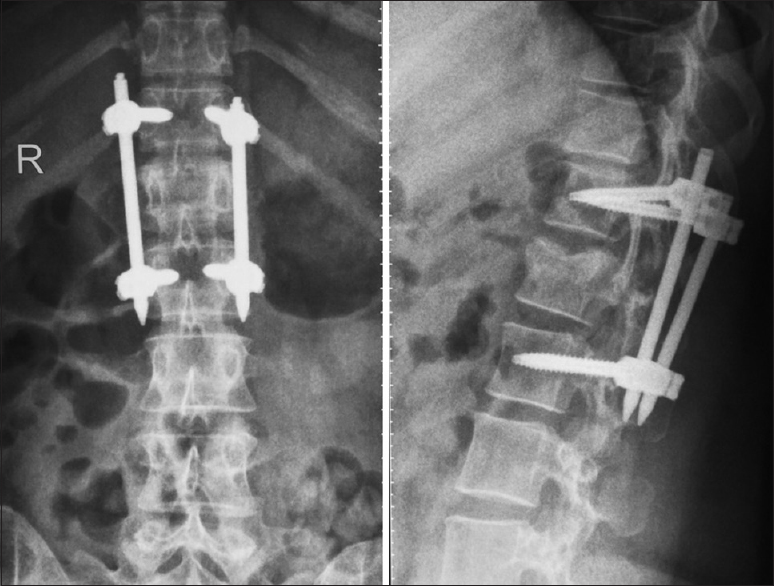
A 27-year-old female sustained a fall in the bathroom following which she presented with severe TL pain, and the inability to stand or walk. Although her neurological examination was normal, the X-rays and MRI studies confirmed an L1 burst fracture without accompanying neural compression [Figures
Postoperative course: Initial washout
Postoperatively, she did well until the third postoperative day at which time she developed severe back pain and serous discharge from the right L2 pedicle wound [
Secondary open debridement
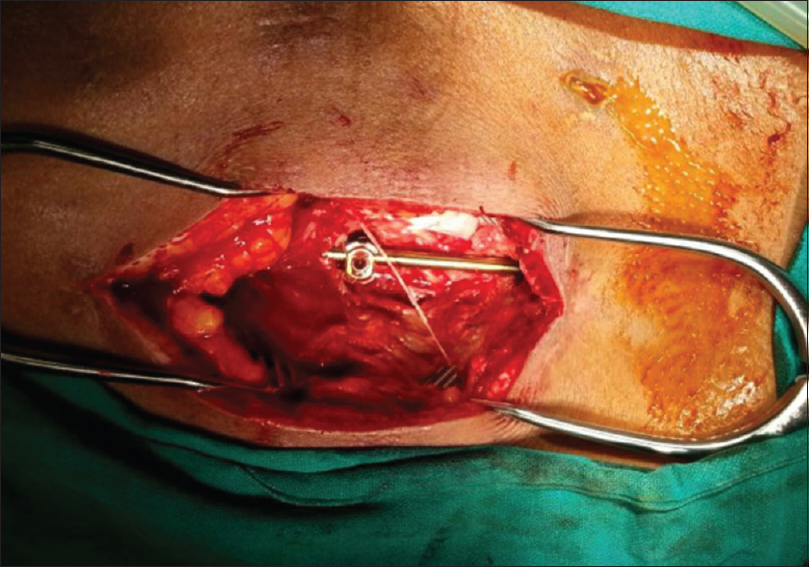
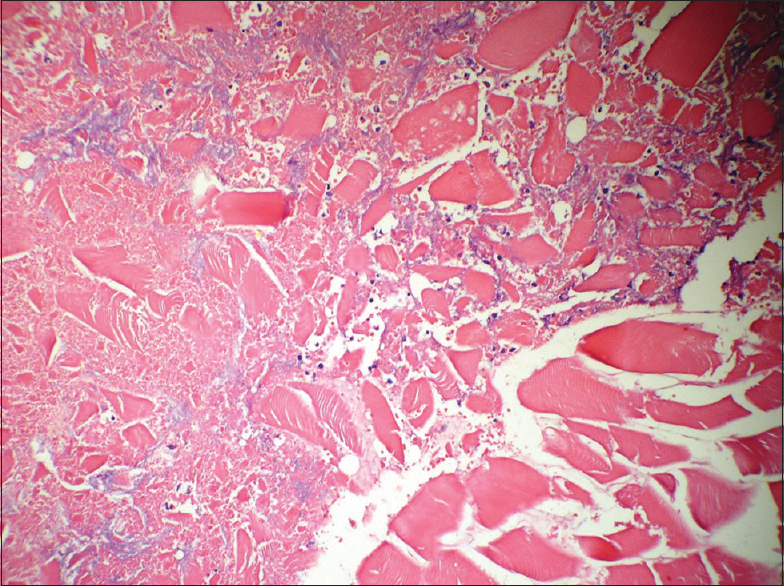
As the patient continued to have discharge without symptomatic improvement, she was taken back to the operating room. At this time, all incisions were opened, and the entire bilateral subfascial tracts were explored; the paraspinal muscles were pale, avascular, and non contractile [
DISCUSSION
Etiology of paralumbar compartment syndrome following percutaneous T12-L2 pedicle screw/rod placement
Acute compartment syndrome involving the paraspinal muscles has been reported in various settings including trauma, surgery, and non-traumatic situations.[
Symptoms and signs of paraspinal compartment syndrome
The physical signs for TL paraspinal musculature compartment syndrome includes loss of lumbar lordosis, sensory loss over the affected muscles, elevated serum CK, and elevated AST (Aspartate aminotransferase) levels; only one study additionally showed an elevated WBC count and increase in amylase.[
Minimally invasive trend
There is presently a trend toward minimally invasive TL spine surgery. Patients with acute and chronic lumbar paraspinal compartment syndromes typically demonstrate raised compartment pressures ranging from 70 to 150 mm Hg. Conservative treatment with medication and rest often results in successful recovery.[
CONCLUSION
A compartment syndrome involving the TL paraspinal musculature should be considered as a cause of persistent sterile drainage when patients have undergone posterolateral pedicle screw fixation. Here, this occurred in a patient with an L1 fracture undergoing a T12-L2 minimally invasive pedicle screw fusion. In cases like this one, urgent surgical decompression may prevent long-term sequelae resulting from avascular necrosis and fibrosis of the paraspinal musculature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barker PJ, Briggs CA. Attachments of the posterior layer of lumbar fascia. Spine (Phila Pa 1976). 1999. 24: 1757-64
2. DiFazio FA, Barth RA, Frymoyer JW. Acute lumbar paraspinal compartment syndrome. A case report. J Bone Joint Surg Am. 1991. 73: 1101-3
3. Ferreira J, Galle C, Aminian A, Michel P, Guyot S, De Wilde JP. Lumbar paraspinal rhabdomyolysis and compartment syndrome after abdominal aortic aneurysm repair. J Vasc Surg. 2003. 37: 198-201
4. Foley KT, Gupta SK. Percutaneous pedicle screw fixation of the lumbar spine: Preliminary clinical results. J Neurosurg. 2002. 97: 7-12
5. Khan RJ, Fick DP, Guier CA, Menolascino MJ, Neal MC. Acute paraspinal compartment syndrome. A case report. J Bone Joint Surg Am. 2005. 87: 1126-8
6. Kitajima I, Tachibana S, Hirota Y, Nakamichi K. Acute paraspinal muscle compartment syndrome treated with surgical decompression: A case report. Am J Sports Med. 2002. 30: 283-5
7. Ringel F, Stoffel M, Stüer C, Meyer B. Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery. 2006. 59: ONS361-6