- Department of Neurosurgery, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brazil
- Department of Neurosurgery, Pedro Ernesto University Hospital, Rio de Janeiro, Brazil
- Department of Surgical Specialties Neurosurgery Teaching and Assistance Unit, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brazil
- Department of Anatomical Pathology, Pedro Ernesto University Hospital, Rio de Janeiro, Brazil
- Department of Internal Medicine - Endocrine Service, Pedro Ernesto University Hospital, Rio de Janeiro, Brazil.
Correspondence Address:
Louise Ferreira Nascimento Pestana da Costa, Department of Neurosurgery, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brazil.
DOI:10.25259/SNI_786_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Louise Ferreira Nascimento Pestana da Costa1, Pedro Henrique Costa Ferreira-Pinto2, Julia Pereira Muniz Pontes3, Ana Carolina Gonçalves Brito4, Bernardo Martins Rodrigues Martha1, Wellerson Novaes da Silva1, Victor Hugo Corrêa Rodrigues1, Ana Beatriz Winter Tavares5, Elington Lannes Simões1, Felipe Gonçalves de Carvalho1, Flavio Nigri1. Endoscopic endonasal transsphenoidal approach during COVID-19 pandemic in Brazil. 04-Nov-2022;13:504
How to cite this URL: Louise Ferreira Nascimento Pestana da Costa1, Pedro Henrique Costa Ferreira-Pinto2, Julia Pereira Muniz Pontes3, Ana Carolina Gonçalves Brito4, Bernardo Martins Rodrigues Martha1, Wellerson Novaes da Silva1, Victor Hugo Corrêa Rodrigues1, Ana Beatriz Winter Tavares5, Elington Lannes Simões1, Felipe Gonçalves de Carvalho1, Flavio Nigri1. Endoscopic endonasal transsphenoidal approach during COVID-19 pandemic in Brazil. 04-Nov-2022;13:504. Available from: https://surgicalneurologyint.com/surgicalint-articles/11981/
Abstract
Background: Endoscopic endonasal transsphenoidal approach (EETA) is a well-established technique for sellar tumor resection. However, this route causes aerosol dispersion from the nasal cavity. In the context of the coronavirus (COVID-19) pandemic, new measures were taken aiming at the safety and protection of patients and health-care professionals. Herein, we present a Brazilian experience with EETA during COVID-19 pandemic.
Methods: This study was based on the review of medical records and observation in the operating room of the patients undergoing endoscopic surgery in the period from May 2020 to July 2022. All patients were tested by real-time polymerase chain reaction (RT-PCR) COVID-19 before and after surgery. Since September 2021, it has been mandatory to present vaccination cards for adults (over 18 years old).
Results: This case series included 28 patients and 35 surgical procedures using the EETA, who presented of nonfunctioning macroadenomas (19 cases − 67.8%), GH-secreting tumor (three cases − 10.8%), ACTH-secreting tumor (three cases − 10.8%), meningiomas (two cases − 7.1%), and Rathke’s cleft cyst (one case – 3.5%). There were eight cases of diabetes insipidus (28.5%), five cases of cerebrospinal fluid leak (17.8%), and one case of meningitis (3.5%). Three patients died due to meningitis (one case), carotid occlusion (one case), and COVID-19 complications (one case).
Conclusion: A simple protocol was established to perform EETA during the COVID-19 pandemic. The pituitary surgeries were maintained to treat critical cases. To date, the protocol should be continually updated to improve the procedure’s safety.
Keywords: COVID-19, Pandemic, Pituitary, Transsphenoidal
INTRODUCTION
Endoscopic endonasal transsphenoidal technique is the main surgical approach for most types of sellar and suprasellar lesions. It is a less invasive procedure with less complications, when compared to other approaches.[
MATERIALS AND METHODS
This case series described patients with pituitary lesions who underwent EETA from May 2020 to July 2022 in Pedro Ernesto University Hospital, Rio de Janeiro, Brazil. Because of the pandemic, only patients with a high risk of visual loss, severe hormonal dysfunction, apoplexy, or refractory headache were selected for surgery. The information used in this study was collected from the medical and surgical records, operating room (OR) observations, and pathology results.
A general safety protocol was established. The mandatory use of N95 for the professionals/patients inside the neurosurgery unit and the OR was implemented. In periods with increased COVID-19 cases, visits to hospitalized patients were suspended and all information were provided by video calls. Exceptions were made for hospital companions of patients under 18 s and over 65 s – with mandatory negative reverse transcriptase polymerase chain reaction (RT-PCR) for the COVID-19 test. The symptomatic or positive RT-PCR cases were isolated and transferred to internal COVID-19 units. Since September 2021, it has been mandatory to present vaccination cards for adults (over 18 years old). During the pandemic period, the staff and patients who presented respiratory symptoms or positive RT-PCR were submitted to a 10–14-day quarantine. It was possible to perform RT-PCR screening and avoid chest computed tomography (CT).
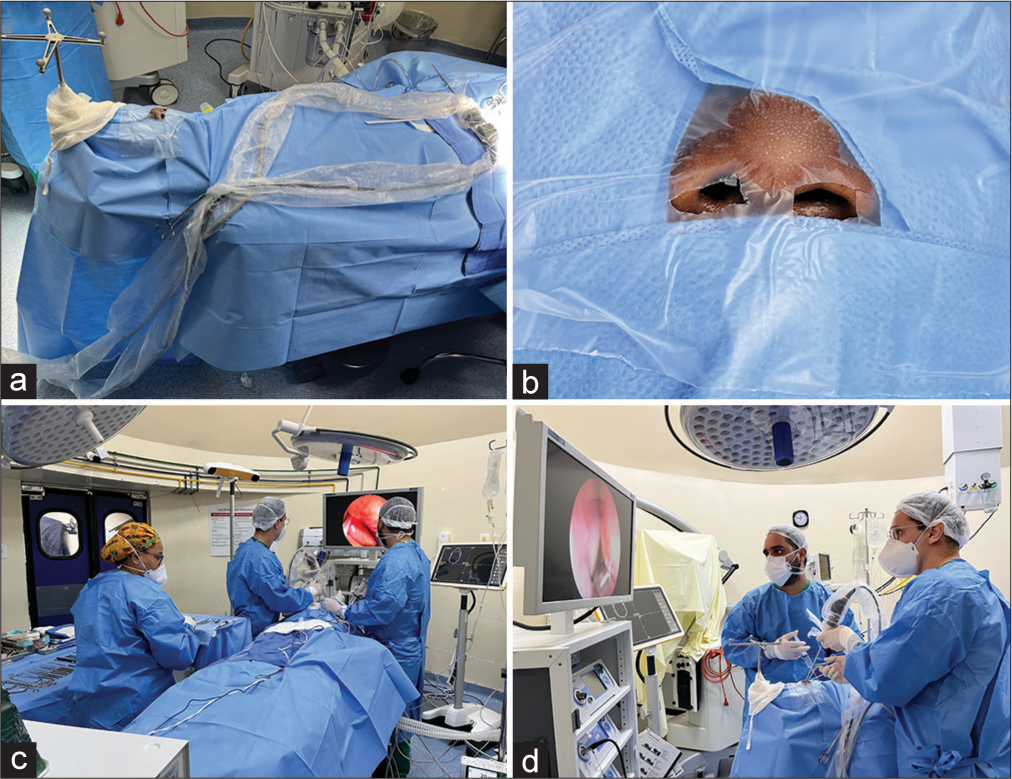
The surgical protocol was based on: (a) preoperative period: patient’s screening with RT-PCR at least 3 days before hospital admission for all patients. The surgical procedure was performed on the following day, (b) intraoperative period: preparation used a different anesthetic induction that was based on the rapid sequence intubation. It was constituted in a reduced dose of opioids (fentanyl or remifentanil) in the induction period, in addition to the lower doses of hypnotics (propofol and ketamine) and neuromuscular blockers (succinylcholine and rocuronium). Only the anesthesiologist was present in the OR during the intubation procedure. It was mandatory to use individual protection equipment, for example, gloves and cloak. A nasal drape (Steri-Drape, 3M, Minnesota, United States) was used to reduce the nostril entry area [
RESULTS
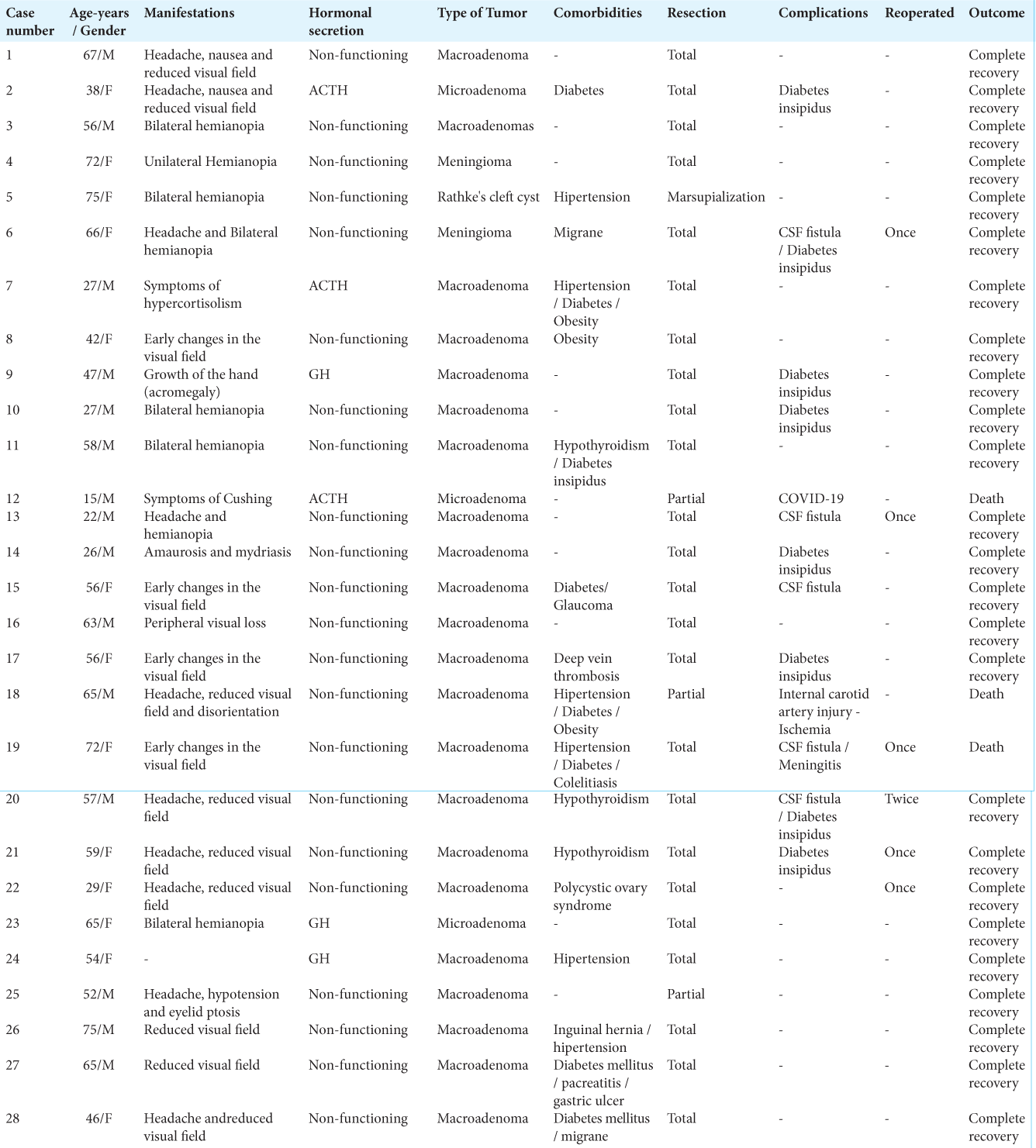
This study described 28 patients and 35 surgical procedures using the EETA between May 2020 and July 2022. Data are resumed in
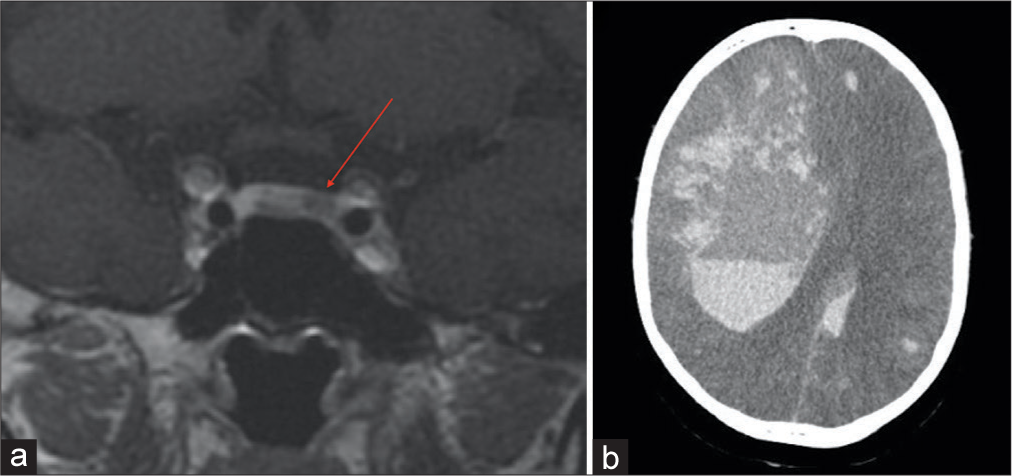
There was one case of COVID-19-related complication: a 15-year-old boy diagnosed with Cushing disease (preoperative cortisol 63.4 µg/dL) was admitted and the magnetic resonance imaging of sella turcica exhibited a right nodular pituitary lesion, measuring 2.0 × 1.5 mm [
DISCUSSION
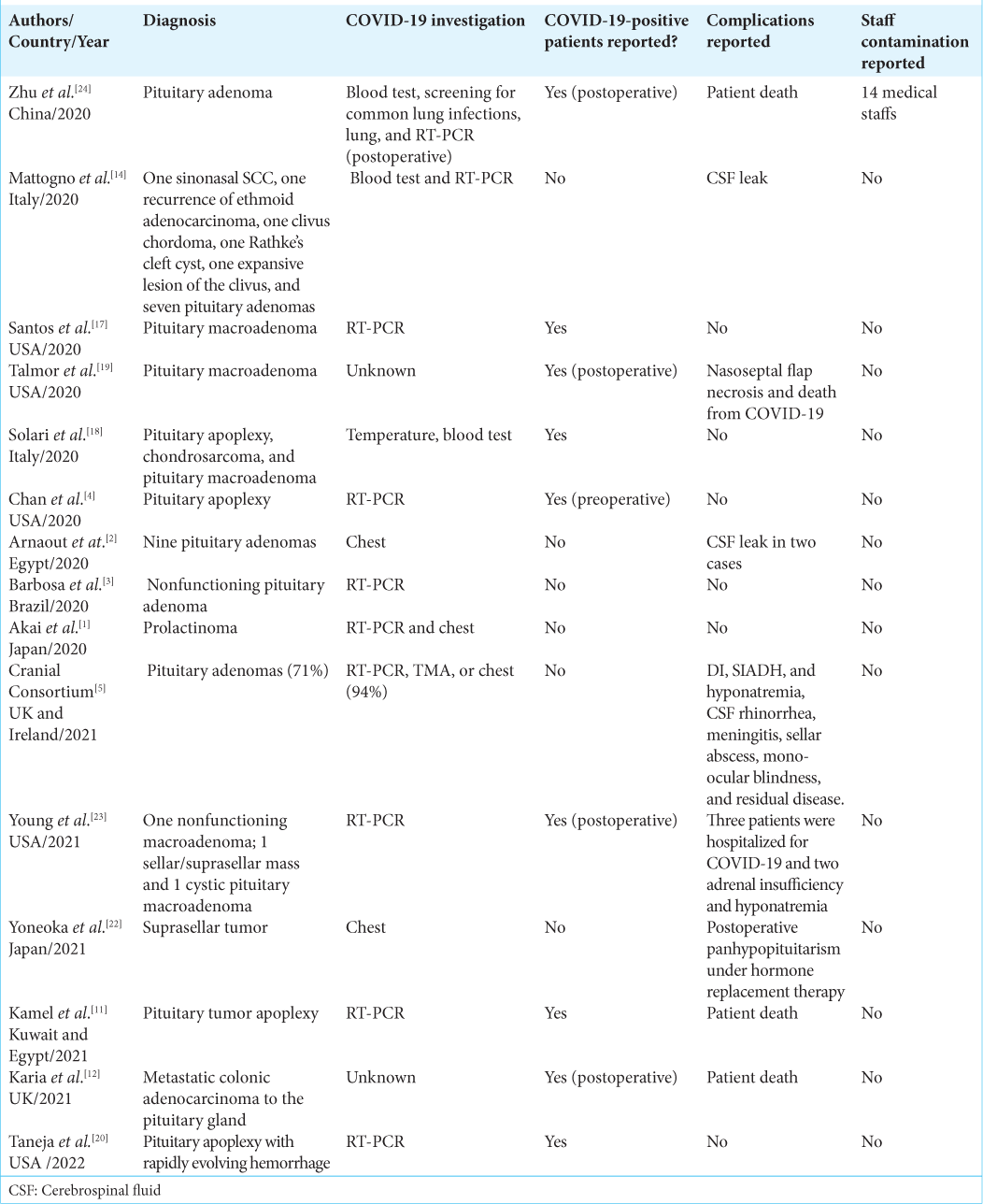
Some reference centers worldwide during the COVID-19 pandemic developed local protocols to perform ETTA safely. Most patients underwent urgent pituitary surgery due to chiasm compression, severe hormonal dysfunction, pituitary apoplexy, or refractory headache.[
Different surgical strategies were implemented in COVID-19-negative patients. Arnaout et al. (Egypt)[
There were different protocols for COVID-19-positive patients: (a) simulation trainees before the skull base surgery;[
Regarding surgical complications[
To date, the surgical team implemented a recent aggressive strategy trying to achieve gross total resection. This includes an extended approach with a large sphenoid sinus/sellar floor opening; extensive tumor dissection raising the risk of sellar roof opening; and CSF fistula. To overcome these complications, especially the CSF leak, multiple layers for skull base reconstruction with nasoseptal flap and fat-fascia graft were used. Regarding the COVID-19 pandemic and skull base surgery, there are no definitive data about complications rates.
One patient suffered from COVID-19 4 days after the surgery. It was not possible to identify the infection source; however, as a pediatric patient, there was an obligation to have a companion during hospitalization increasing the patient exposure. To date, the companion admission RT-PCR was negative. On the 4th postoperative day, the parent tested positive. The cause of the COVID-19-related death in this case series was not identified. It is possible that the hypercoagulability state of Cushing disease could have influenced the course of COVID-19 infection.
CONCLUSION
Our institutional protocol to perform EETA during COVID-19 pandemic was easy to implement and the pituitary surgeries were maintained during the pandemic only to treat critical cases. Nevertheless, the protocols should be continually updated for greater patient and health-care professional safety.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
The authors received financial support from FAPERJ – Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro and NIPNAC – Center of High Complexity Neurosurgery Intern Patients from Rio de Janeiro State Department of Health.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akai T, Maruyama K, Takakura H, Yamamoto Y, Morinaga Y, Kuroda S. Safety management in urgent endonasal transsphenoidal surgery for pituitary adenoma during the COVID-19 pandemic in Japan-a case report. Interdiscip Neurosurg. 2020. 22: 100820
2. Arnaout MM, Bessar AA, Elnashar I, Abaza H, Makia M. Pituitary adenoma surgeries in COVID-19 era: Early local experience from Egypt. Surg Neurol Int. 2020. 11: 363
3. Barbosa D, Oberman D, Moreira A, Borges L, Goncalves F. Endonasal endoscopic pituitary adenoma resection in light of the COVID-19 pandemic: A technical report. Arq Bras Neuroci. 2021. 40: 82-5
4. Chan JL, Gregory KD, Smithson SS, Naqvi M, Mamelak AN. Pituitary apoplexy associated with acute COVID-19 infection and pregnancy. Pituitary. 2020. 23: 716-20
5. Cranial Consortium. CSF rhinorrhea after endonasal intervention to the skull base (CRANIAL)-part 2: Impact of COVID-19. World Neurosurg. 2021. 149: e1090-7
6. Erber J, Kappler V, Haller B, Mijočević H, Galhoz A, Da Costa C. Infection control measures and prevalence of SARS-CoV-2 IgG among 4,554 university hospital employees, Munich, Germany. Emerg Infect Dis. 2022. 28: 572-81
7. Esposito D, Olsson DS, Ragnarsson O, Buchfelder M, Skoglund T, Johannsson G. Non-functioning pituitary adenomas: Indications for pituitary surgery and post-surgical management. Pituitary. 2019. 22: 422-34
8. Fang J, Xie S, Li N, Jiang Z. Postoperative complications of endoscopic versus microscopic transsphenoidal pituitary surgery: A meta-analysis. J Coll Physicians Surg Pak. 2018. 28: 554-9
9. Fleseriu M, Buchfelder M, Cetas JS, Fazeli PK, Mallea-Gil SM, Gurnell M. Pituitary society guidance: Pituitary disease management and patient care recommendations during the COVID-19 pandemic-an international perspective. Pituitary. 2020. 23: 327-37
10. Halvorsen H, Ramm-Pettersen J, Josefsen R, Rønning P, Reinlie S, Meling T. Surgical complications after transsphenoidal microscopic and endoscopic surgery for pituitary adenoma: A consecutive series of 506 procedures. Acta Neurochir (Wien). 2014. 156: 441-9
11. Kamel WA, Najibullah M, Saleh MS, Azab WA. Coronavirus disease 2019 infection and pituitary apoplexy: A causal relation or just a coincidence? A case report and review of the literature. Surg Neurol Int. 2021. 12: 317
12. Karia K, Price SA, Soon WC, Chowdhury YA, Thant KZ, Batra R. Metastatic colon cancer in the pituitary: A case report with review of literature. Asian J Neurosurg. 2021. 16: 872-5
13. Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of giant pituitary adenomas. Pituitary. 2012. 15: 150-9
14. Mattogno PP, Rigante M, Lauretti L, Parrilla C, D’Alessandris QG, Paludetti G. Transnasal endoscopic skull base surgery during COVID-19 pandemic: Algorithm of management in an Italian reference COVID center. Acta Neurochir (Wien). 2020. 162: 1783-5
15. Pandey AS, Ringer AJ, Rai AT, Kan P, Jabbour P, Siddiqui AH. Minimizing SARS-CoV-2 exposure when performing surgical interventions during the COVID-19 pandemic. J Neurointerv Surg. 2020. 12: 643-7
16. Quillin JW, Oyesiku NM. Status of pituitary surgery during the COVID-19 pandemic. Neurol India. 2020. 68: S134-6
17. Santos CD, Filho LM, Santos CA, Neill JS, Vale HF, Kurnutala LN. Pituitary tumor resection in a patient with SARS-CoV-2 (COVID-19) infection. A case report and suggested airway management guidelines. Braz J Anesthesiol. 2020. 70: 165-70
18. Solari D, Bove I, Esposito F, Cappabianca P, Cavallo LM. The nose lid for the endoscopic endonasal procedures during COVID-19 era: Technical note. Acta Neurochir (Wien). 2020. 162: 2335-9
19. Talmor G, Grube JG, Eloy JA, Liu JK, Hsueh WD. Nasoseptal flap necrosis after endoscopic skull base surgery in the setting of COVID-19 pandemic. World Neurosurg. 2020. 140: 374-7
20. Taneja C, Fazeli PK, Gardner PA, Wang EW, Snyderman CH. Rapidly progressive pituitary apoplexy in a patient with COVID-19 disease treated with endoscopic endonasal surgery. J Neurol Surg Rep. 2022. 83: e8-e12
21. Van Gerven L, Qian Z, Starovoyt A, Jorissen M, Meulemans J, Van Loon J. Endoscopic, endonasal transsphenoidal surgery for tumors of the sellar and suprasellar region: A monocentric historical cohort study of 369 patients. Front Oncol. 2021. 11: 643550
22. Yoneoka Y, Seki Y, Akiyama K, Sakurai Y, Ohara N, Hasegawa G. Prolonged postoperative pyrexia and transient nonnephrogenic vasopressin-analogue-resistant polyuria following endoscopic transsphenoidal resection of an infundibular epidermoid cyst. Case Rep Neurol Med. 2021. 2021: 6690372
23. Young JS, Oh T, Arora T, Blevins LS, Aghi MK, El-Sayed IH. Letter: COVID conundrum: Postoperative COVID-19 infections following endonasal transsphenoidal pituitary surgery. Neurosurgery. 2021. 88: E571-2
24. Zhu W, Huang X, Zhao H, Jiang X. A COVID-19 patient who underwent endonasal endoscopic pituitary. Adenoma resection: A case report. Neurosurgery. 2020. 87: E140-6