Single-session percutaneous embolization with onyx and coils of sinus pericranii
Date of publication: 04-Jun-2018
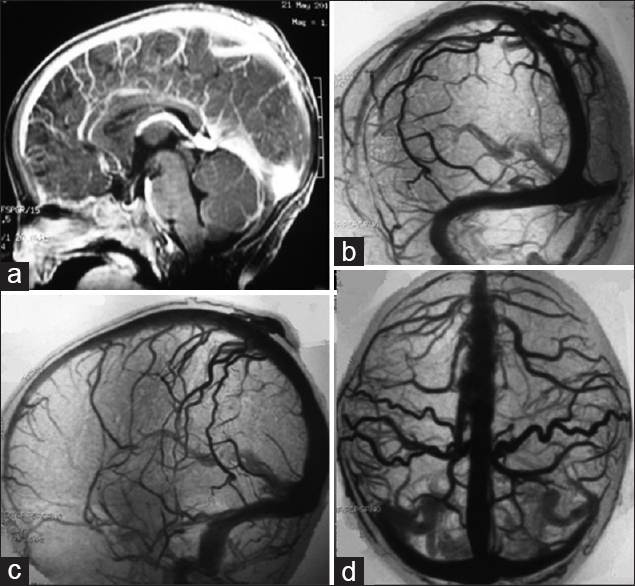
Background:Sinus pericranii (SP) is a rare vascular malformation consisting of an abnormal communication between the extra- and the intracranial venous system. It occurs due to the adhesion of vessels without a muscular layer or a hemangioma on the outer surface of the skull through diploic vessels, communicating with an intracranial venous sinus.
Management of autonomic dysreflexia associated with Charcot spinal arthropathy in a patient with complete spinal cord injury: Case report and review of the literature
Date of publication: 29-May-2018
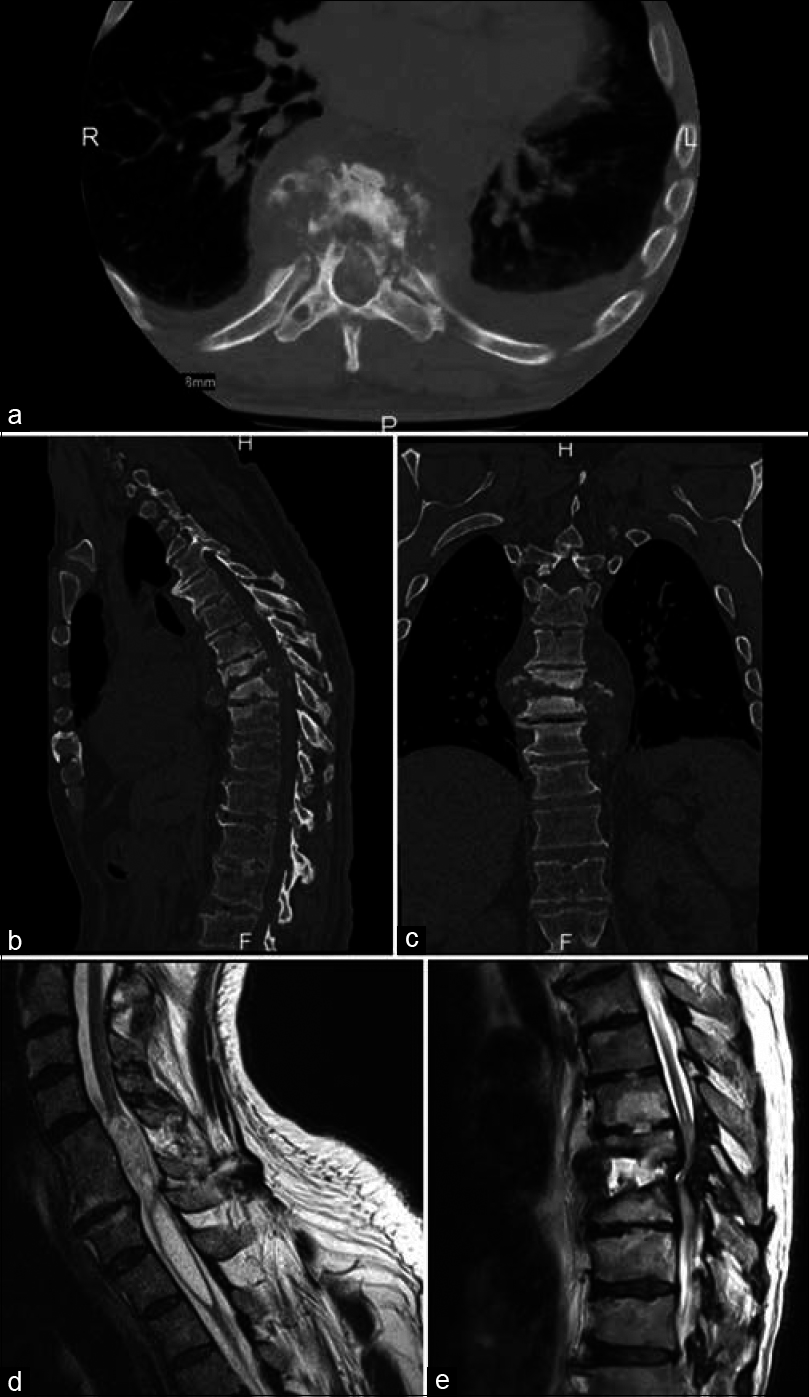
Background:Charcot spinal arthropathy (CSA) clearly represents a challenge in long-term spinal cord injury patients, one that can have extremely uncomfortable and potentially lethal outcomes if not managed properly.
The role of radiosurgery in the acute management of fourth ventricle compression due to brain metastases
Date of publication: 29-May-2018
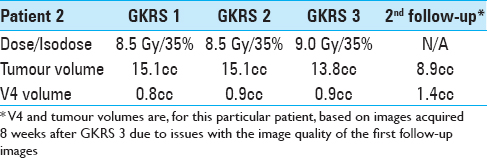
Background:Approximately 20–30% of all intracranial metastases are located in the posterior fossa. The clinical evolution hinges on factors such as tumor growth dynamics, local topographic conditions, performance status, and prompt intervention. Fourth ventricle (V4) compression with secondary life-threatening obstructive hydrocephalus remains a major concern, often requiring acute surgical intervention. We have previously reported on the application of adaptive hypofractionated Gamma Knife Radiosurgery in the acute management of critically located metastases, a technique known to us as rapid rescue radiosurgery (3R). We report the results of 3R in the management of posterior fossa lesions and ensuing V4 decompression.
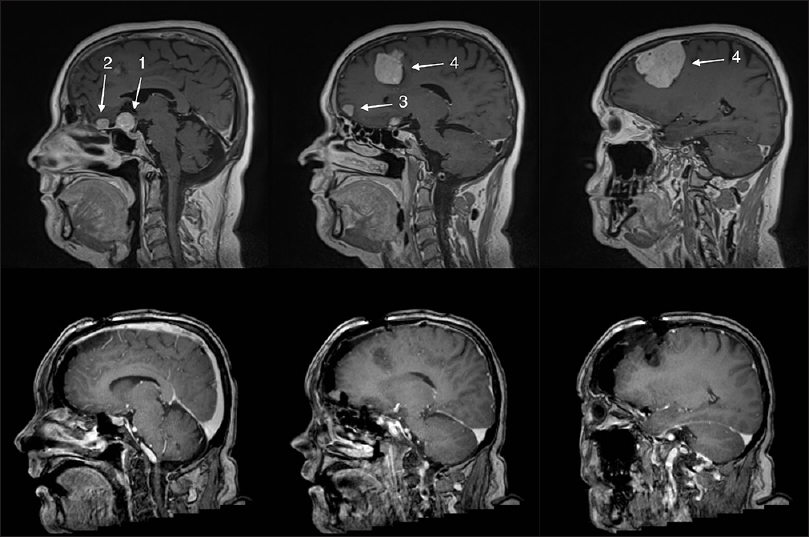
Giant parieto-occipital lobe pediatric gliosarcoma: Report of a rare entity and review of literature
Date of publication: 29-May-2018
Background:Gliosarcoma is a rare high-grade malignant tumor and a variant of glioblastoma characterized by biphasic glial and mesenchymal components. Gliosarcomas occur most commonly in the fifth or sixth decade of life and have a temporal lobe predilection. Occurrence in the pediatric population is extremely rare.
Primary diffuse large B-cell lymphoma of the choroid plexus: A case report and review of the literature
Date of publication: 25-May-2018
Background:Primary lymphomas in the choroid plexus are much less frequent than primary lymphomas in the brain parenchyma.
Multiple meningiomas in two male-to-female transsexual patients with hormone replacement therapy: A report of two cases and a brief literature review
Date of publication: 25-May-2018
Background:Exogenous sex hormones may play a role in meningioma development and growth. Thus, transsexual patients being on long-standing hormone replacement therapy (HRT) may be at particular risk for meningioma development and growth. Here we present two cases of two male-to-female transsexual patients taking HRT for an extended period of time with both patients requiring surgical treatment at our institution due to multiple growing meningiomas.
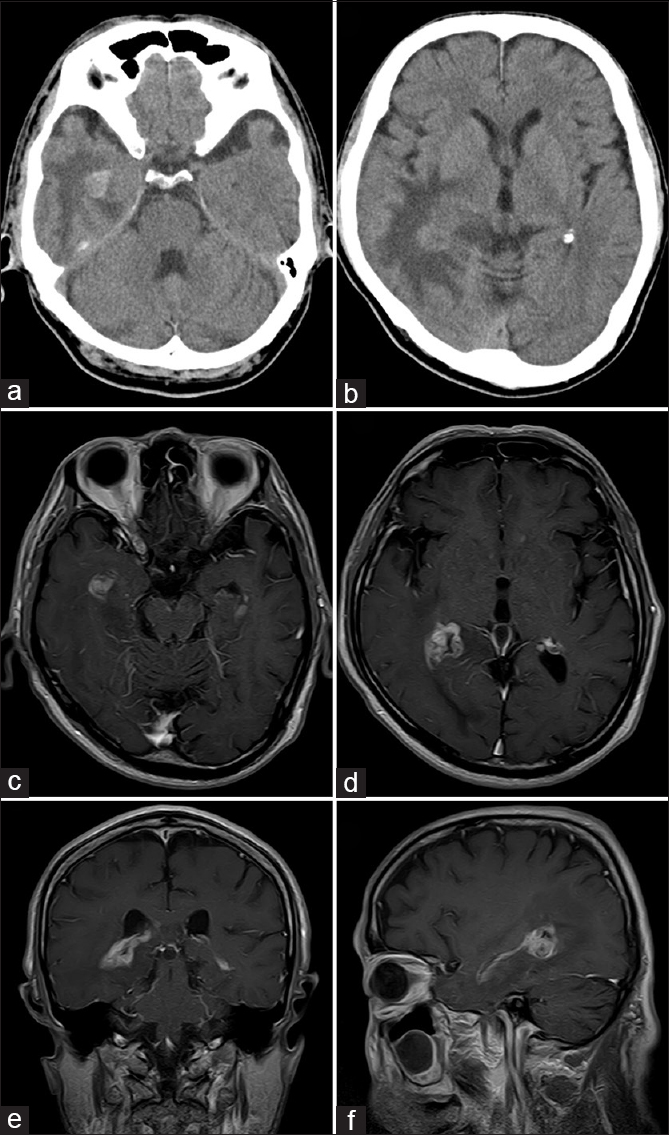
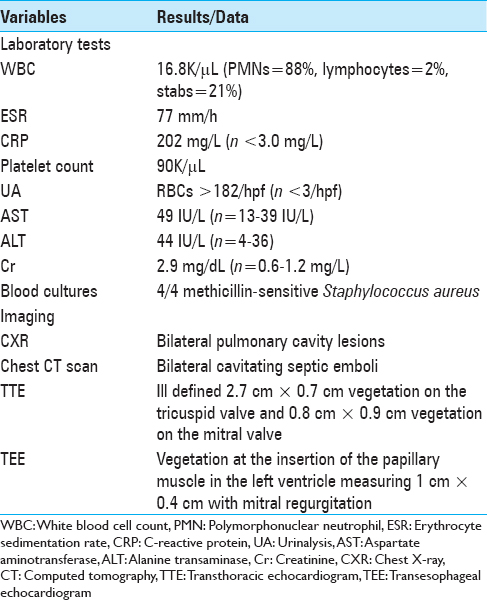
Intracranial complications of acute bacterial endocarditis
Date of publication: 25-May-2018
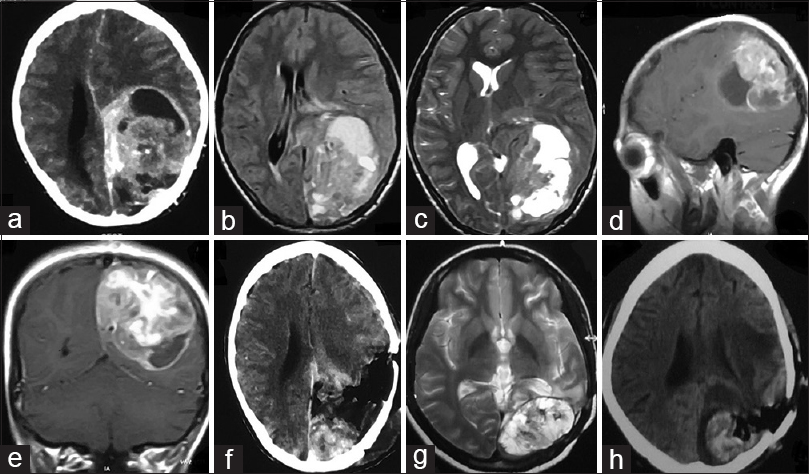
Background:Infectious endocarditis (IE) clinically manifests as either subacute bacterial endocarditis (SBE) or acute bacterial endocarditis (ABE). Neurologic manifestations are markedly different for these two entities. ABE is caused by invasive, highly virulent pathogens (e.g., Staphylococcus aureus), whereas SBE is attributed to relatively avirulent, non-invasive organisms (e.g., viridans streptococci).
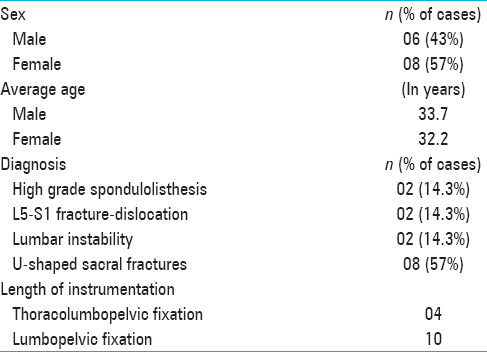
Fluoroscopy only for the placement of long iliac screws: A study on 14 patients
Date of publication: 25-May-2018
Background:Iliac screw placement is challenging due to the particular anatomy of the ilium. Most series have reported the use of relatively short (≤90 mm in length) screws despite a long iliac buttress, which has an average length of 129 mm in females and 141 mm in males. This study describes a series of 14 patients who underwent placement of long iliac screws (≥100 mm in length) as part of a spinopelvic fusion utilizing fluoroscopy alone.
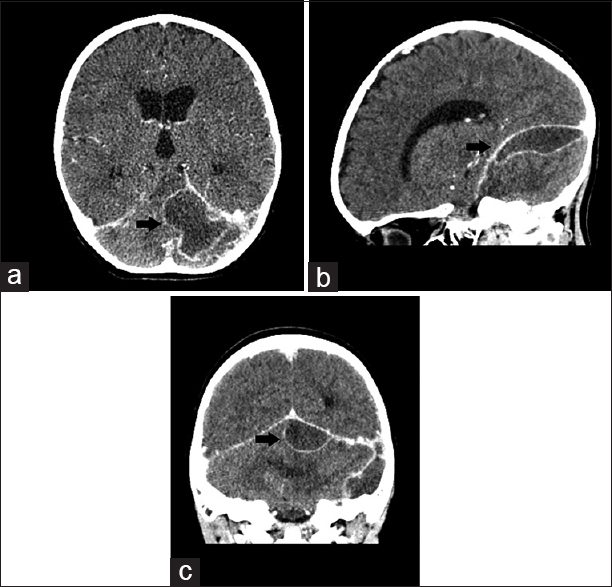
Pediatric infratentorial subdural empyema: A case report
Date of publication: 24-May-2018
Background:Infratentorial subdural empyemas in children are extremely rare and potentially lethal intracranial infections. Delay in diagnosis and therapy is associated with increased morbidity and mortality.
A review of the diagnosis and management of vertebral basilar (posterior) circulation disease
Date of publication: 24-May-2018
Abstract
We have reviewed the English literature published in the last 70 years on Diseases of the Vertebral Basilar Circulation, or Posterior Circulation Disease (PCD). We have found that errors have been made in the conduct and interpretation of these studies that have led to incorrect approaches to the management of PCD. Because of the difficulty in evaluating the PC, the management of PCD has been incorrectly applied from anterior circulation disease (ACD) experience to PCD. PCD is a common form of stroke affecting 20-40% patients with stroke. Yet, the evidence is strong that the Anterior Circulation (AC) and Posterior Circulations (PC) differ in their pathology, in their clinical presentations, in the rapidity of development of symptoms, in optimal imaging methods, and in available treatments.
There appears to be two categories of patients who present with PCD. The first, acute basilar artery occlusion has a more rapid onset. The diagnosis must be made quickly and if imaging proves a diagnosis of Basilar Artery Occlusion (BAO), the treatment of choice is Interventional removal of the basilar artery thrombosis or embolus. The second category of PCD and the most commonly seen PCD disease process presents with non-specific symptoms and early warnings of PCD that now can be related to ischemic events in the entire PC vessels. These warning symptoms and signs occur much earlier than those in the AC.
IA angiography is still the gold standard of diagnosis and is superior in definition to MR and CT angiography which are commonly used as a convenient screening imaging tool to evaluate PCD but are both inferior to IA angiography in definition for lesions below 3-4 mm. In at least two reported studies 7T MR angiography appears superior to other imaging modalities and will become the gold standard of imaging of PCD in the future. Medical treatments applied to the ACD have not been proven of value in specific forms of PCD. Interventional therapy was promising but of unproven value in Randomized Controlled Trials (RCT) except for the treatment of Basilar Artery Occlusion (BAO).
Surgical revascularization has been proved to be highly successful in patients, who are refractory to medical therapy. These studies have been ignored by the scientific community basically because of an incorrect interpretation of the flawed EC-IC Bypass Trial in 1985 as applying to all stroke patients. Moreover, the EC-IC Bypass Study did not include PCD patients in their study population, but the study results were extrapolated to patients with PCD without any scientific basis. This experience led clinicians to an incorrect bias that surgical treatments are of no value in PCD. Thus, incorrectly, surgical treatments of PCD have not been considered among the therapeutic possibilities for PCD.
QMRA is a new quantitative MR technique that measures specific blood flow in extra and intracranial vessels. QMRA has been used to select those patients who may benefit from medical, or interventional, or surgical treatment for PCD based on flow determinations with a high success rate. QMRA accurately predicts the flows in many large and small vessels in the PC and AC and clearly indicates that both circulations are intimately related.
From medical and surgical studies, the longer one waits for surgical treatment the higher the risk of a poor outcome results. This observation becomes obvious when the rapidity of development of PCD is compared with ACD. Recent advances in endovascular therapy in the treatment of acute basilar thrombosis is a clear sign that early diagnosis and treatment of PCD will reduce the morbidity and mortality of these diseases.
In this review it is evident that there are multiple medical and surgical treatments for PCD depending upon the location of the lesion(s) and the collateral circulation demonstrated. It is clear that the AC and PC have significant differences. With the exception of the large population studies from Oxford England, the reported studies on the management of PCD in the literature represent small selected subsets of the universe of PC diseases, the information from which is not generalizable to the universe of PCD patients. At this point in the history of PCD, there are not large enough databases of similar patients to provide a basis for valid randomized studies, with the exception of the surgical studies. Thus, a high index of suspicion of the early warning symptoms of PCD should lead to a rapid individual clinical assessment of patients selecting those with PCD. Medical, interventional, and/or surgical treatments should be chosen based on knowledge presented in this review. Recording the results in a national Registry on a continuing basis will provide the data that may help advance the management of PCD based on larger data bases of well documented patient information to guide the selection of future therapies for PCD treatments. It is also clear that the management of patients within the complex of diseases that comprise PCD should be performed in centers with expertise in the imaging, medical, interventional and surgical approaches to diseases of the PCD.