- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
Correspondence Address:
Ha Son Nguyen
Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
DOI:10.4103/2152-7806.165173
Copyright: © 2015 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nguyen HS, Doan N, Eckardt G, Pollock G. Surgical decompression coupled with diagnostic dynamic intraoperative angiography for bow hunter's syndrome. Surg Neurol Int 14-Sep-2015;6:147
How to cite this URL: Nguyen HS, Doan N, Eckardt G, Pollock G. Surgical decompression coupled with diagnostic dynamic intraoperative angiography for bow hunter's syndrome. Surg Neurol Int 14-Sep-2015;6:147. Available from: http://surgicalneurologyint.com/surgicalint_articles/surgical-decompression-coupled-with-diagnostic-dynamic/
Abstract
Background:Bow hunter's syndrome, also known as rotational vertebrobasilar insufficiency, arises from mechanical compression of the vertebral artery during the neck rotation. Surgical options have been the mainstay treatment of choice. Postoperative imaging is typically used to assess adequate decompression. On the other hand, intraoperative assessment of decompression has been rarely reported.
Case Description:A 52-year-old male began to see “black spots,” and experienced presyncope whenever he rotated his head toward the right. The patient ultimately underwent a dynamic diagnostic cerebral angiogram, which revealed a dominant right vertebral artery and complete proximal occlusion of the right vertebral artery with the head rotated toward the right. Subsequently, the patient underwent an anterior transcervical approach to the right C6/C7 transverse process. The bone removal occurred along with the anterior wall of the C6 foramen transversarium, followed by the upper portion of the anterior C6 body medially, and the transverse process of C6 laterally. An oblique osseofibrous band was noted to extend across the vertebral artery; it was dissected and severed. An intraoperative cerebral angiogram confirmed no existing compression of the vertebral artery with the head rotated toward the right. The patient recovered from surgery without issues; he denied recurrence of preoperative symptoms at follow-up.
Conclusions:The authors report the third instance where intraoperative dynamic angiography was employed with good outcomes. Although intraoperative cerebral angiography is an invasive procedure, which prompts additional risks, the authors believe the modality affords better, real-time visualization of the vertebral artery, allowing for assessment of the adequacy of the decompression. This advantage may reduce the probability for a second procedure, which has its own set of risks, and may counteract the risks involved with intraoperative dynamic angiography.
Keywords: Bow hunter's syndrome, intraoperative angiography, surgical decompression
INTRODUCTION
Bow hunter's syndrome, also known as rotational vertebrobasilar insufficiency, arises from mechanical compression of the vertebral artery during neck rotation.[
CASE PRESENTATION
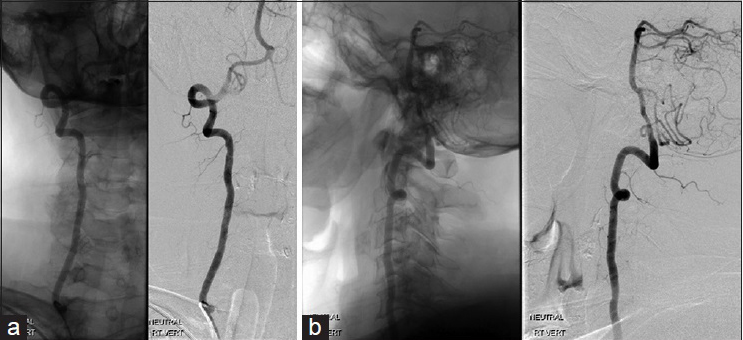
A 52-year-old male, with a history of multiple right shoulder surgeries, began to see “black spots” and experienced presyncope whenever he rotated his head toward the right. Moreover, he noted decreased sensation in the median nerve distribution on his right hand. He denied any vertigo, diplopia, or syncope. Given concerns for transient cerebral ischemia either as a consequence of a vertebral artery stenosis or a steal syndrome, a computed tomography angiography (CTA) head and neck was obtained, which revealed no significant stenosis of the right subclavian artery or vertebral artery. Magnetic resonance imaging (MRI) brain was unremarkable; MRI cervical spine exhibited multilevel degenerative disc disease without spinal canal narrowing. Subsequently, the patient underwent a dynamic cerebral angiogram, which revealed complete proximal occlusion of the right vertebral artery with the head turned toward the right [Figures
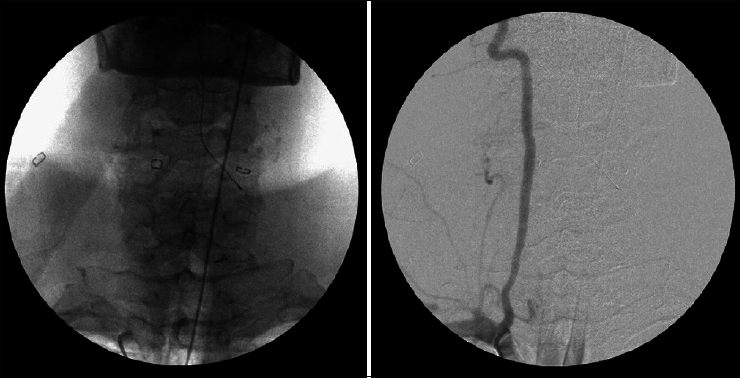
Decompression of the vertebral artery was recommended. An incision was made along the anterior border of the sternocleidomastoid muscle down to the suprasternal notch. The avascular plane medial to the border of the sternocleidomastoid muscle exposed. Dissection was carried down to the C6 transverse process after the division of the omohyoid muscle and the sternal head of the sternocleidomastoid muscle. The disk space at C6–C7 was confirmed with C-arm fluoroscopy. The longus colli muscle was detached from the vertebral body anteriorly, and the fascia overlying the longus colli was incised and reflected laterally in an attempt to protect the sympathetic chain, which was not visualized. The longus colli muscle was then incised over the C6 transverse process and reflected laterally, allowing for identification of the transverse foramen and the vertebral artery, which was confirmed by palpation and a micro-Doppler assessment.
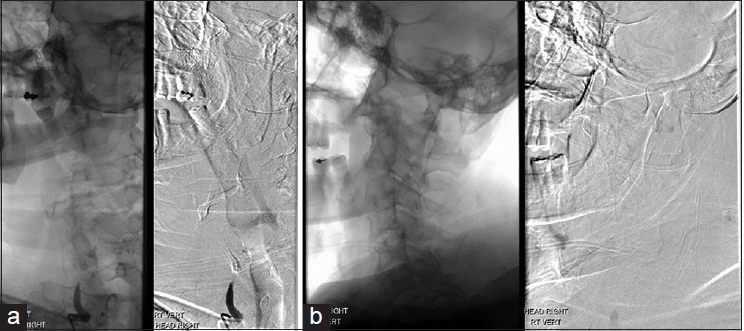
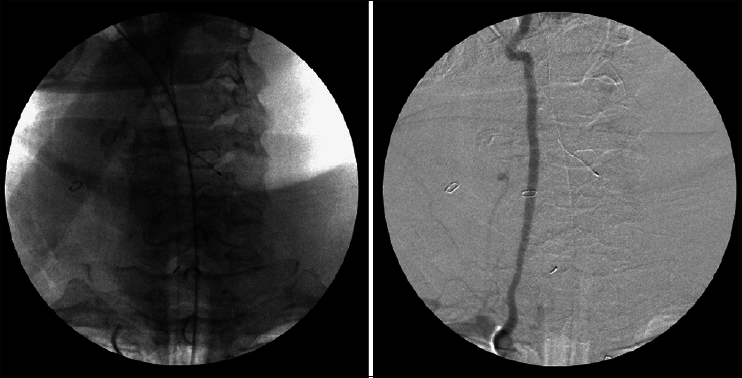
The bone removal occurred along with the anterior wall of the C6 foramen transversarium, followed by the upper portion of the anterior C6 body medially, and the transverse process of C6 laterally. This completed a 270° decompression of the foramen transversarium of C6. An oblique fibrous band was noted to extend across the vertebral artery in its anterior aspect superomedially to anterolaterally, starting at the level of the foramen transversarium of C6 and extending inferolaterally. The fibrous band was carefully dissected off the vertebral artery, and then severed using a 15 blade. An intraoperative cerebral angiogram initially imaged the right vertebral artery in neutral position [
DISCUSSION
More than half of the patients with bow hunter's syndrome present with syncope, while at least a third also exhibit vertigo, dizziness, and/or impaired vision.[
Intraoperative assessment of decompression has rarely been reported. In 2005, Vilela et al.[
Ding et al.[
CONCLUSION
The authors report the third instance where intraoperative dynamic angiography was employed with good outcomes. Noninvasive intraoperative modalities, including transcranial Doppler, Doppler ultrasonography directly on the vertebral artery, and fluorescent angiography have been discussed in the past. Although intraoperative cerebral angiography is an invasive procedure, which prompts additional risks, the authors believe the modality affords better, real-time visualization of the vertebral artery, allowing for assessment of the adequacy of the decompression. This advantage would guide further intraoperative surgical management of bow hunter's syndrome in one setting if needed, avoiding a second trip to operating room had the decompression found to be inadequate. Minimizing the probability for a second procedure, which has its own set of risks, might counteract the risks involved with intraoperative dynamic angiography.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anaizi AN, Sayah A, Berkowitz F, McGrail K. Bow hunter's syndrome: The use of dynamic magnetic resonance angiography and intraoperative fluorescent angiography. J Neurosurg Spine. 2014. 20: 71-4
2. Darkhabani MZ, Thompson MC, Lazzaro MA, Taqi MA, Zaidat OO. Vertebral artery stenting for the treatment of bow hunter's syndrome: Report of 4 cases. J Stroke Cerebrovasc Dis. 2012. 21: 908.e1-5
3. Ding D, Mehta GU, Medel R, Liu KC. Utility of intraoperative angiography during subaxial foramen transversarium decompression for bow hunter's syndrome. Interv Neuroradiol. 2013. 19: 240-4
4. Jost GF, Dailey AT. Bow hunter's syndrome revisited: 2 new cases and literature review of 124 cases. Neurosurg Focus. 2015. 38: E7-
5. Matsuyama T, Morimoto T, Sakaki T. Bow hunter's stroke caused by a nondominant vertebral artery occlusion: Case report. Neurosurgery. 1997. 41: 1393-5
6. Sugiu K, Agari T, Tokunaga K, Nishida A, Date I. Endovascular treatment for bow hunter's syndrome: Case report. Minim Invasive Neurosurg. 2009. 52: 193-5
7. Velat GJ, Reavey-Cantwell JF, Ulm AJ, Lewis SB. Intraoperative dynamic angiography to detect resolution of bow hunter's syndrome: Technical case report. Surg Neurol. 2006. 66: 420-3
8. Vilela MD, Goodkin R, Lundin DA, Newell DW. Rotational vertebrobasilar ischemia: Hemodynamic assessment and surgical treatment. Neurosurgery. 2005. 56: 36-43
9. Whitmore RG, Simon SL, Hurst RW, Nisenbaum HL, Kasner SE, Zager EL. Bow hunter's syndrome caused by accessory cervical ossification: Posterolateral decompression and the use of intraoperative Doppler ultrasonography. Surg Neurol. 2007. 67: 169-71