- Department of Neurosurgery, Tufts Medical Center, Washington, Boston, United States.
- Department of Anesthesiology, Tufts Medical Center, Washington, Boston, United States.
Correspondence Address:
James Kryzanski, Department of Neurosurgery, Tufts Medical Center, Washington, Boston, United States.
DOI:10.25259/SNI_25_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Caitlin Keenan1, Andy Y. Wang1, Konstantin Balonov2, James Kryzanski1. Postoperative vasovagal cardiac arrest after spinal anesthesia for lumbar spine surgery. 11-Feb-2022;13:42
How to cite this URL: Caitlin Keenan1, Andy Y. Wang1, Konstantin Balonov2, James Kryzanski1. Postoperative vasovagal cardiac arrest after spinal anesthesia for lumbar spine surgery. 11-Feb-2022;13:42. Available from: https://surgicalneurologyint.com/surgicalint-articles/11388/
Abstract
Background: Spinal anesthesia is being increasingly recognized as a favorable alternative to general anesthesia. However, there are still several considerations for its safe and effective use.
Case Description: A 62-year-old male received spinal anesthesia during an uneventful L3-L5 decompressive laminectomy. However, he subsequently experienced a brief episode of pulseless electrical activity in the post-anesthesia care unit, and was successfully resuscitated without further sequelae. This was attributed to a vasovagal episode, with his notable prior history of experiencing vasovagal syncope with lightheadedness and fainting at the sight of blood.
Conclusion: Patients with a history of vasovagal syncope may be predisposed to experiencing brief potentiated episodes of severe bradycardia and even cardiac arrest following spinal anesthesia.
Keywords: Cardiac arrest, Lumbar spine, Pulseless electrical activity, Spinal anesthesia, Vasovagal
INTRODUCTION
Spinal anesthesia during lumbar surgery is a safe and effective alternative to general anesthesia for patients across a wide range of ages and health statuses.[
CASE DESCRIPTION
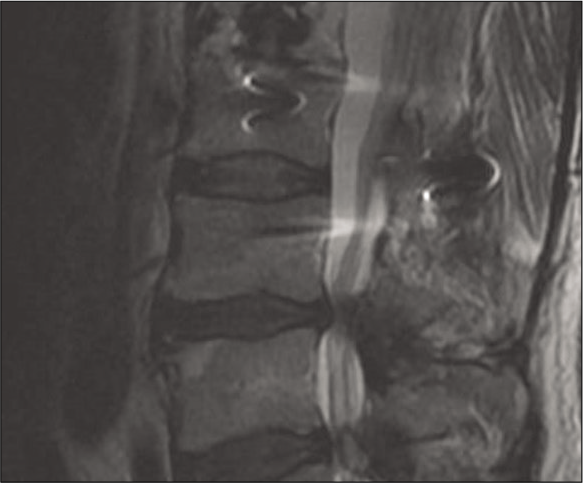
A 62-year-old male presented with progressive/severe neurogenic claudication. He had a previous L1 burst fracture with fusion surgery 10 years prior, and now has severe L3/L4 and L4/L5 spinal stenosis on imaging [
DISCUSSION
Here, we present the case of a 62-year-old male who experienced brief PEA arrest in the PACU after an uneventful lumbar surgery under spinal anesthesia. This episode was attributed to a vasovagal reflex (also known as the BezoldJarisch reflex or neurocardiogenic syncope).[
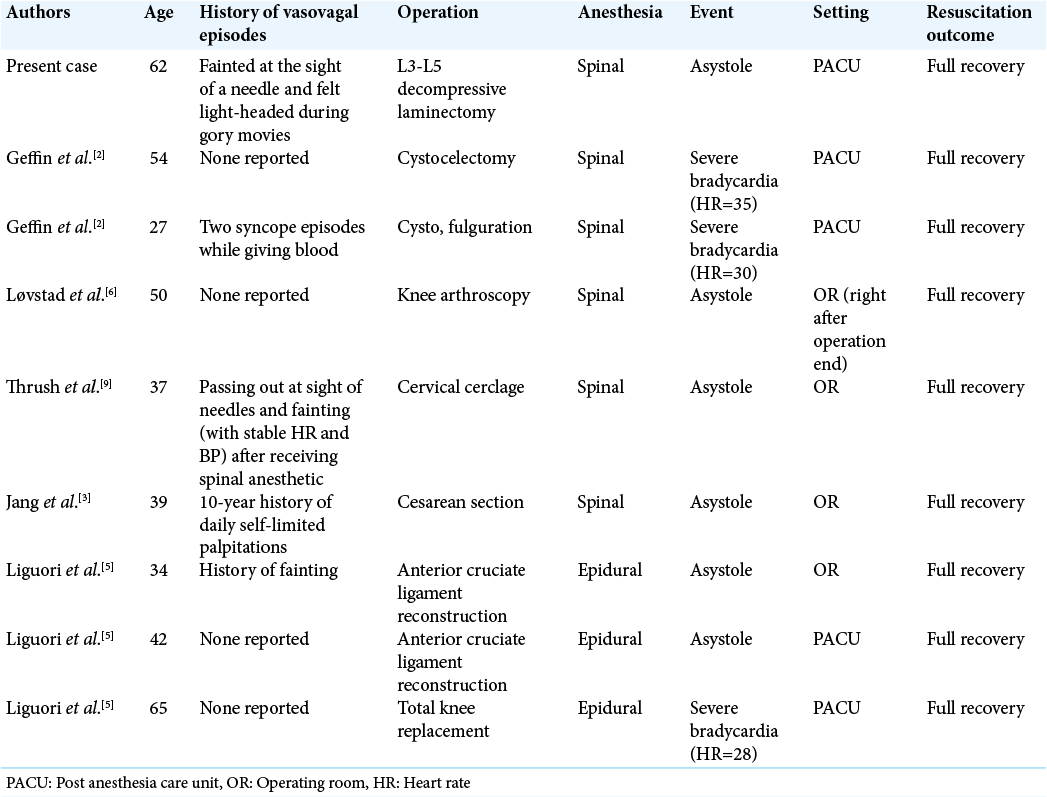
There is precedent in the literature for patients with a history of vasovagal episodes experiencing similar events under regional anesthesia [
Kinsella et al. offer several suggestions for avoiding vasovagal arrest under spinal anesthesia.[
CONCLUSION
This case report describes an episode of vasovagal cardiac arrest occurring in the PACU following spinal anesthesia for lumbar stenosis surgery, and we recommend asking patients about their history of vasovagal events to gain some insight into their risk for vasovagal complications such as PEA following spinal anesthesia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Breton JM, Ludwig CG, Yang MJ, Nail TJ, Riesenburger RI, Liu P. Spinal anesthesia in contemporary and complex lumbar spine surgery: Experience with 343 cases. J Neurosurg Spine. 2021. p. 1-8
2. Geffin B, Shapiro L. Sinus bradycardia and asystole during spinal and epidural anesthesia: A report of 13 cases. J Clin Anesth. 1998. 10: 278-85
3. Jang YE, Do SH, Song IA. Vasovagal cardiac arrest during spinal anesthesia for Cesarean section-a case report. Korean J Anesthesiol. 2013. 64: 77-81
4. Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: Relationship to vasovagal syncope and the Bezold-Jarisch reflex. Br J Anaesth. 2001. 86: 859-68
5. Liguori GA, Sharrock NE. Asystole and severe bradycardia during epidural anesthesia in orthopedic patients. Anesthesiology. 1997. 86: 250-7
6. Løvstad RZ, Granhus G, Hetland S. Bradycardia and asystolic cardiac arrest during spinal anaesthesia: A report of five cases. Acta Anaesthesiol Scand. 2000. 44: 48-52
7. Mackey DC, Carpenter RL, Thompson GE, Brown DL, Bodily MN. Bradycardia and asystole during spinal anesthesia: A report of three cases without morbidity. Anesthesiology. 1989. 70: 866-8
8. Pollard JB. Cardiac arrest during spinal anesthesia: Common mechanisms and strategies for prevention. Anesth Analg. 2001. 92: 252-6
9. Thrush DN, Downs JB. Vagotonia and cardiac arrest during spinal anesthesia. Anesthesiology. 1999. 91: 1171-3