- Department of Neurosurgery, National Medical Center November 20 Institute of Security and Social Services of State Workers (ISSTE), Mexico City, Mexico.
Correspondence Address:
Francisco Castañeda Aguayo, Department of Neurosurgery, National Medical Center November 20 Institute of Security and Social Services of State Workers (ISSTE), Mexico City, Mexico.
DOI:10.25259/SNI_83_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Andres Jaime Aguirre, Francisco Castañeda Aguayo, Apolinar De la Luz Lagunas, Cuauhtemoc Gil Ortiz Mejia. Three cases of kyphoplasty performed in the lateral position due to significant comorbidities. 19-Apr-2024;15:138
How to cite this URL: Andres Jaime Aguirre, Francisco Castañeda Aguayo, Apolinar De la Luz Lagunas, Cuauhtemoc Gil Ortiz Mejia. Three cases of kyphoplasty performed in the lateral position due to significant comorbidities. 19-Apr-2024;15:138. Available from: https://surgicalneurologyint.com/surgicalint-articles/12862/
Abstract
Background: More than 700,000 people suffer from vertebral compression fractures attributed to osteoporosis, metastatic disease, or trauma each year in the United States, and undergo kyphoplasty. They are typical. These often undergo kyphoplasty to treat resultant pain or new neurological deficits. Here, we present three patients who, due to significant comorbidities, underwent kyphoplasty performed in the lateral decubitus rather than the prone position.
Case Description: Three females, two with metastatic cancer and one with osteoporosis, presented with lumbar compression fractures and new accompanying pain and/or neurological deficits. Due to significant accompanying comorbidities, kyphoplasty was safely and effectively performed in all three patients utilizing the lateral decubitus rather than the prone position.
Conclusion: Although vertebral kyphoplasties are typically performed in the prone position, here, we present three patients who, due to significant comorbidities, safely and effectively underwent kyphoplasties performed in the lateral decubitus position.
Keywords: Kyphoplasty, Lateral position, Osteoporosis, Vertebral fracture
INTRODUCTION
More than 700,000 people sustain vertebral compression fractures per year in the United States. They are typically due to osteoporosis, metastatic disease/osteolytic lesions, or trauma. Kyphoplasty is typically offered to treat resultant vertebral compression fractures. For patients with significant major comorbidities, including respiratory/compromise, kyphoplasty, rather than being performed in the prone position, may alternatively be safely and effectively performed in the lateral decubitus position.
CASE REPORTS
Case 1
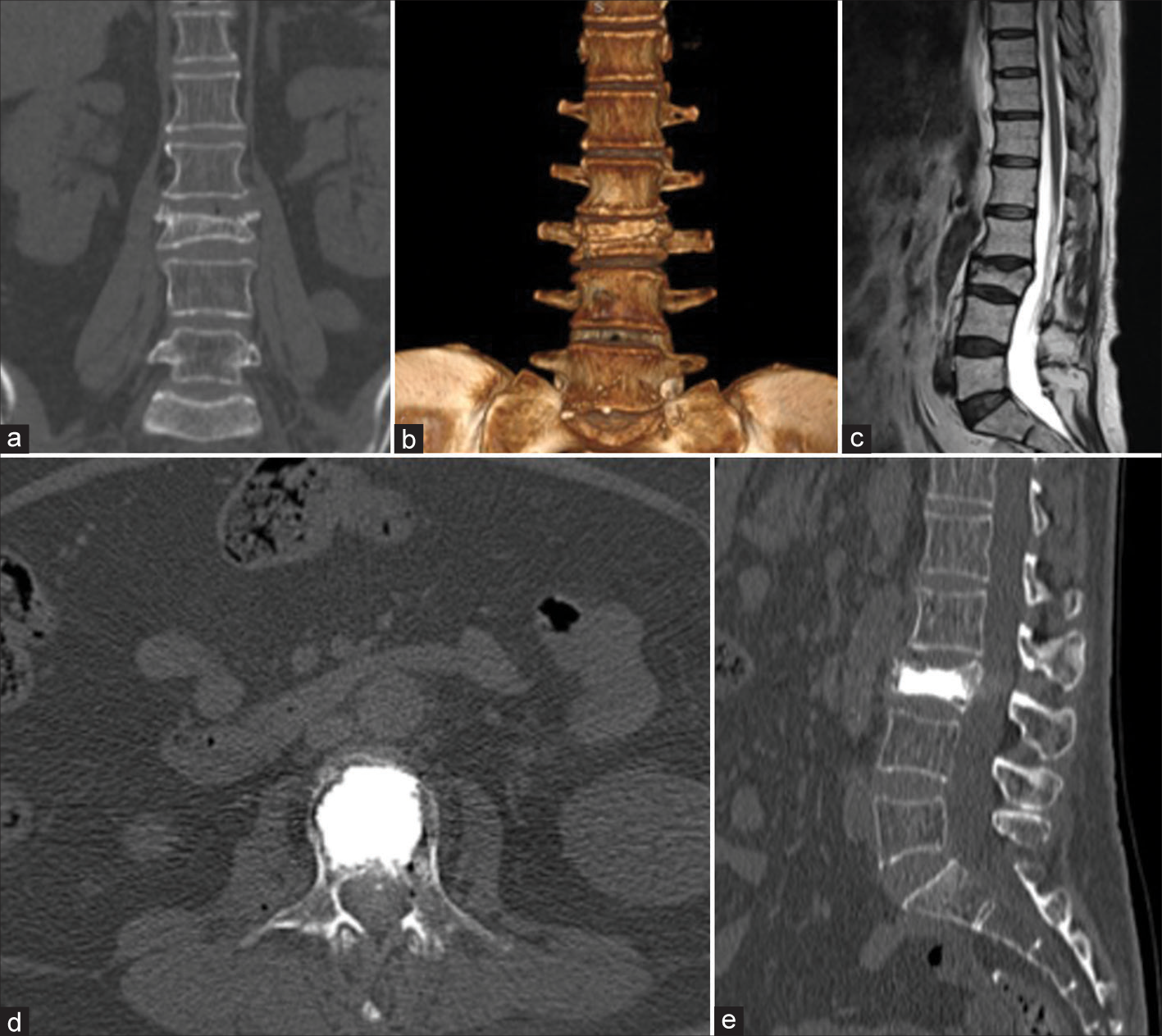
A 64-year-old female, following a fall, presented with bilateral L5 radiculopathy and bilateral L5 pathological vertebral compression fractures attributed to metastatic endometrial adenocarcinoma (i.e., previously managed with radiotherapy [
Figure 1:
Lumbar tomography in coronal view (a) and 3D reconstruction (b), lumbar MRI in T2 weighting (c), where a L3 vertebral compression fracture is observed. Lumbar tomography in axial (d) and sagittal (e) view after kyphoplasty, with the presence of hyperdensity in the body of L3 corresponding to cementation.
Case 2
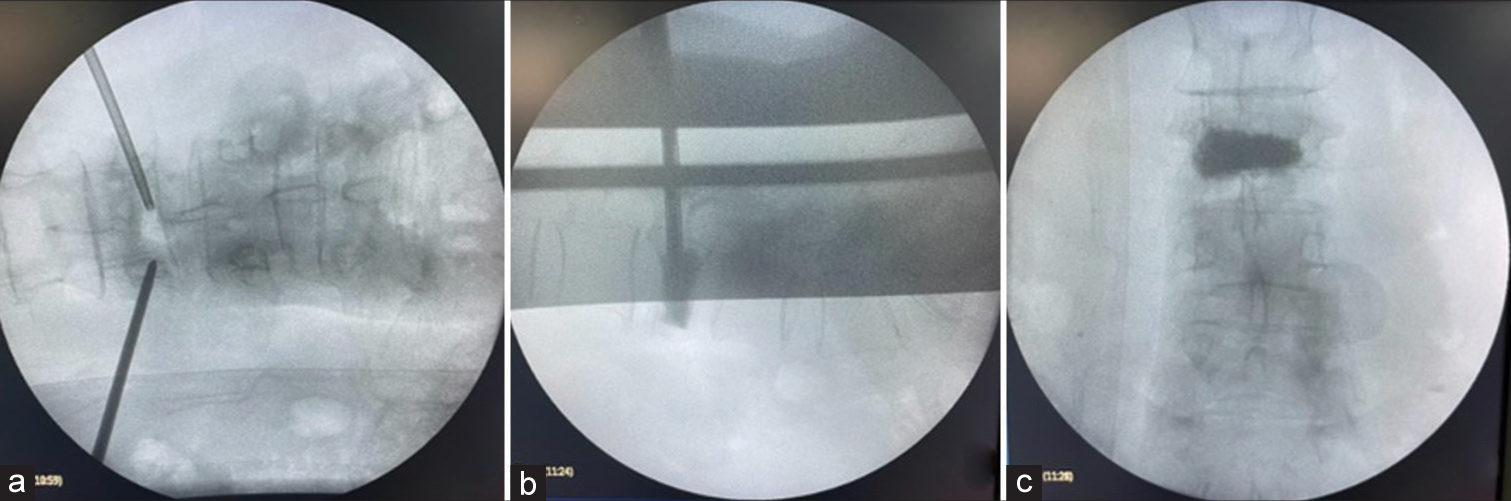
A 58-year-old female with a history of colon cancer (i.e., status postradiotherapy, surgery, and a secondary diverting colostomy) presented with lumbar pain (8/10). When the X-ray, computed tomography (CT), and magnetic resonance studies revealed a pathological L3 compression fracture, she successfully underwent a kyphoplasty performed in the lateral decubitus rather than prone position [
Figure 3:
Intraoperative fluoroscopy images, showing (a) AP X-ray with the presence of transpedicular cannulas, Subsequently, (b) lateral X-ray is observed during cement injection through the cannula in the vertebral body, Finally, (c) AP X-ray with the presence of intracorporeal cement at the end of the procedure and removal of cannulas.
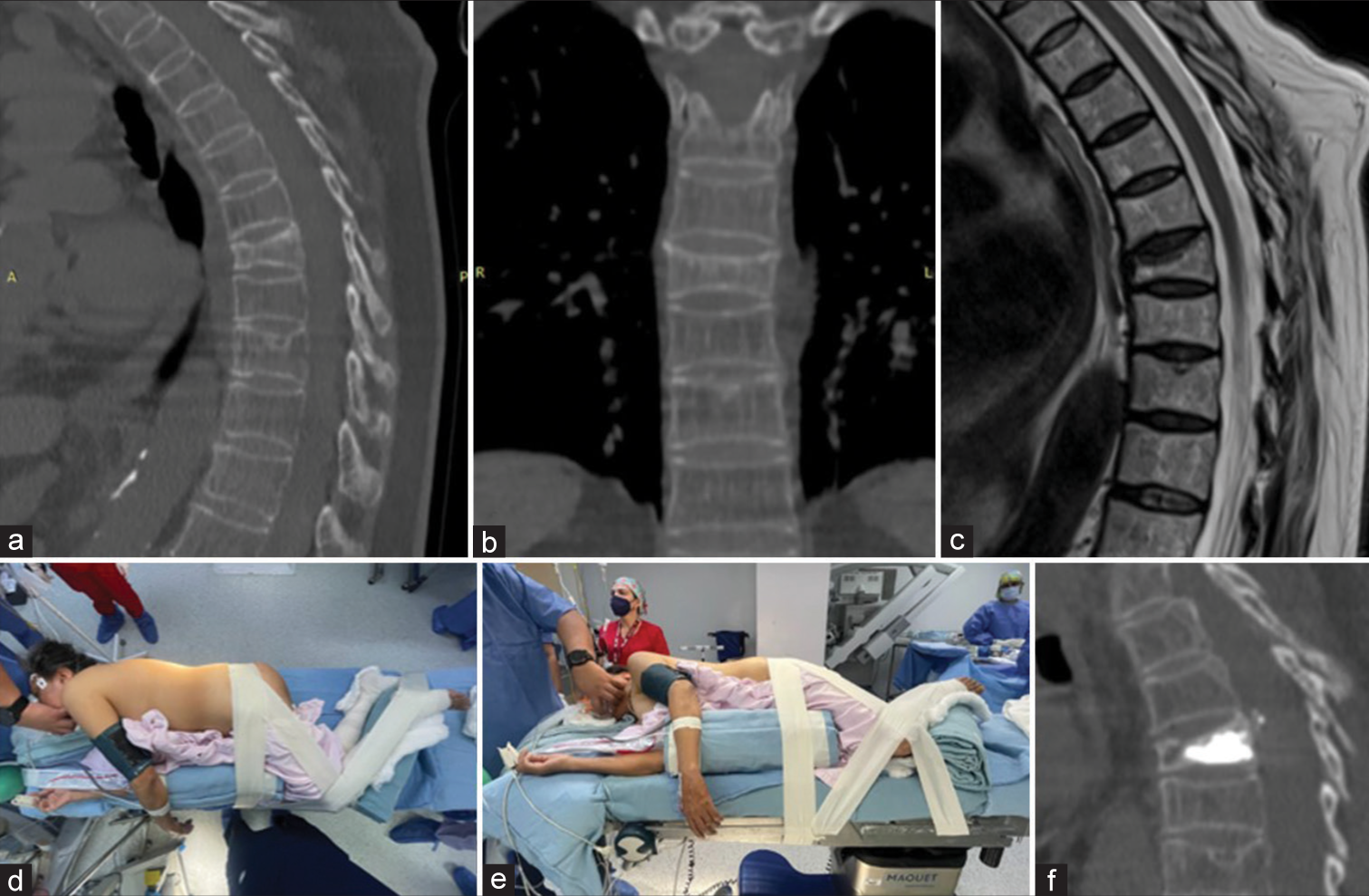
Case 3
A 62-year-old female with a history of osteoporosis treated with teriparatide presented with a 4-week history of falling from a height. When the CT scan revealed a T7 vertebral fracture, she successfully underwent a kyphoplasty performed in the lateral decubitus rather than prone position [
DISCUSSION
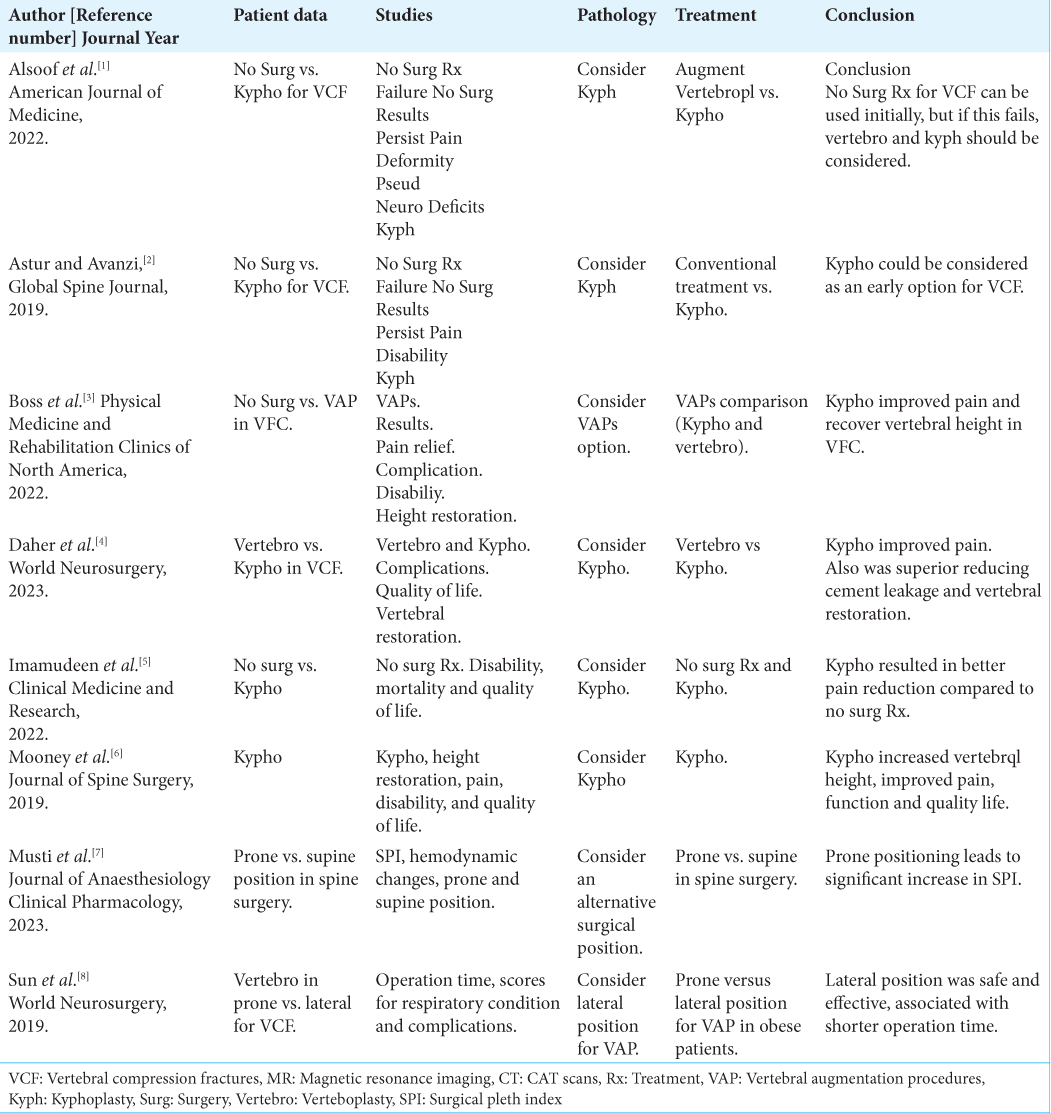
More than 700,000 people suffer from vertebral compression fractures each year in the U.S., and kyphoplasty could be recommended as an early treatment for this population.[
Advantages of kyphoplasty performed in the lateral decubitus position
Patients with significant comorbidities may safely/ effectively undergo kyphoplasty performed in the lateral decubitus versus the prone position. Advantages of this include reductions in the cardiac index/stroke volume and reduced left ventricular distention/venous return.[
CONCLUSION
The lateral decubitus position proved to be a safe and effective alternative for performing three kyphoplasties in patients with significant comorbidities and resultant vertebral compression fractures.
Ethical approval
The Institutional review board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
To the health authorities for their support in the management of patients in the neurosurgery service.
References
1. Alsoof D, Anderson G, McDonald CL, Basques B, Kuris E, Daniels AH. Diagnosis and management of vertebral compression fracture. Am J Med. 2022. 135: 815-21
2. Astur N, Avanzi O. Balloon kyphoplasty in the treatment of neoplastic spine lesions: A systematic review. Global Spine J. 2019. 9: 348-56
3. Boss S, Srivastava V, Anitescu M. Vertebroplasty and kyphoplasty. Phys Med Rehabil Clin N Am. 2022. 33: 425-53
4. Daher M, Kreichati G, Kharrat K, Sebaaly A. Vertebroplasty versus kyphoplasty in the treatment of osteoporotic vertebral compression fractures: A meta-analysis. World Neurosurg. 2023. 171: 65-71
5. Beall D, Lorio MP, Yun BM, Runa MJ, Ong KL, Warner CB. Review of vertebral augmentation: An updated meta-analysis of the effectiveness. Int J Spine Surg. 2018. 12: 295-321
6. Mooney JH, Amburgy J, Self M, Agee BS, Schoel L, Pritchard PR. Vertebral height restoration following kyphoplasty. J Spine Surg. 2019. 5: 194-200
7. Musti S, Chakrabarti D, Bansal S. The effect of prone positioning on surgical pleth index in patients undergoing spine surgery under general anesthesia-A prospective observational study. J Anaesthesiol Clin Pharmacol. 2023. 38: 646-51
8. Sun HB, Jing XS, Zhang GQ, Hai Y, Liu YZ, Wang DC. Preliminary study of obese patients with chronic obstructive pulmonary disease suffering from painful osteoporotic vertebral compression fracture treated by percutaneous vertebroplasty in improved prone position and right lateral position. World Neurosurg. 2019. 130: e933-40