- Department of Surgery, Section of Neurosurgery, Aga Khan University Hospital, Karachi, Pakistan
Correspondence Address:
Muhammad Ehsan Bari
Department of Surgery, Section of Neurosurgery, Aga Khan University Hospital, Karachi, Pakistan
DOI:10.4103/2152-7806.161785
Copyright: © 2015 Khan MB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Khan MB, Riaz M, Bari ME. Multiple cerebral hydatid cysts in 8-year-old boy: A case report and literature review of a rare presentation. Surg Neurol Int 29-Jul-2015;6:125
How to cite this URL: Khan MB, Riaz M, Bari ME. Multiple cerebral hydatid cysts in 8-year-old boy: A case report and literature review of a rare presentation. Surg Neurol Int 29-Jul-2015;6:125. Available from: http://surgicalneurologyint.com/surgicalint_articles/multiple-cerebral-hydatid-cysts-in-8%e2%80%91year%e2%80%91old-boy-a-case-report-and-literature-review-of-a-rare-presentation/
Abstract
Background:Multiple cerebral hydatid cysts are very rare with only a few reports in the literature detailing diagnostic workup, medical management, surgical techniques, possible complications, and outcomes.
Case Description:We present the case of an 8-year-old boy who presented with progressively worsening headaches, vomiting, and intermittent fever since 20 days. Diagnostic workup was performed, and magnetic resonance imaging revealed multiple intracranial cysts predominantly in the right frontal region with significant mass effect. A total of 19 intracranial cysts were removed surgically, and the child recovered uneventfully.
Conclusions:Neurosurgeons should keep hydatidosis in the list of differentials when evaluating patients with cystic diseases of the brain. Although the removal of such cysts is challenging, outcomes are excellent when cysts are evacuated without rupture and patients show complete resolution of symptoms.
Keywords: Albendazole, Echinococcus, hydatid cysts, intracranial, surgical excision
INTRODUCTION
Infection with Echinococcus larvae causes hydatid disease in humans.[
Here, we report the case of an 8-year-old boy with 19 intracranial cysts, which were successfully removed surgically and also review the literature with an emphasis on diagnosis and management of patients with multiple cerebral cysts.
CASE REPORT
This 8-year-old boy presented with complaints of progressively worsening headaches along with vomiting and intermittent fever since 20 days. There were no significant findings on general physical and neurological examination. The patient's routine laboratory investigations were normal. A magnetic resonance imaging (MRI) brain was performed which showed multiple intracranial cysts predominantly in the right frontal region with significant mass effect [
Figure 1
(a) T1-weighted magnetic resonance imaging axial section demonstration multiple cysts generating a hypointense signal. Multiple septations can be appreciated significant mass effect can be appreciated. (b) T2-weighted magnetic resonance imaging axial section representing multiple cysts with a hyperintense signal and the cyst walls generating a hypointense signal. (c) T1-contrast enhanced magnetic resonance imaging axial cut showing contrast enhancement of the cyst wall in some regions. (d) Fluid attenuated inversion recovery sequence coronal section showing multiple cysts as hypointense signals and significant mass effect
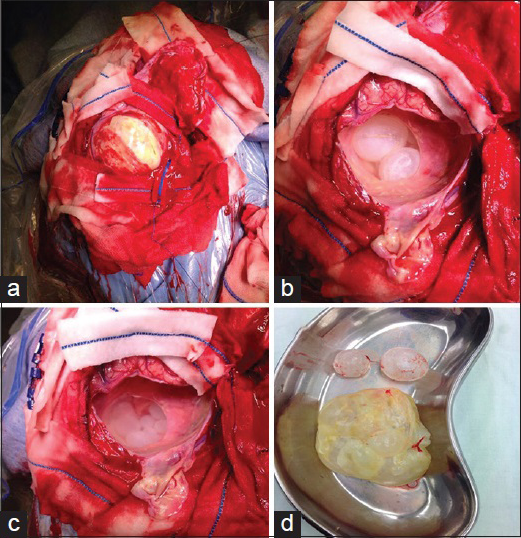
A frontoparietal craniotomy was performed. There was significant dural tension, and a c-shaped durotomy was done which revealed a huge hydatid cyst extending toward the lateral ventricle [
The patient continued taking albendazole (200 mg, BID), dexamethasone, cefazolin, and levetiracetam postoperatively and had an uneventful postoperative course. The patient was seen in clinic on 3 months postoperative visit and his complaints of headache and vomiting had completely resolved. His neurological examination was completely normal and considering financial constraints a follow-up computed tomography (CT) scan was thus not performed.
DISCUSSION
Hydatid disease is a potentially fatal parasitic infection that can affect wildlife animals, commercial stock, and humans.[
A viable primary lesion could rupture spontaneously or due to trauma or surgery. The spillage of the scolices in the brain parenchyma results in multiple secondary hydatid cysts.[
Both CT and MRI scan have been reported to be useful in the correct preoperative diagnosis of cerebral hydatid cysts.[
Serological tests have traditionally had low sensitivity and specificity in diagnosing intracerebral hydatid cysts.[
Successful medical treatment of liver and abdominal hydatid cysts with albendazole, mebendazole, and praziquantel has been well reported in the literature.[
CONCLUSION
Neurosurgeons should keep hydatidosis in the list of differentials when evaluating patients with cystic diseases of the brain. An MRI can greatly aid in diagnosis and surgical planning. The goal of surgery should be total excision of intact cyst which should be followed by antibiotic and antihelminthic treatment to avoid recurrence. Surgical outcomes are excellent, and patients show complete resolution of symptoms after complete excision of the cyst.
References
1. Boles DM. Cerebral echinococciasis. Surg Neurol. 1981. 16: 280-2
2. Bükte Y, Kemaloglu S, Nazaroglu H, Ozkan U, Ceviz A, Simsek M. Cerebral hydatid disease: CT and MR imaging findings. Swiss Med Wkly. 2004. 134: 459-67
3. Cavusoglu H, Tuncer C, Ozdilmaç A, Aydin Y. Multiple intracranial hydatid cysts in a boy. Turk Neurosurg. 2009. 19: 203-7
4. Diren HB, Ozcanli H, Boluk M, Kilic C. Unilocular orbital, cerebral and intraventricular hydatid cysts: CT diagnosis. Neuroradiology. 1993. 35: 149-50
5. Duishanbai S, Jiafu D, Guo H, Liu C, Liu B, Aishalong M. Intracranial hydatid cyst in children: Report of 30 cases. Childs Nerv Syst. 2010. 26: 821-7
6. Gana R, Skhissi M, Maaqili R, Bellakhdar F. Multiple infected cerebral hydatid cysts. J Clin Neurosci. 2008. 15: 591-3
7. Martín Oterino JA, Chimpén Ruiz VA, Reviriego Jaén G, Sánchez Rodríguez A. Repeated strokes as a sign of multiple cerebral hydatid cysts. Neurologia. 1996. 11: 307-9
8. Pasaoglu A, Orhon C, Akdemir H. Multiple primary hydatid cysts of the brain. Turk J Pediatr. 1989. 31: 57-61
9. Sen N, Laha D, Gangopadhyay PK, Mohanty BC. Young girl with multiple intracranial hydatid cyst. Ann Neurosci. 2012. 19: 96-8
10. Todorov T, Vutova K, Petkov D, Balkanski G. Albendazole treatment of multiple cerebral hydatid cysts: Case report. Trans R Soc Trop Med Hyg. 1988. 82: 150-2
11. Tüzün M, Hekimoglu B. Hydatid disease of the CNS: Imaging features. AJR Am J Roentgenol. 1998. 171: 1497-500
12. Vaquero J, Jiménez C, Martínez R. Growth of hydatid cysts evaluated by CT scanning after presumed cerebral hydatid embolism. Case report. J Neurosurg. 1982. 57: 837-8
13. Yüceer N, Güven MB, Yilmaz H.editors. Multiple hydatid cysts of the brain: A case report and review of the literature. Neurosurg Rev. 1998. 21: 181-4
14. Yurt A, Avci M, Selçuki M, Ozer F, Camlar M, Uçar K. Multiple cerebral hydatid cysts. Report of a case with 24 pieces. Clin Neurol Neurosurg. 2007. 109: 821-6