- Department of Neurosurgery, Saudi German Hospital, Ajman, United Arab Emirates,
- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq
- Department of Neurosurgery, University of Al-Nahrain, College of Medicine, Baghdad, Iraq
- Department of Neurosurgery, University of Fallujah, College of Medicine, Al Anbar, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
DOI:10.25259/SNI_918_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Al-Mutasim B. Etaiwi1, Mustafa Ismail2, Teeba A. Al-Ageely2, Ayaat F. Alasady3, Alsultan O. Jabbar4, Jaafar AbdulWahid3, Mahmood F. Al-Zaidy2, Samer S. Hoz5. Retrograde cranio-orbital penetrating injury: A case report. 13-Jan-2023;14:11
How to cite this URL: Al-Mutasim B. Etaiwi1, Mustafa Ismail2, Teeba A. Al-Ageely2, Ayaat F. Alasady3, Alsultan O. Jabbar4, Jaafar AbdulWahid3, Mahmood F. Al-Zaidy2, Samer S. Hoz5. Retrograde cranio-orbital penetrating injury: A case report. 13-Jan-2023;14:11. Available from: https://surgicalneurologyint.com/surgicalint-articles/12102/
Abstract
Background: Transorbital (Orbito-cranial) injuries are uncommon, but they are among the most debilitating types of traumatic brain injury (TBI), mainly caused by high-velocity gunshot wounds. In addition, the management of transorbital TBI is well documented in the literature. In contrast, the cranio-orbital migration of a bullet following TBI is rarely reported. In this article, we report a reverse cranio-orbital penetration of a bullet after a TBI from the occiput with a discussion about its management.
Case Description: A 34-year-old male presented with a loss of consciousness to the emergency department. His Glasgow Coma Scale was 10 (E3, V3, M4), with a left-sided weakness grade of 3 on the Medical Research Council of Canada scale. A head computed tomography (CT) scan was performed, which revealed a bullet embedded in the right orbit with an entrance point from the right occipital bone. Moreover, the CT scan showed an intraventricular hemorrhage in the lateral ventricle. The surgery was performed where the hematoma was evacuated, the scalp was debrided, and the bullet was removed successfully. However, the patient died on the 7th postoperatively.
Conclusion: Cranio-orbital penetrating brain injury is a severe yet rare type of penetrating brain injury. The direction of cranio-orbital injury is usually from the orbital region to the cerebrum. In our case, the retrograde fashion of the bullet migration renders it unique and calls for further studies to highlight the differences in injury and management of such cases.
Keywords: Cranio-orbital, TBI, Traumatic brain injury
INTRODUCTION
Penetrating head injury represents one of the most severe traumatic brain injuries (TBIs). They account for the majority of brain injuries and cause a high death rate in the civilian population.[
CASE PRESENTATION
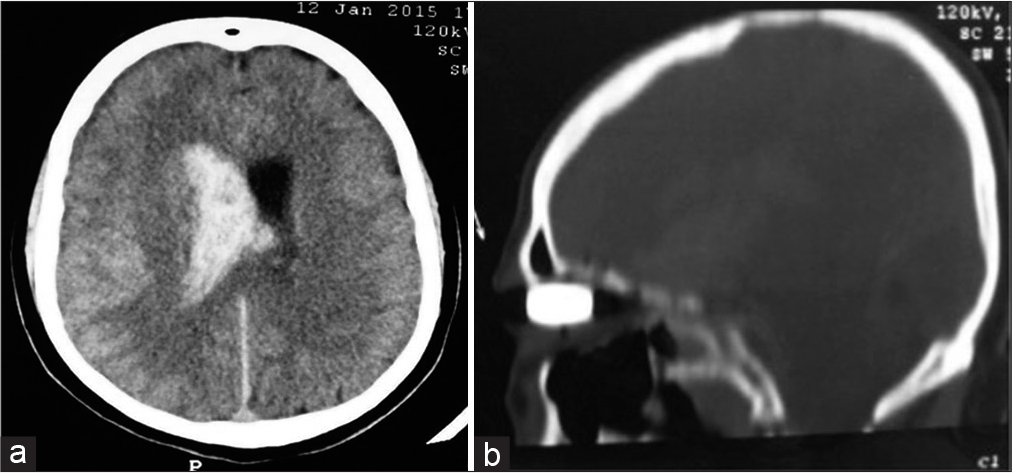
An otherwise healthy 34-year-old male presented with a loss of consciousness to the emergency department (ER). A gunshot wound entry was observed on his occiput with the right orbital swelling. His Glasgow Coma Scale (GCS) was 10 (E3, V3, M4), with a left-sided weakness grade of 3 on the Medical Research Council of Canada (MRC) scale. An ophthalmological examination was performed and revealed avulsed damaged globe. A head computed tomography (CT) scan was performed, which revealed a bullet lodged in the right orbit with an entrance point from the right occipital bone [
The patient is transferred to the operating room, where an interdisciplinary team of surgeons is prepared. The surgery was focused on three targets (1) hematoma evacuation, (2) scalp debridement, and (3) gentle bullet removal, which was performed successfully. The surgery went unremarkable. Furthermore, the postoperative course featured GCS 12 (E3, V4, M5) and a left-sided weakness MRC grade of 3. In the neurointensive care unit (ICU), measures were taken to decrease the intracranial pressure (ICP), including head elevation and mannitol boluses, according to the follow-up neurological examinations alone, as ICP monitoring is not available. In addition, essential care was performed, which included primary wound care and closure of both inlet and outlet in the neuro ICU. However, the patient died on the 7th day postoperatively, which mainly contributed to the patient’s TBI.
DISCUSSION
Penetrating brain injuries can be caused by a missile or non-missile mechanisms. Penetration of the missile is more common with high-velocity objects.[
Management of migratory fragments of penetrative bullets is still a subject of debate. Some authors recommend that bullets within the brain should be evacuated if accessible and if they can be removed without further neurological damage.[
Infectious complications caused by bullet migration induce a notable rise in morbidity and mortality rates. Local wound infections, meningitis, ventriculitis, and cerebral abscess are exceptionally high among these patients because contaminated foreign objects, skin, hair, and bone fragments were propelled along with bullets into the projectile track.[
Removal of the bullet in our case might have induced iatrogenic injury to the brain parenchyma. The expected complications are visual deterioration secondary to damage to the eyeball, cranial nerve palsies, severe infections such as meningitis and cerebral abscess, cerebral contusion and hematoma, and vascular lesions.[
The cranio-orbital versus orbitocranial trajectory of penetrating TBI may impact the planning of treatment and the priority in managing brain and eye injuries. In classic instances, the penetrating missile passes through the orbital, causing extensive injury to the eye globe with an inevitable vision violation. The ophthalmologist treats such injury at a later stage after stabilization of the neurological condition, and that treatment would include inoculation of the affected eye by implanting an artificial one. On the other hand, the next phase of injury entails a penetration to the retro-orbital parts of the cerebral hemisphere with a high risk of injury to the vascular bed at the base of the brain.
In the present scenario, the trajectory is cranio-orbital and opposite to the typical orbitocranial pathway, with the initial phase of injury affecting the brain and the eye representing a settling destination. This may result in less extensive orbital damage and more aggressive cerebral insult.
The unique direction of the bullet migration, in this case, sheds light on the proper considerations that should be accounted for to identify retrograde cranio-orbital penetrating injuries and encourage future studies to explore the different aspects of management and outcome in such cases and to prevent further complications.
CONCLUSION
Cranio-orbital penetrating brain injury is a severe yet rare type of penetrating brain injury usually associated with high-velocity objects such as bullets. The direction of cranio-orbital injury is usually from the orbital region to the cerebrum. In our case, the retrograde fashion of the bullet migration renders it unique and calls for further studies in the literature to highlight the differences in injury and management of such cases.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aarabi B, Alden TD, Maas AI, Narayan RK, Potapov AA, Salazar AM. Management and prognosis of penetrating brain injury. J Trauma Injury Infect Crit Care. 2001. 51: S1-85
2. Chibbaro S, Tacconi L. Orbito-cranial injuries caused by penetrating non-missile foreign bodies. Experience with eighteen patients. Acta Neurochirur (Wien). 2006. 148: 937-42 discussion 941-2
3. Duman H, Ziyal IM, Canpolat A. Spontaneous subfalcial transcallosal migration of a missile to the contralateral hemisphere causing deterioration in neurological status case-report. Neurol Med Chir (Tokyo). 2002. 42: 332-3
4. Estebanez G, Garavito D, López L, Ortiz J, Rubiano AM. Penetrating orbital-cranial injuries management in a limited resource hospital in Latin America. Craniomaxillofac Trauma Reconstr. 2015. 8: 356-62
5. Grant GA. Management of penetrating head injuries: Lessons learned. World Neurosurg. 2014. 82: 25-6
6. Milhorat TH, Elowitz EH, Johnson RW, Miller JI. Spontaneous movement of bullets in the brain. Neurosurgery. 1993. 32: 140-3
7. Nishio Y, Hayashi N, Hamada H, Hirashima Y, Endo S. A case of delayed brain abscess due to a retained intracranial wooden foreign body: A case report and review of the last 20 years. Acta Neuro Chir (Wien). 2004. 146: 847-50
8. Oh C, Lin J, Lettieri S. Traumatic cranio-orbital injury: Reconstruction using extraocular muscles. J Craniofac Surg. 2020. 1: e258-9
9. O’Neill OR, Gilliland G, Delashaw JB, Purtzer TJ. Transorbital penetrating head injury with a hunting arrow: Case report. Surg Neurol. 1994. 42: 494-7
10. Özkan Ü, Özateş M, Kemaloğlu S, Güzel A. Spontaneous migration of a bullet into the brain. Clin Neurol Neurosurg. 2006. 108: 573-5
11. Rapp LG, Arce CA, McKenzie R, Darmody WR, Guyot DR, Michael DB. Incidence of intracranial bullet fragment migration. Neurol Res. 1999. 21: 475-80
12. Rinaldi A, Gazzeri R, Conti L, Schiavone M, Cava M, Tirelli CC. Cranio-orbital missile wound and bullet migration. Case report. J Neurosurg Sci. 2000. 44: 107-12
13. Salama K, Choukry K, Negham H, Oukessou Y, Abada R, Mahtar M. A rare case of a penetrating cranio-facial foreign body stuck in the skull base. Int J Surg Case Rep. 2021. 81: 105721
14. Shuker ST. Management of transcranial orbital penetrating shrapnel/bullet war injuries. J Oral Maxillofac Surg. 2008. 66: 1927-31
15. Yeh S, Foroozan R. Orbital apex syndrome. Curr Opin Ophthalmol. 2004. 15: 490-8