Microsurgical treatment for cerebellomesencephalic fissure arteriovenous malformations after multiple sessions of endovascular treatment
Date of publication: 10-May-2021
Background: Arteriovenous malformations (AVMs) are relatively uncommon congenital vascular anomalies, and only 7–15% of AVMs occur in the posterior fossa. Most posterior fossa AVMs clinically present with hemorrhage and are associated with a high risk of neurological deficits and mortality. These malformations are associated with a high incidence of flow-related aneurysms. Endovascular treatment of infratentorial AVMs is challenging in pediatric patients.
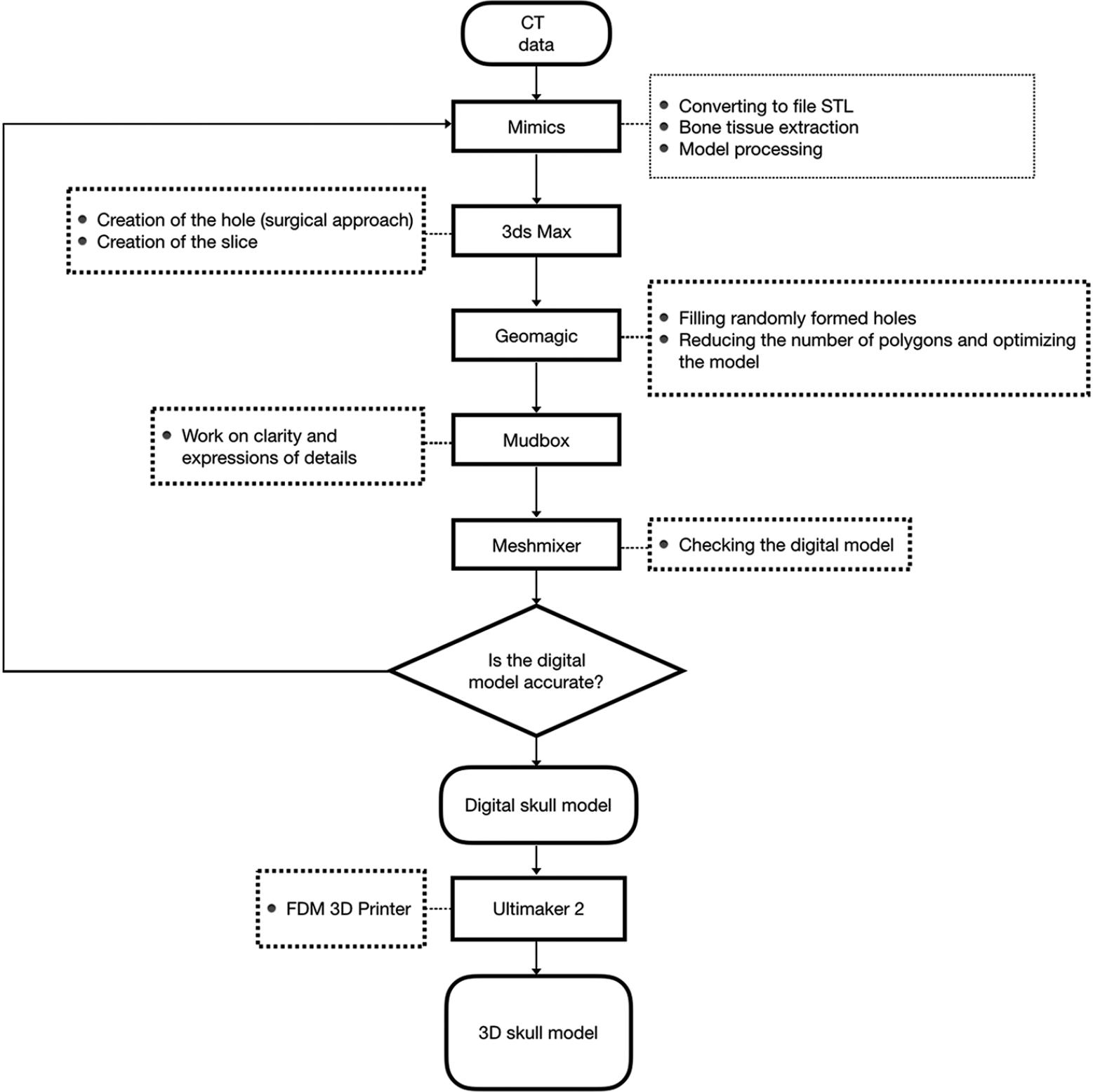
3D-printed cranial models simulating operative field depth for microvascular training in neurosurgery
Date of publication: 10-May-2021
Background: The skills required for neurosurgical operations using microsurgical techniques in a deep operating field are difficult to master in the operating room without risk to patients. Although there are many microsurgical training models, most do not use a skull model to simulate a deep field. To solve this problem, 3D models were created to provide increased training in the laboratory before the operating room, improving patient safety.
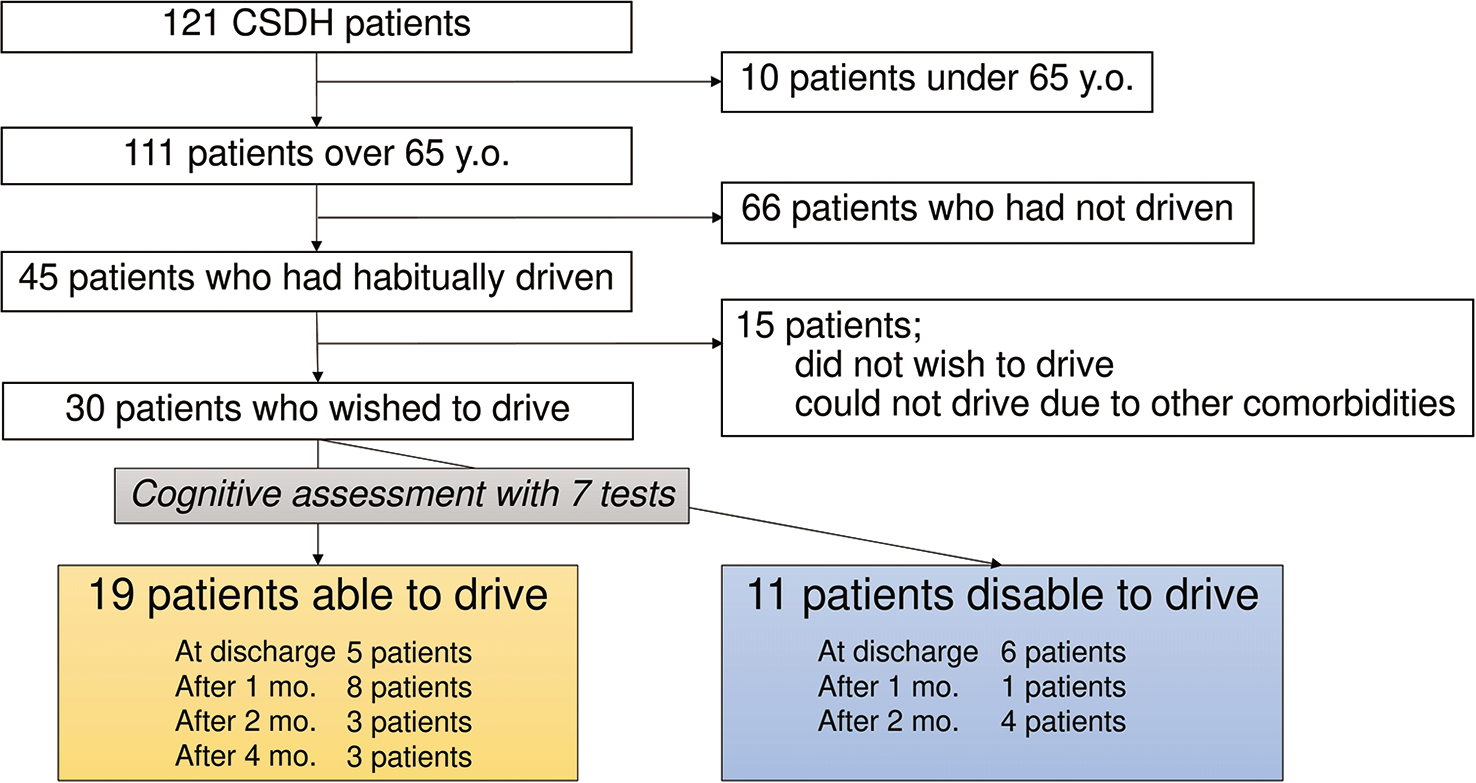
Chronic subdural hematoma in patients over 65 years old: Results of using a postoperative cognitive evaluation to determine whether to permit return to driving
Date of publication: 10-May-2021
Background: Chronic subdural hematoma (CSDH) is usually associated with good recovery with burr hole irrigation and postoperative drainage under local anesthesia. In Japan, traffic accidents by the elderly drivers over 65 years old are severely increasing, and there is no consensus on whether or not to return to driving after CSDH treatment. We perform a postoperative cognitive assessment. We retrospectively investigated the return-to-driving rate and associated factors.
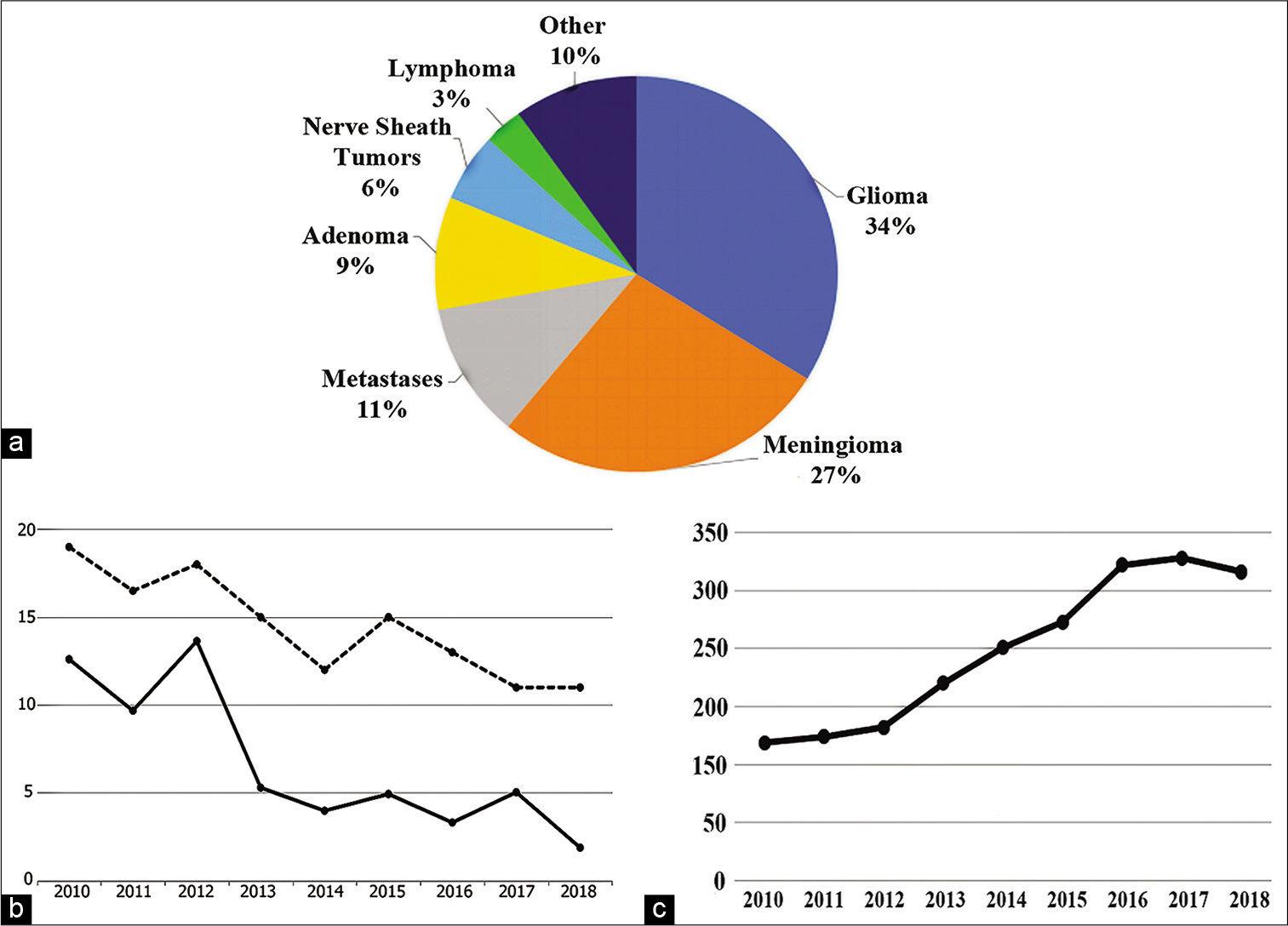
Trends in hospital stay and outcome of CNS tumor patients in Greece during the socioeconomic crisis period (2010–2018): The case of the academic neurosurgical department at Evangelismos Hospital
Date of publication: 03-May-2021
Targeting gut dysbiosis as a means to enhance recovery from surgical brain injury
Date of publication: 03-May-2021
Background: Surgical brain injury (SBI) impacts roughly 800,000 people who undergo neurosurgical procedures each year. SBI is the result of unavoidable parenchymal damage, vessel disruption, and thermal injury that is an inherent part of all neurosurgical procedures. Clinically, SBI has been associated with postoperative seizures and long-term neurobehavioral deficits. Current therapies are aimed at providing symptom relief by reducing swelling and preventing seizures. However, there are no therapies aimed at reducing the extent of SBI preoperatively. The microbiome-gut-brain axis may serve as a potential target for the development of new preventative therapies due to its extensive involvement in central nervous system function.
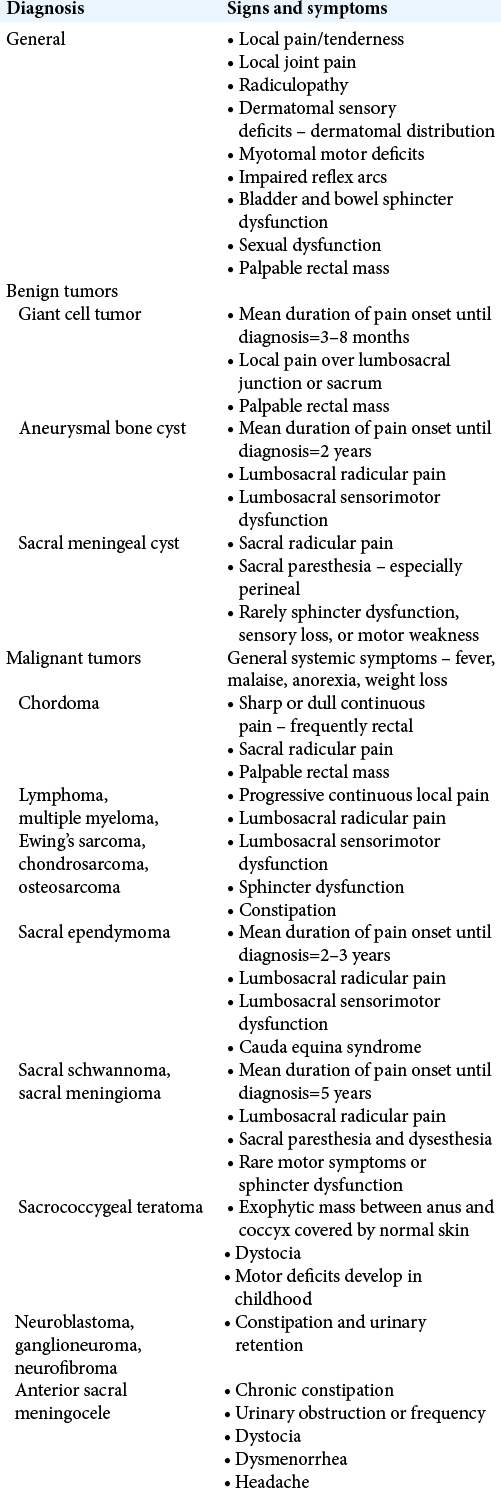
Clinical manifestations, classification, and surgical management of sacral tumors and the need for personalized approach to sacrectomy
Date of publication: 03-May-2021
Background: Although comprising 7% of all spinal tumors, sacral tumors present with a litany of issues due to their slow growth and difficulty in detection. As a result, sacral tumors can grow unperturbed for years until a patient presents for an incidental workup of an unassociated minor trauma or an offending primary tumor source that has metastasized to the sacrum; in most cases, this includes primary tumors of the breast, prostate, and lung. The goal of this review is to outline the pathophysiology underlying sacral tumors including the various tissues and structures that can be targeted for treatment, along with a discussion of the surgical approach to sacrectomy.
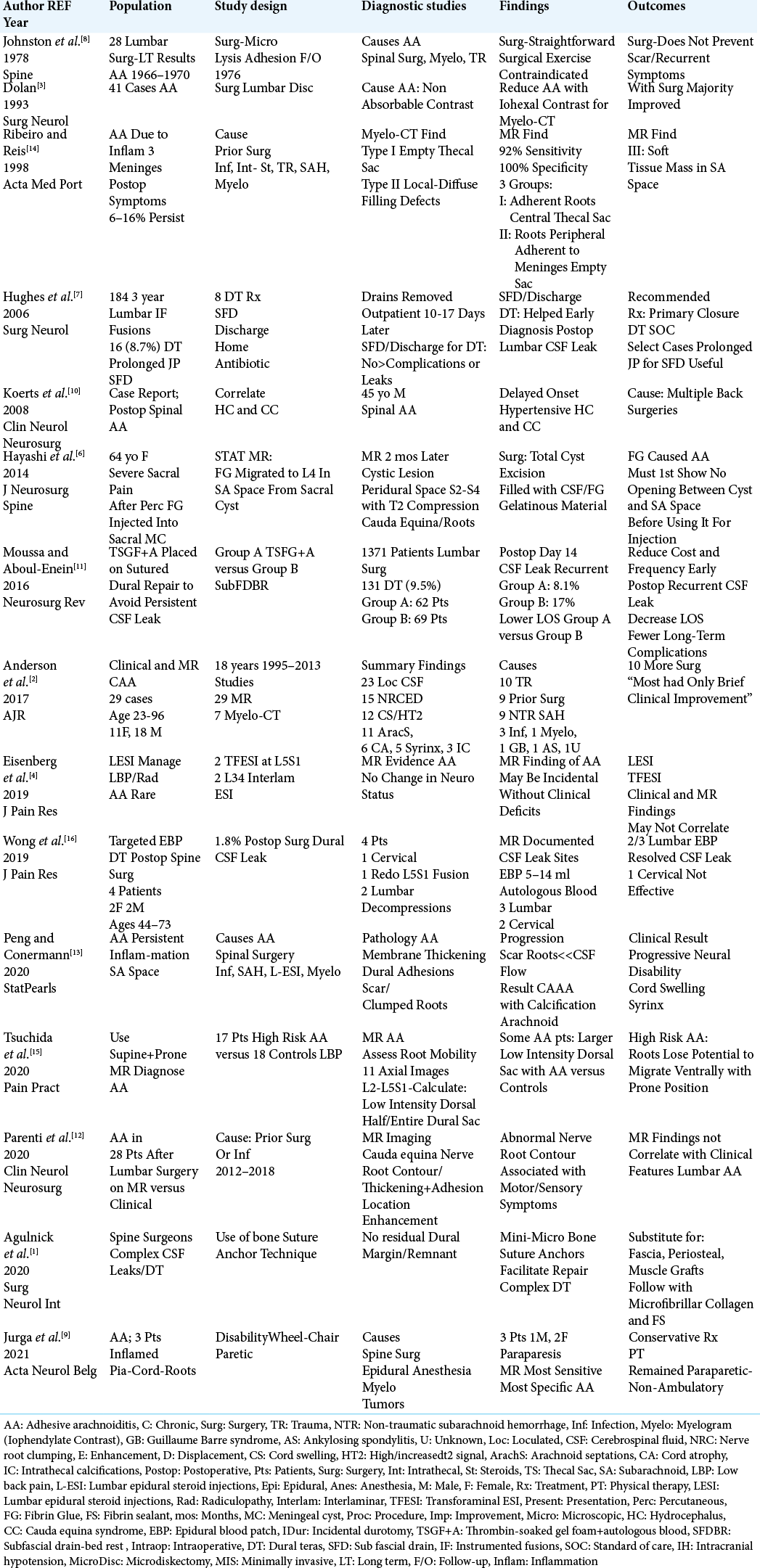
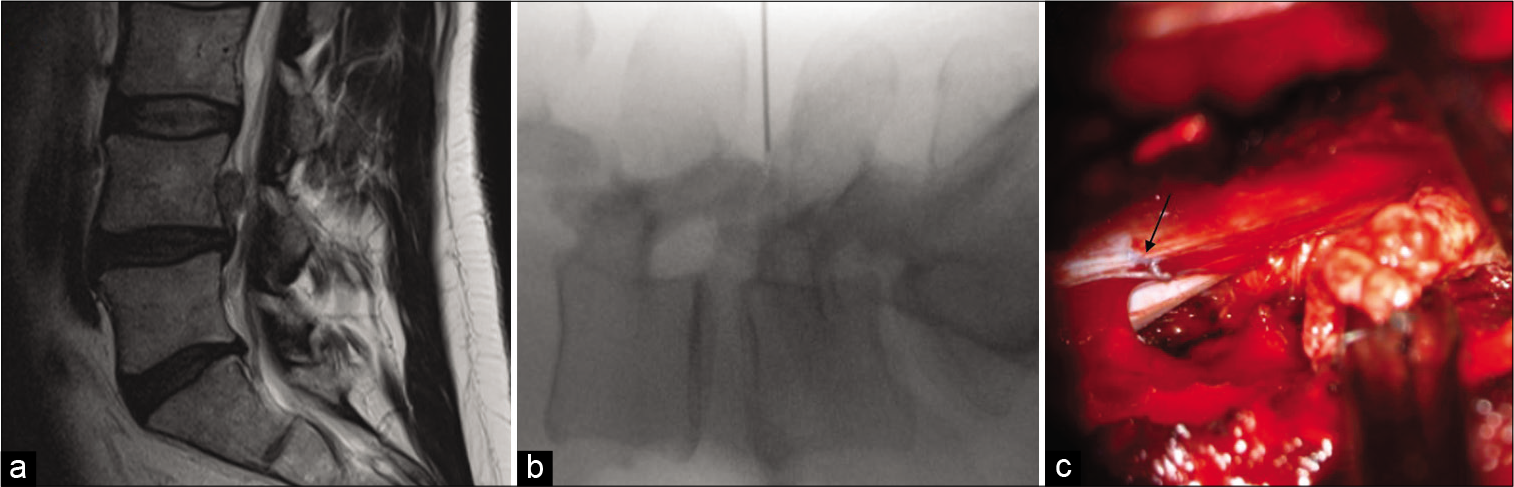
Perspective: Early diagnosis and treatment of postoperative recurrent cerebrospinal fluid fistulas/ dural tears to avoid adhesive arachnoiditis
Date of publication: 03-May-2021
Background: Intraoperative traumatic cerebrospinal fluid (CSF) fistulas/dural tears (DT) occur in up to 8.7–9.5% of primary lumbar surgical procedures. Further, they recur secondarily in between 8.1% and 17% of cases. It is critical to diagnose and treat these recurrent lumbar DT early (i.e. within 3–4 weeks of the index surgery) to avoid the evolution of adhesive arachnoiditis (AA), and its’ permanent neurological sequelae.
MEDICOLEGAL CORNER. Failure to replace obstructed lumbar drain after thoracic-abdominal aortic aneurysm repair leads to paraplegia
Date of publication: 03-May-2021
Background: To avoid spinal cord ischemia following endovascular/open thoracic-abdominal aortic aneurysm (T-AAA) repair, lumbar drains (LDs) are placed to reduce intraspinal pressure, and increase spinal perfusion pressure. Here, we present a medicolegal case in which a critical care (CC) physician knew that the LD was obstructed following a T-AAA repair, but did not replace it until the patient became paraplegic. The patient was left with permanent sphincter loss, and a severe paraparesis.
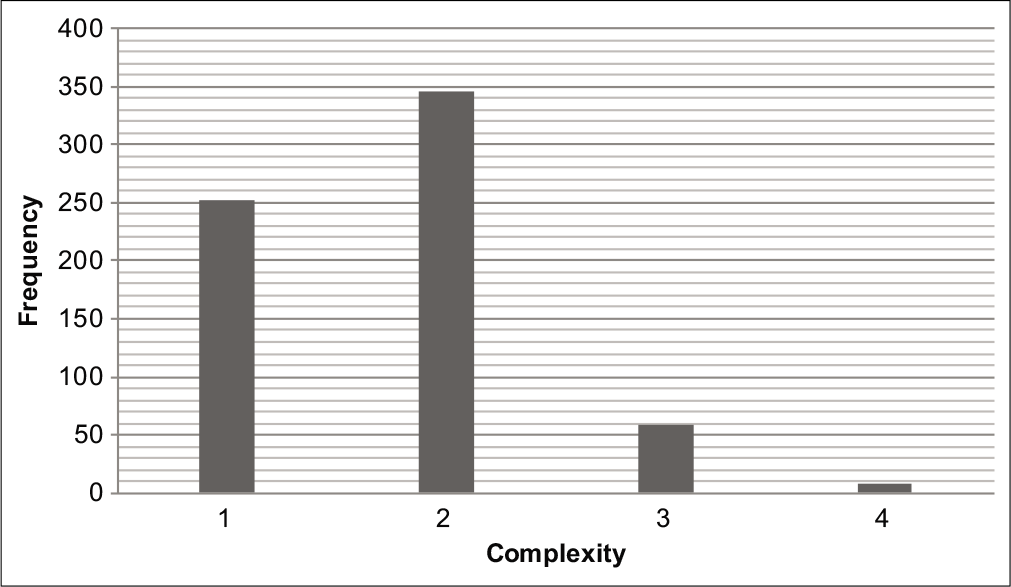
Spine surgery complexity score predicts outcomes in 671 consecutive spine surgery patients
Date of publication: 03-May-2021
Background: The spine surgery complexity score (SSCS), previously reported by us, is a simple grading system to predict postoperative complications and hospital length of stay (LOS). This scale is based on the technical difficulty of the spinal procedures being performed.
Dural leakage due to ipsilateral needle placement for spinal level localization in unilateral decompression surgery: A case report
Date of publication: 03-May-2021
Background: A spinal dural defect caused by needle placement for spinal level localization is an uncommon complication of cerebrospinal fluid leak with the potential for the development of intracranial hypertension.