- Department of Neurosurgery, Allama Iqbal Medical College, Jinnah Hospital, Lahore, Pakistan,
- Wolfson School of Medicine, University of Glasgow, Glasgow, Scotland, United Kingdom,
- School of Medicine, King Edward Medical University, Lahore, Punjab, Pakistan,
- Administration, Allama Iqbal Medical College, Jinnah Hospital, Lahore, Pakistan.
Correspondence Address:
Usman Ahmad Kamboh, Department of Neurosurgery, Allama Iqbal Medical College, Jinnah Hospital Lahore, Lahore, Pakistan.
DOI:10.25259/SNI_314_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Usman Ahmad Kamboh1, Mohammad Ashraf1,2, Shah Gul Zahra3, Muhammad Asif Raza1, Mehwish Manzoor4, Mehreen Mehboob1, Minaam Farooq3, Manzoor Ahmad1, Syed Shahzad Hussain1, Naveed Ashraf1. Outcome of surgical treatment for neglected congenital muscular torticollis: A series of 28 adolescent patients. 08-Jul-2022;13:292
How to cite this URL: Usman Ahmad Kamboh1, Mohammad Ashraf1,2, Shah Gul Zahra3, Muhammad Asif Raza1, Mehwish Manzoor4, Mehreen Mehboob1, Minaam Farooq3, Manzoor Ahmad1, Syed Shahzad Hussain1, Naveed Ashraf1. Outcome of surgical treatment for neglected congenital muscular torticollis: A series of 28 adolescent patients. 08-Jul-2022;13:292. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11708
Abstract
Background: Congenital muscular torticollis (CMT) is a common musculoskeletal anomaly that can be excellently managed at birth with conservative physiotherapy; as a result, literature on neglected cases of CMT in older patients is sparse, and there is controversy regarding the ideal surgical approach. This report aims to provide the outcome of 28 adolescent patients with neglected CMT who underwent unipolar release at the distal sternocleidomastoid muscle (SCM).
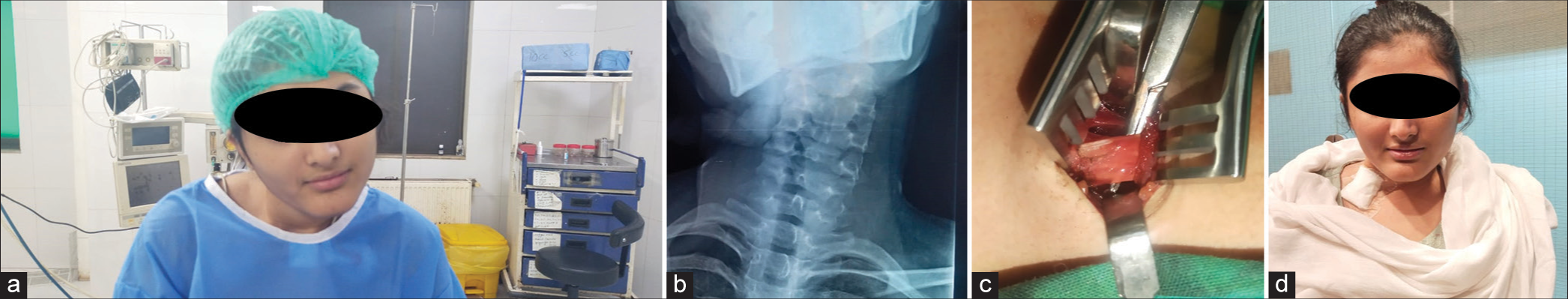
Methods: Twenty-eight adolescent patients with untreated CMT presented to our department between 2016 and 2019 and underwent unipolar release at the distal end of their SCM. All patients had no other anomaly based on clinical examination and radiological investigations. At the time of surgery, the mean age of patients was 15.8 years (range 13–18 years). There were 10 male and 18 female patients with the right side affected in 20 cases. All patients were followed up for 2 years. Patients were evaluated using an adapted version of the modified Lee’s scoring system to assess cosmesis and the cervical-mandibular angle (CMA) to assess radiological change.
Results: The adapted modified Lee’s scoring system indicated 17 patients (60.7%) had an excellent outcome, 6 patients (21.4%) had a good outcome, and 5 patients (17.9%) had a fair outcome. In particular, scarring was fine in 23 patients (82.1%) and only slight in the remaining. Independent to the categorical outcome, all patients subjectively reported high satisfaction with their cosmesis. The preoperative mean CMA was 19.6° (range, 8.5–31.5°), which was reduced to a mean of CMA of 14.0° (range, 3–28°) after surgery (P
Conclusion: In uncomplicated cases of neglected CMT in adolescent patients, unipolar tenotomy of the distal SCM is a safe and reliable technique with good clinical outcomes.
Keywords: Adolescent, Congenital muscular torticollis, Neglected torticollis, Sternocleidomastoid muscle, Unipolar release
INTRODUCTION
Torticollis is a Latin word that means twisted neck. First, Tubby in 1912 defined it as “a deformity, congenital, or acquired, characterized by a lateral inclination of the head to the shoulder, with torsion of the neck and deviation of the face.”[
Congenital muscular torticollis (CMT) is the third most common congenital musculoskeletal anomaly after dislocation of the hip and clubfoot.[
When diagnosed early, it is accepted that torticollis can be managed with good or excellent results using conservative physiotherapy.[
MATERIALS AND METHODS
This study was a prospective case series approved by our institutional review board and conducted at our neurosurgery department between 2016 and 2019. All images attached are with informed consent. We enrolled all patients who presented to our outpatient clinic with neglected congenital torticollis. All patients underwent a detailed neurological history and examinations and were advised relevant investigations including X-ray cervical spine and MRI with cervical-medullary junction. X-ray cervical spine was obtained for all patients to determine if a CT scan should be obtained, if a craniovertebral anomaly was suspected. Investigations and imaging were to ensure all cases could be labeled as CMT and other causes could be excluded from the study. All patients were followed up at their 2-year clinic visit.
Inclusion and exclusion criteria
Patients of both sexes were aged 13–18 years. Congenital torticollis with head tilt toward the affected side and tight band in the ipsilateral SCM. Absence of any other abnormality in the neck as assessed on radiological imaging, including hindbrain herniation, cervical spine lesions, syringomyelia, and cervical spine and neck infection. No previous medical or surgical treatment has been received for torticollis.
Surgical procedure and postoperative management
All patients underwent a uniform operative technique of unipolar release of the lower end of SCM by the same neurosurgeon. Patients were positioned supine with their heads rotated toward the side opposite to torticollis. A transverse skin crease incision is marked 3 cm above the sternoclavicular end of the SCM. The skin and subcutaneous tissue were incised in the incision line, and the platysma was cut open. The lower end of the SCM was identified, and the sternal and clavicular head were released at the inferior end. The range of neck motion was also assessed at the inferior end, and the wound was closed in layers. Following surgery, manual stretching and rehabilitation of a cervical range of motion were performed by rehabilitation in the department twice daily, with each session lasting 30 min, for 3 days. On the 3rd postoperative day, all patients were discharged with the advice to continue manual stretching for 3 months and self-mirroring. Patients were advised a cervical collar for 3 months postoperatively.
Outcome assessment
The outcomes in this series were assessed using the cervicalmandibular angle (CMA) and an adapted version of the modified Lee’s criteria.[
An adapted version of the modified Lee’s scoring system[
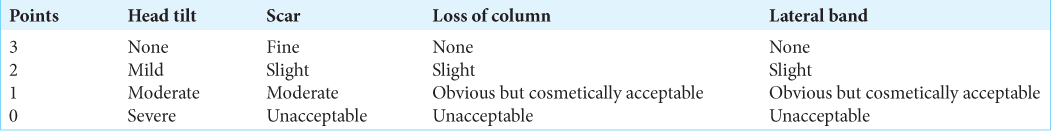
Table 1:
Assessing cosmesis using our adapted version of the modified Lee’s score.[
Outcome was categorized as follows:
Excellent: a score of 11 or 12 Good: a score of 9 or 10 Fair: a score <9.
Statistical Package for the Social Sciences Version 27 IMB was used to analyze the results. The CMA at baseline was compared to that at 2-year follow-up. P < 0.05 was considered statistically significant.
RESULTS
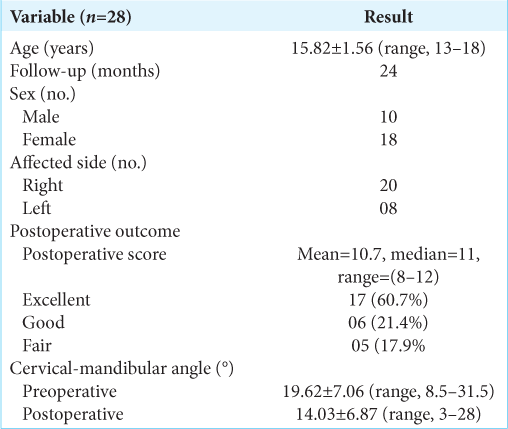
A total of 28 patients were studied, including 10 males and 18 females. The mean age was 15.82 ± 1.56 (13–18 years). The right side was affected in 20 patients, while the left side was affected in 8. All patients were evaluated at a 2-year clinic follow-up [
DISCUSSION
Most CMT cases resolve completely spontaneously within months after birth or with conservative measures initiated early, such as gentle controlled passive manual stretching exercises on the affected side. Sönmez et al. found that 95% of patients diagnosed and treated effectively before age 1 year did not need surgical treatment.[
The timing of surgery is controversial. Canale et al.[
Concerning adolescent and younger patients, age, head tilt, scar formation, and craniofacial asymmetry are important parameters determining outcomes after surgery.[
Our study also showed good surgical results in adolescent patients with neglected CMT and no other abnormalities. In our series of adolescent patients treated with simple unipolar release, over 80% of patients had either an excellent or good result with no complications. We opted for a unipolar resection at the distal end of the SCM; rotation and lateral flection on the left side improved, and SCM tension disappeared during surgery. Excellent results were found in 60.7% of patients and good results in 21.4%. No significant complications and recurrences were observed in any patients. In the study by Canale et al., noticeable cosmetic deformity was observed in approximately 31% of patients.[
The satisfaction rate in the follow-up was above 85%, even in those with a fair outcome. This is similar to Lee et al.’s[
CONCLUSION
Adolescent patients with neglected CMT benefit from unipolar SCM release at the distal end. The surgery restores the range of neck motion, resolves the head tilt, has minimum scarring, and greatly improves cosmesis, thus significantly improving the patient’s quality of life. All patients were greatly satisfied with their outcome, independent of whose outcome was clinically classified as excellent, good, or fair. Therefore, the unipolar release of the SCM is a safe and effective technique in adolescent patients with neglected CMT.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akazawa H, Nakatsuka Y, Miyake Y, Takahashi Y. Congenital muscular torticollis: Long-term follow-up of thirty-eight partial resections of the sternocleidomastoid muscle. Arch Orthop Trauma Surg. 1993. 112: 205-9
2. Canale S, Griffin D, Hubbard C. Congenital muscular torticollis. A long-term follow-up. J Bone Joint Surg Am. 1982. 64: 810-6
3. Chen CE, Ko JY. Surgical treatment of muscular torticollis for patients above 6 years of age. Arch Orthop Trauma Surg. 2000. 120: 149-51
4. Cheng J, Tang S. Outcome of surgical treatment of congenital muscular torticollis. Clin Orthop Relat Res. 1999. 362: 190-200
5. Cheng J, Wong M, Tang S, Chen T, Shum S, Wong E. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants: A prospective study of eight hundred and twenty-one cases. J Bone Joint Surg Am. 2001. 83: 679-87
6. Do TT. Congenital muscular torticollis: Current concepts and review of treatment. Curr Opin Pediatr. 2006. 18: 26-9
7. Ferkel RD, Westin GW, Dawson EG, Oppenheim WL. Muscular torticollis. A modified surgical approach. J Bone Joint Surg Am. 1983. 65: 894-900
8. Gill S, Nagi O, Gakhar H. Bipolar release for neglected and relapsed cases of congenital muscular torticollis. Indian J Orthop. 2005. 39: 45
9. Ippolito E, Tudisco C. Idiopathic muscular torticollis in adults. Arch Orthop Trauma Surg. 1986. 105: 49-54
10. Lee E, Kang Y, Bose K. Surgical correction of muscular torticollis in the older child. J Pediatr Orthop. 1986. 6: 585-9
11. Lee GS, Lee MK, Kim WJ, Kim HS, Kim JH, Kim YS. Adult patients with congenital muscular torticollis treated with bipolar release: Report of 31 cases. J Korean Neurosurg Soc. 2017. 60: 82
12. Lee IJ, Lim SY, Song HS, Park MC. Complete tight fibrous band release and resection in congenital muscular torticollis. J Plast Reconstr Aesthet Surg. 2010. 63: 947-53
13. Lim KS, Shim JS, Lee YS. Is sternocleidomastoid muscle release effective in adults with neglected congenital muscular torticollis?. Clin Orthop Relat Res. 2014. 472: 1271-8
14. Ling C. The influence of age on the results of open sternomastoid tenotomy in muscular torticollis. Clin Orthop Relat Res. 1976. 116: 142-8
15. Minamitani K, Inoue A, Okuno T. Results of surgical treatment of muscular torticollis for patients greater than 6 years of age. J Pediatr Orthop. 1990. 10: 754-9
16. Oh I, Nowacek CJ. Surgical release of congenital torticollis in adults. Clin Orthop Relat Res. 1978. 131: 141-5
17. Omidi-Kashani F, Hasankhani EG, Sharifi R, Mazlumi M. Is surgery recommended in adults with neglected congenital muscular torticollis? A prospective study. BMC Musculoskelet Disord. 2008. 9: 158
18. Patwardhan S, Shyam A, Sancheti P, Arora P, Nagda T, Naik P. Adult presentation of congenital muscular torticollis: A series of 12 patients treated with a bipolar release of sternocleidomastoid and Z-lengthening. J Bone Joint Surg Br. 2011. 93: 828-32
19. Petronic I, Brdar R, Cirovic D, Nikolic D, Lukac M, Janic D. Congenital muscular torticollis in children: Distribution, treatment duration and out come. Eur J Phys Rehabil Med. 2010. 46: 153-7
20. Sönmez K, Türkyilmaz Z, Demiroğulları B, Ozen IO, Karabulut R, Bağbanci B. Congenital muscular torticollis in children. ORL J Otorhinolaryngol Relat Spec. 2005. 67: 344-7
21. Tubby AH.editors. Deformities, Including Diseases of the Bones and Joints: A Text-book of Orthopaedic Surgery. New York: Macmillan and Company, Limited; 1912. Vol. 2:
22. Yuan B, Qu F, Zhao G, Wang J, Shen X, Liu Y. Arthroscopic surgical treatment for neglected congenital muscular torticollis in adults. J Craniofac Surg. 2015. 26: 512-5