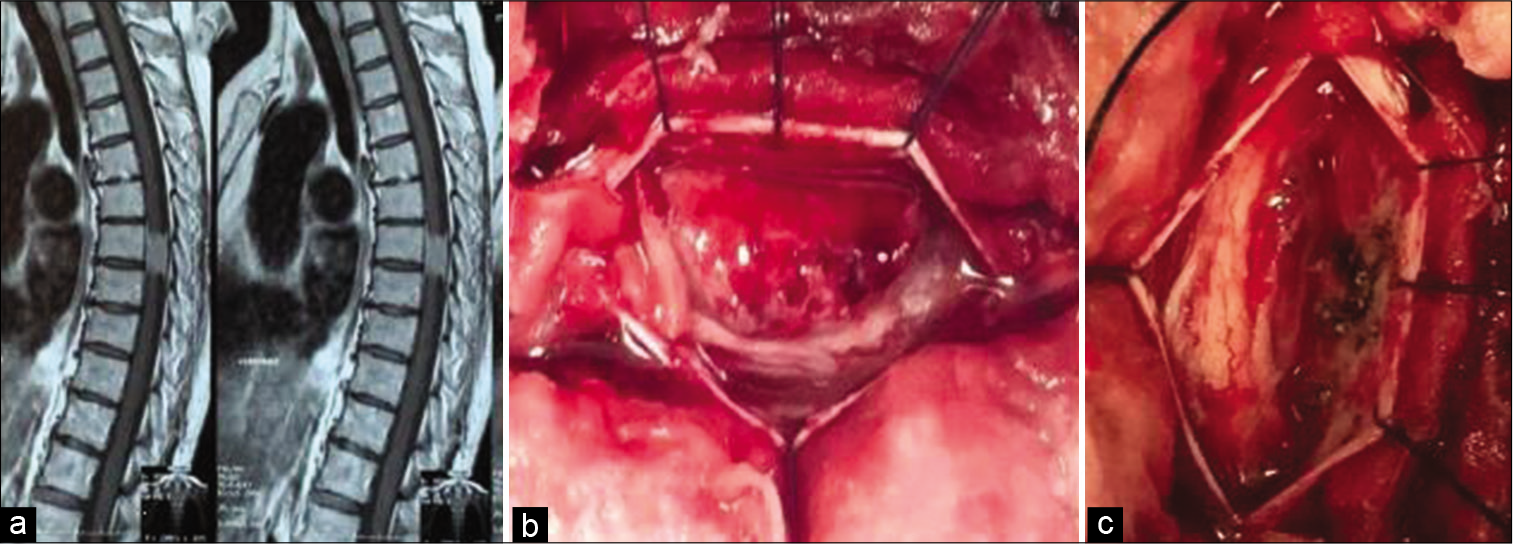
Delayed recovery from paraplegia following resections of thoracic meningiomas
Date of publication: 02-Oct-2020
Background: In this retrospective study, we evaluated the patterns of postoperative recovery for patients who were initially paraplegic before the excision of thoracic spine meningiomas. We also determined how the various prognostic factors impacted outcomes.
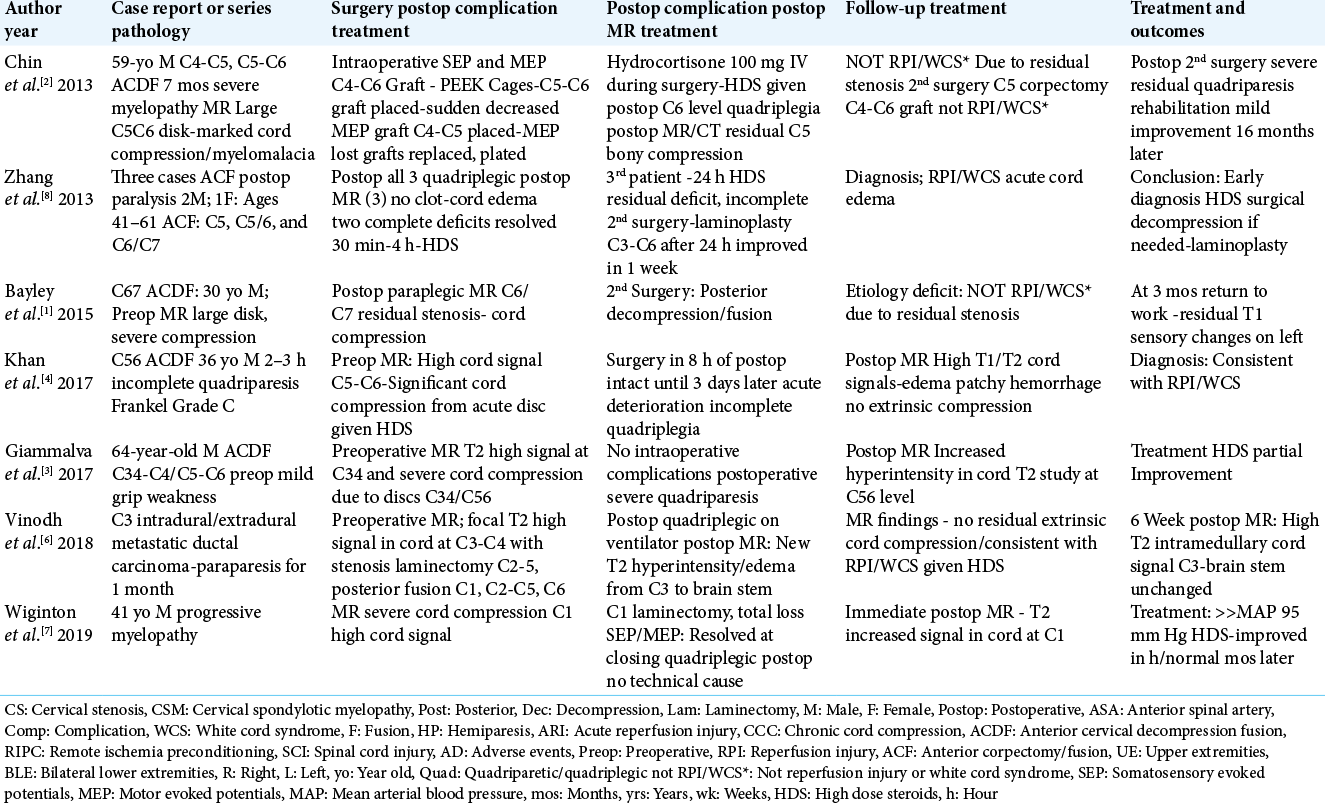
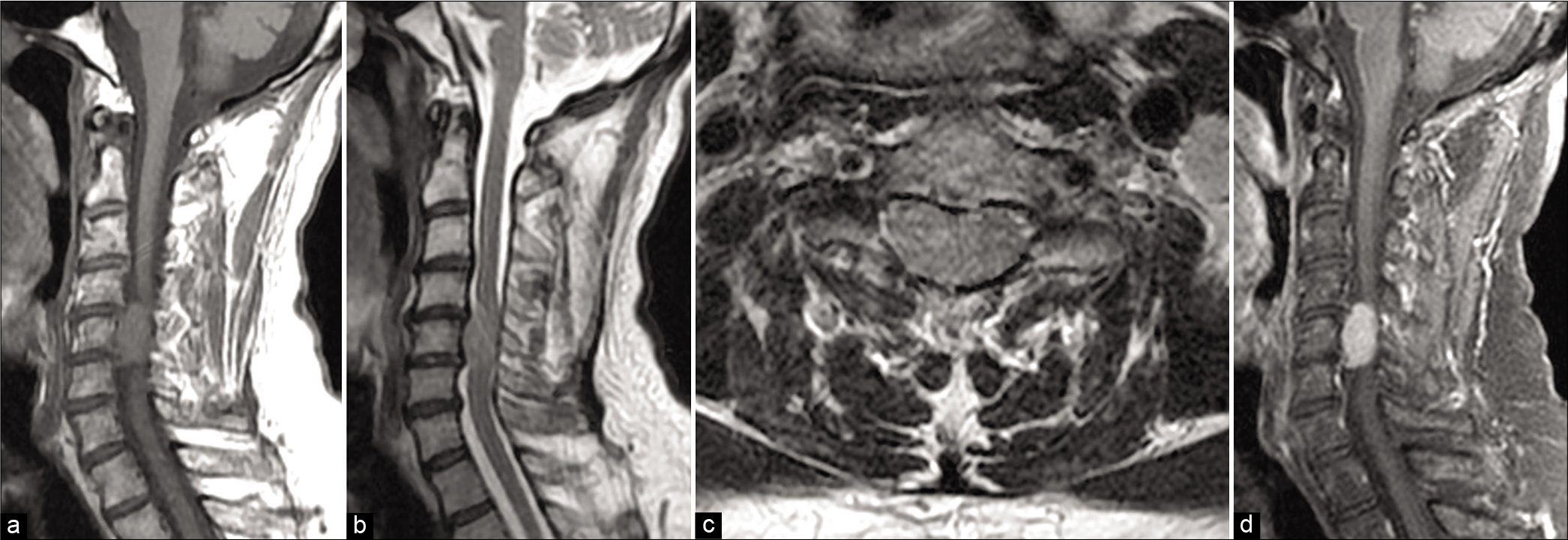
Reperfusion Injury (RPI)/White Cord Syndrome (WCS) Due to Cervical Spine Surgery: A Diagnosis of Exclusion
Date of publication: 02-Oct-2020
Background: Following acute cervical spinal cord decompression, a subset of patients may develop acute postoperative paralysis due to Reperfusion Injury (RPI)/White Cord Syndrome (WCS). Pathophysiologically, this occurs due to the immediate restoration of normal blood flow to previously markedly compressed, and under-perfused/ischemic cord tissues. On emergent postoperative MR scans, the classical findings for RPI/ WCS include new or expanded, and focal or diffuse intramedullary hyperintense cord signals consistent with edema/ischemia, swelling, and/or intrinsic hematoma. To confirm RPI/WCS, MR studies must exclude extrinsic cord pathology (e.g. extramedullary hematomas, new/residual compressive disease, new graft/vertebral fracture etc.) that may warrant additional cervical surgery to avoid permanent neurological sequelae.
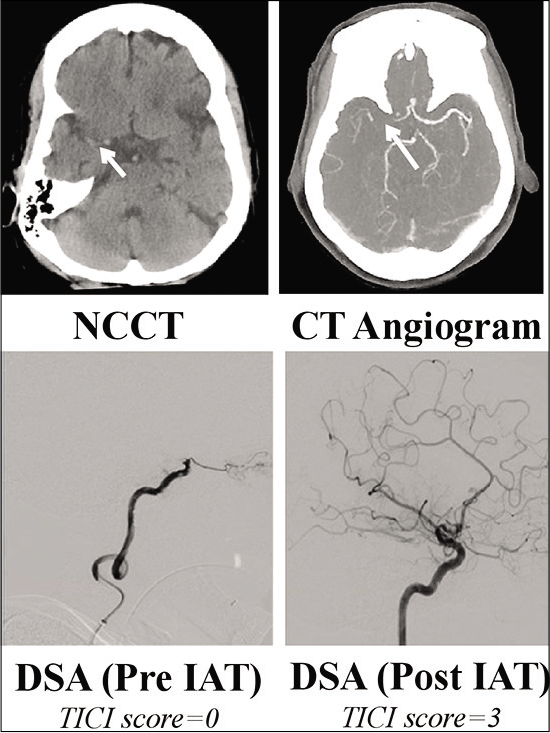
Brain abscess – A rare complication of endovascular treatment for acute ischemic stroke
Date of publication: 02-Oct-2020
Background: Brain abscess is a neurosurgical emergency, which can arise through direct bacterial seeding or hematogenous spread. Rarely, brain abscess formation has been reported following ischemic stroke. An increasingly utilized therapy for stroke is mechanical thrombectomy, and within this report, we present a case of brain abscess formation following this procedure.
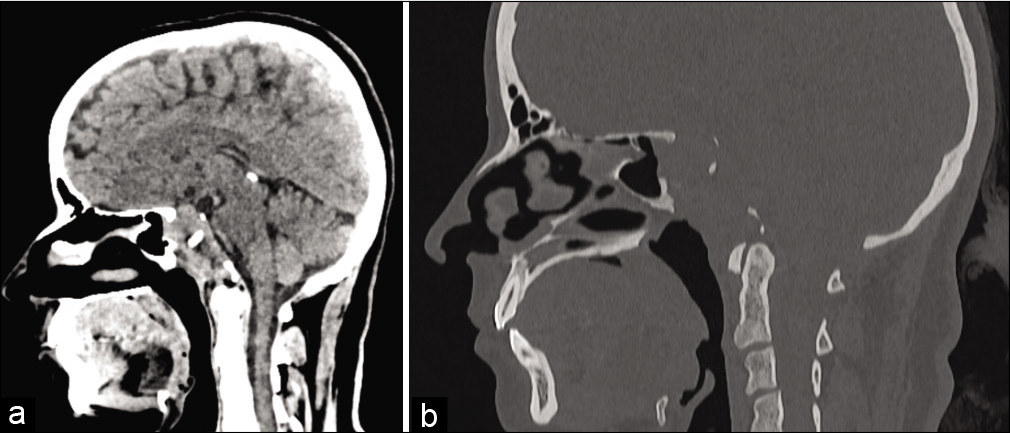
Aspergillus masquerading as clival chordoma
Date of publication: 02-Oct-2020
Cervical meningioma resection including the inner dura through an open-door laminoplasty using hydroxyapatite spacers: A case report
Date of publication: 02-Oct-2020
Background: The ideal surgery for spinal cord tumors is complete resection to prevent recurrence. However, it should be accomplished safely/effectively without risking increased morbidity. Here, we report a cervical meningioma that was totally resected, including the inner dura, through a laminoplasty performed with hydroxyapatite (HA) spacers.
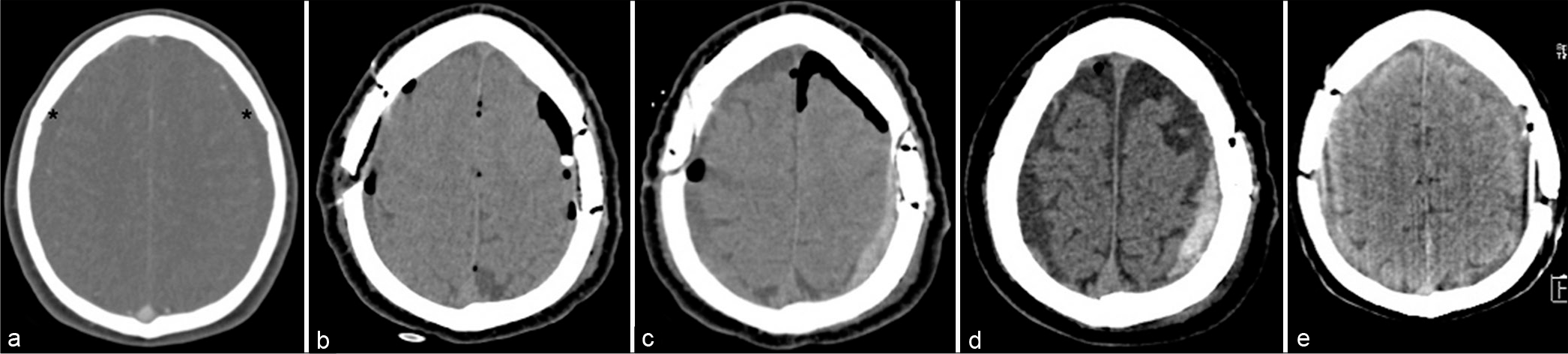
Acute subdural hematoma recurrence during drain removal associated with spontaneous intracranial hypotension – A non-reported complication
Date of publication: 02-Oct-2020
Background: Spontaneous intracranial hypotension (SIH) is an uncommon, benign, and generally self-limiting condition caused by low cerebrospinal fluid (CSF) volume and pressure usually caused by a CSF leak. Patients with SIH have an increased incidence of subdural hematomas (SDH), which may be bilateral and recurrent.
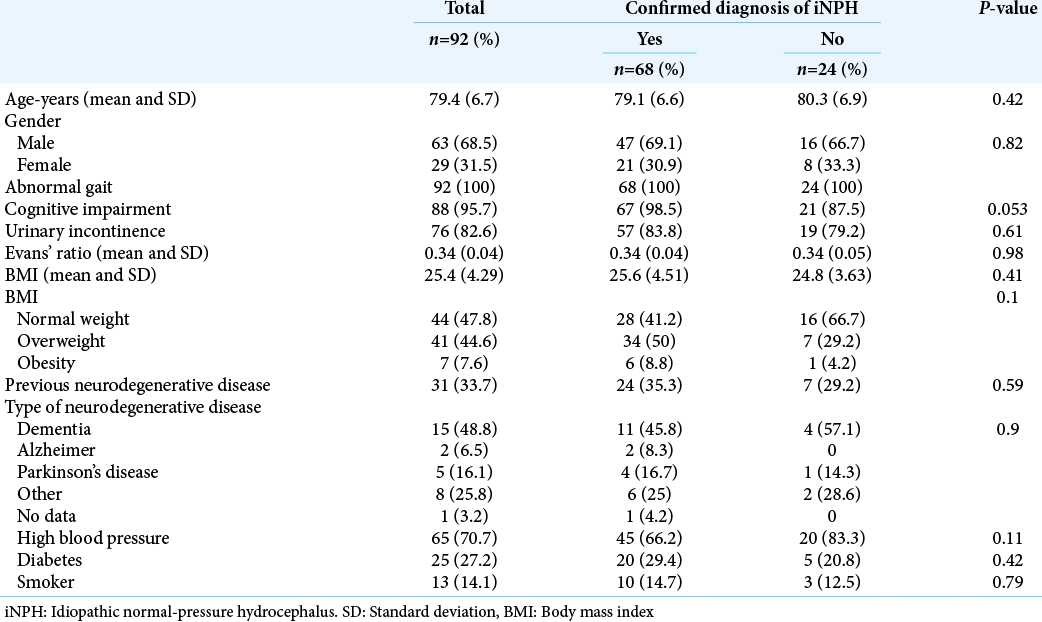
Cerebrospinal fluid closing pressure-guided tap test for the diagnosis of idiopathic normal pressure hydrocephalus: A descriptive cross-sectional study
Date of publication: 02-Oct-2020
Background: Tap test improves symptoms of idiopathic normal pressure hydrocephalus (iNPH); hence, it is widely used as a diagnostic procedure. However, it has a low sensitivity and there is no consensus on the parameters that should be used nor the volume to be extracted. We propose draining cerebrospinal fluid (CSF) during tap test until a closing pressure of 0 cm H2O is reached as a standard practice. We use this method with all our patients at our clinic.
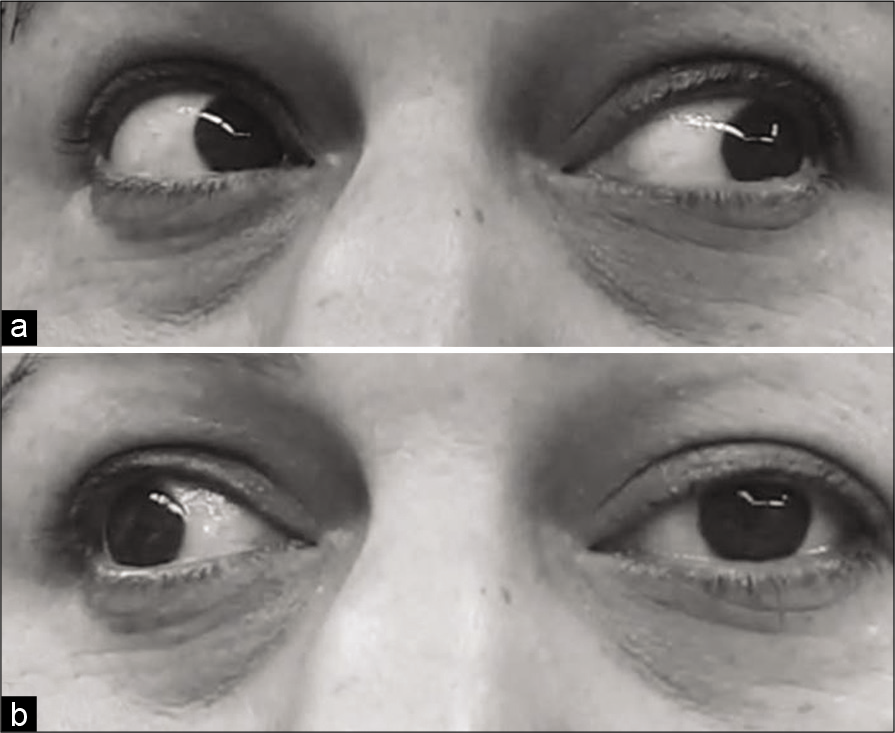
Meningothelial meningioma of the oculomotor nerve: A case report and review of the literature
Date of publication: 02-Oct-2020
Background: The origin of meningioma tumors is known as the meningothelial or arachnoid cap cells. The arachnoid granulations or villi are concentrated along with the dural venous sinuses in the cerebral convexity, parasagittally, and sphenoid wing regions. The majority of meningiomas are found in these locations with dural attachment. Infrequently, meningiomas develop without dural attachment but in dural adjacent. There are numerous reports of patients with cranial nerve involvement as a result of the compressive effect of the sinus cavernous or adjacent structures meningioma tumor on the cranial nerve.
Rapidly growing diffuse neurofibroma of the scalp with calvarial defect in a young woman: A rare entity
Date of publication: 02-Oct-2020
Background: A diffuse neurofibroma, a variant of neurofibroma, most commonly occurs in young adults and involves the head and neck. In the absence of neurofibromatosis, associated calvarial defect with these swellings is rarely seen.
Case Report (Precis): Patient with MR-Documented Large Lateral Cervical Disc Misdiagnosed as Neurodegenerative Disease
Date of publication: 25-Sep-2020
Background: Patients who present to neurologists with cervical radiculopathy typically undergo initial MR scans. If reports show “abnormal” findings they, and other physicians, should review the studies with the interpreting radiologists/neuroradiologists. When patients’ neurological deficits progress, neurologists should review their electromyographic (EMG) findings (i.e. especially if documenting neurodegenerative disease), the initial “abnormal” MR scans/reports (i.e. review with radiologists/neuroradiologists), and obtain spinal surgical consultations to rule out “surgical” disease.